Congenital Glaucoma: Causes, Symptoms, Diagnosis & Treatment
Understand congenital glaucoma, a rare but serious childhood eye condition—explore its causes, symptoms, diagnosis, treatment, and outlook.
Congenital glaucoma represents a group of rare disorders that affect infants and children, often threatening sight from birth or in the first few years of life. Early detection, accurate diagnosis, and timely treatment are critical in preserving vision and supporting healthy development. This comprehensive resource covers the key facts about congenital glaucoma, including its causes, symptoms, risk factors, diagnostic methods, treatment options, possible complications, and the outlook for affected children.
What Is Congenital Glaucoma?
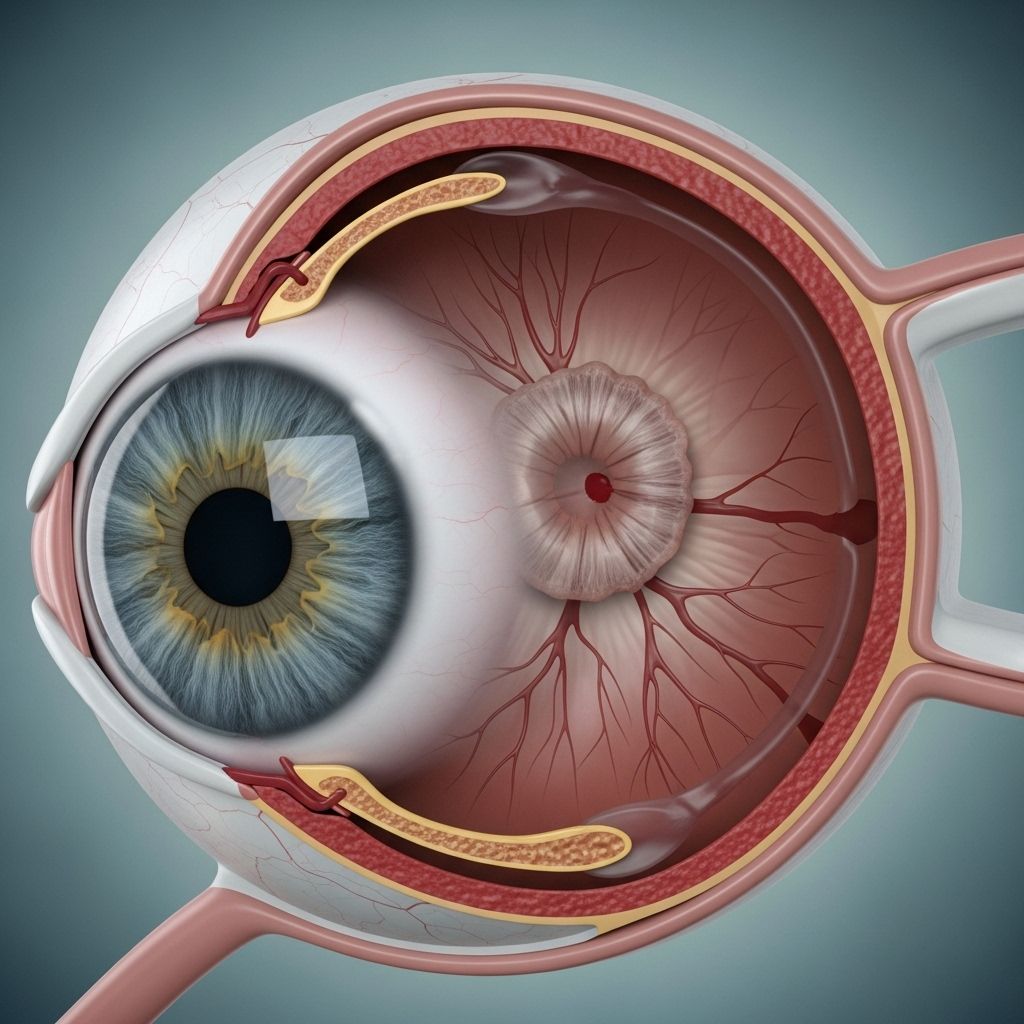
Congenital glaucoma refers to increased pressure inside a child’s eye (intraocular pressure, or IOP) due to issues with fluid drainage. This elevated pressure damages the optic nerve—the nerve responsible for carrying visual information from the eye to the brain. Unlike adult-onset glaucoma, congenital glaucoma typically causes noticeable changes in the developing eye, such as enlargement and clouding of the cornea.
- Most cases are identified within the first year of life, but some emerge later in childhood (juvenile glaucoma).
- It is a leading cause of preventable childhood blindness worldwide, responsible for about 5–18% of childhood blindness cases in some regions.
- The condition most commonly affects both eyes, but can occur in just one eye.
How Common Is It?
Congenital glaucoma is rare, with incidence rates that vary by region and population:
- Range: 1 in 2,500 to 20,000 live births, depending on ethnicity and genetic risk factors.
- Higher rates are found in populations with a greater incidence of familial or consanguineous marriages.
Types and Causes of Congenital Glaucoma
Congenital glaucoma is classified mainly into primary and secondary types, each with distinct causes and associations.
Primary Congenital Glaucoma (PCG)
Primary congenital glaucoma is due to abnormal development of the eye’s drainage tissues during pregnancy. This abnormality often results from gene mutations related to eye development (e.g., CYP1B1 and LTBP2 genes).
- Characterized by improper formation of the trabecular meshwork, the area responsible for draining “aqueous humor” (fluid in the front of the eye).
- This leads to increased eye pressure, stretching and enlarging the eye (buphthalmos), and damaging the optic nerve.
- PCG is usually noticed in children younger than 3 years but can be apparent at birth.
| Subtype | Age of Onset |
|---|---|
| True congenital glaucoma | Birth to 1 month |
| Infantile glaucoma (most common) | 1–24 months |
| Juvenile glaucoma | After 2–3 years |
Secondary Congenital Glaucoma
Secondary congenital glaucoma arises from other ocular or systemic conditions that disrupt the fluid drainage pathways. These include:
- Axenfeld-Rieger syndrome: Affects eye structure development.
- Peters anomaly: Causes corneal clouding and structural abnormalities.
- Aniridia: Partial or complete absence of the iris.
- Certain metabolic or vascular disorders that affect the eye.
Risk Factors
Several factors increase the risk of a child developing congenital glaucoma:
- Genetics: A family history of glaucoma, especially when close relatives are affected.
- Consanguinity: Parents who are closely related (such as cousins) are more likely to have a child with PCG due to autosomal recessive inheritance patterns.
- Associated syndromes: Children with certain birth defects or syndromes described above.
Symptoms of Congenital Glaucoma
Symptoms are often subtle initially, but as eye pressure rises, signs become more noticeable:
- Excessive tearing (epiphora)
- Increased sensitivity to light (photophobia)
- Cloudy or hazy cornea—may appear gray or milky
- Enlargement of the eye (buphthalmos)
- Frequent blinking or eye rubbing
- Apparent vision problems or poor visual tracking in infants
Some children develop symptoms rapidly, while in others, changes develop gradually and go unrecognized for months or even years. Early signs are often mistaken for other common conditions, such as eye infections or allergies.
When to Seek Medical Attention
Consult a pediatrician or ophthalmologist promptly if your child:
- Has persistently watery or red eyes unresponsive to standard treatments
- Demonstrates light sensitivity or avoids opening eyes in bright environments
- Has a clouded, enlarged, or abnormally shaped eye
- Shows poor vision, lack of eye contact, or fails to follow objects visually
How Is Congenital Glaucoma Diagnosed?
Diagnosis requires specialized ophthalmic assessment. The process may include these elements:
- Medical history and physical exam: Review of family history and symptoms; general health screening.
- Measurement of intraocular pressure (tonometry): Elevation above normal values for age suggests glaucoma.
- Examination of the eye’s anatomy: Slit lamp microscopy, gonioscopy (examining the drainage structures), and optic nerve imaging. Young children may require brief sedation for a thorough exam.
- Corneal diameter measurement: Enlargement of the eye and cornea is characteristic in congenital cases.
- Assessment of corneal clarity: Clouding may indicate chronic high pressure.
- Visual function tests: As appropriate for age and cognitive ability.
Treatment of Congenital Glaucoma
Successful management aims to lower intraocular pressure safely and preserve vision. Treatment almost always involves surgery, but medications may be used in preparation for or after surgery.
Surgical Treatments
Surgery is considered the primary approach for congenital glaucoma. Key procedures include:
- Goniotomy: Opening the eye’s natural drainage channel from inside, best in cases with a clear cornea.
- Trabeculotomy: Creating an alternative outflow path for eye fluid by entering from outside the eye; useful if the cornea is not clear.
- Trabeculectomy: Creating a new drainage opening if other methods fail.
- Drainage implants or tube shunts: Implanted devices to divert fluid in complex or refractory cases.
Medications
Medications can help reduce eye pressure, mainly as a temporary solution before surgery or for adjunctive control postoperatively. Types include:
- Beta-blockers
- Alpha-adrenergic agonists
- Carbonic anhydrase inhibitors
- Prostaglandin analogs
- Parasympathomimetics
Medications can have side effects and are used cautiously in infants and children—always under a doctor’s care.
Treatment for Secondary Congenital Glaucoma
Secondary glaucoma often requires management of both the primary eye defect or syndrome and the raised eye pressure. Multidisciplinary care may be necessary to address systemic issues.
Possible Complications of Congenital Glaucoma
Untreated or uncontrolled congenital glaucoma can result in significant visual impairment or blindness. Complications may include:
- Permanent vision loss
- Astigmatism (improper focusing of light by the eye)
- Myopia (nearsightedness)
- Permanent corneal clouding
Surgical and medical treatments can also cause complications. These may include:
- Cataracts (clouding of the lens)
- Retinal detachment
- Hypotony (abnormally low eye pressure)
- Infection or bleeding
Living With and Managing Congenital Glaucoma
Children who undergo treatment for congenital glaucoma require regular monitoring throughout childhood. Ongoing management may include:
- Frequent eye exams to monitor pressure and eye health
- Adjusting or repeating surgical procedures if needed
- Eye drops or oral medications as prescribed
- Vision support services—such as glasses, low vision aids, or educational adaptations if necessary
- Family education and support regarding the lifelong nature of eye care
Prognosis & Long-term Outlook
The long-term outlook for children with congenital glaucoma depends on:
- Age at diagnosis: Early identification and prompt treatment promote the best outcomes.
- Severity and type: Some children have milder, non-progressive forms; others experience ongoing challenges.
- Response to treatment: Most children who receive appropriate surgery and lifelong monitoring can maintain good vision, but regular follow-up is crucial.
Early diagnosis and intervention reduce the risk of permanent visual impairment and support healthy child development.
Frequently Asked Questions (FAQs)
Q: Can congenital glaucoma be prevented?
A: Most cases are not preventable due to their genetic or developmental origins. However, if parents are known carriers of relevant genetic mutations, genetic counseling prior to conception may be helpful.
Q: Are there warning signs parents should watch for?
A: Yes, persistent tearing, light sensitivity, cloudy or enlarged eyes, and poor vision response are warning signs requiring immediate medical evaluation.
Q: Will a child with congenital glaucoma always need surgery?
A: Surgery is the mainstay of treatment for most children with this condition, but lifelong monitoring and additional procedures or medications may also be needed.
Q: Is vision loss from congenital glaucoma reversible?
A: Vision that has already been lost is not reversible, which is why early diagnosis and treatment are essential to preserve vision.
Q: How often does congenital glaucoma run in families?
A: About 10–40% of cases have a family history. Autosomal recessive inheritance is common, especially in populations with higher rates of consanguinity.
Q: Can children with congenital glaucoma live normal lives?
A: With early diagnosis, effective treatment, and regular follow-up, many children maintain good vision and lead active lives. Some may require ongoing educational or vision support.
Key Takeaways
- Congenital glaucoma is a rare but serious cause of preventable blindness in children.
- Early signs include tearing, light sensitivity, and changes in eye appearance.
- Surgery is the primary treatment, often aided by medications.
- Lifelong monitoring and family support are vital for the best outcomes.
If you have concerns about your child’s eye health, see a pediatric eye specialist right away for assessment and, if needed, prompt treatment.
References
- https://resources.healthgrades.com/right-care/eye-health/congenital-glaucoma
- https://www.medicalnewstoday.com/articles/congenital-glaucoma
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11146270/
- https://www.healthline.com/health/eye-health/glaucoma-hereditary
- https://glaucoma.org/types/congenital-glaucoma
- https://www.ncbi.nlm.nih.gov/books/NBK574553/
Read full bio of Sneha Tete












