Conditions Commonly Associated with IgA Nephropathy
Explore which conditions are linked to IgA nephropathy, their shared mechanisms, and impacts on kidney health.
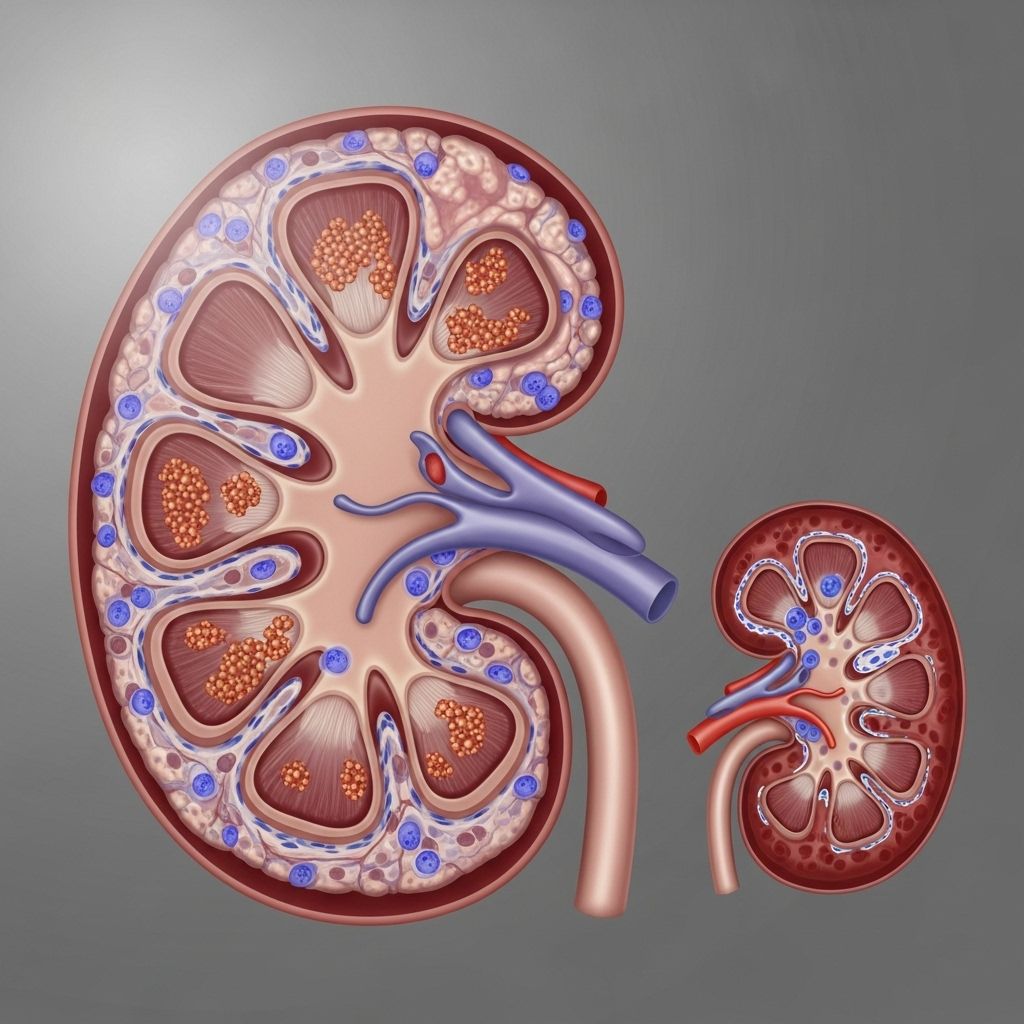
IgA nephropathy (also known as Berger’s disease) is a chronic kidney disorder caused by deposits of immunoglobulin A (IgA) in the glomeruli, the tiny filtering units within the kidneys. Although IgA nephropathy is a kidney-specific disease, it is often found in conjunction with other health conditions, especially those involving immune system dysfunction and inflammation.
Understanding IgA Nephropathy
IgA nephropathy is characterized by the accumulation of the antibody IgA in the kidneys. This accumulation leads to inflammation, kidney tissue damage, and, in some cases, the progressive loss of kidney function. The underlying cause remains unclear, but abnormal IgA production and immune complex formation are central. The disease often shows no symptoms in its early stages, but can result in hematuria (blood in urine), proteinuria (protein in urine), high blood pressure, and, in advanced cases, chronic kidney disease or failure.
- IgA Nephropathy = Kidney inflammation triggered by abnormal IgA protein buildup.
- Symptoms may first appear as blood or protein in urine after infections or physical exertion.
Why Are Other Conditions Associated With IgA Nephropathy?
IgA nephropathy is frequently linked with autoimmune disorders and systemic conditions. This is largely because immune complexes and inflammation play significant roles in both IgA nephropathy and these associated conditions. Understanding these links is crucial for both managing symptoms and anticipating complications.
- Shared immune pathways contribute to overlapping risks.
- Symptoms can be compounded when multiple conditions are present.
Main Associated Conditions
Certain conditions occur alongside IgA nephropathy more often than by chance. These include:
- Autoimmune diseases
- Inflammatory bowel disease (IBD)
- Liver disease (particularly cirrhosis)
- Dermatological disorders (such as Henoch-Schönlein purpura)
- Chronic infections
- Celiac disease
1. Autoimmune Disorders
Autoimmune diseases are those in which the immune system attacks the body’s own cells. Because IgA nephropathy involves malfunction of immune mechanisms, it’s not surprising that it may be associated with other immune-based conditions.
- Systemic lupus erythematosus (SLE): Both involve immune complex deposition in kidneys, though SLE typically deposit different immunoglobulins.
- Rheumatoid arthritis: A handful of people with IgA nephropathy have coexisting arthritis, possibly due to systemic immune activation.
- Vasculitis syndromes: Small-vessel vasculitis, including Henoch-Schönlein purpura (HSP), can present similarly and occasionally progress to IgA nephropathy.
Why these links exist: Research suggests underlying genetic and environmental factors may predispose individuals to both IgA nephropathy and other autoimmune diseases.
2. Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (encompassing Crohn’s disease and ulcerative colitis) is characterized by chronic gastrointestinal tract inflammation. There is an increased prevalence of IgA nephropathy in patients with IBD.
- Shared immune dysregulation connects the conditions.
- Gut-associated lymphoid tissue may generate abnormal IgA, facilitating kidney deposition.
Clinical significance: IBD patients with kidney involvement may get regular monitoring for proteinuria and hematuria.
3. Chronic Liver Disease and Cirrhosis
Chronic liver disease, particularly cirrhosis, significantly raises the risk for IgA nephropathy. This is likely due to impaired IgA clearance by the damaged liver; excess IgA stays in circulation and is more likely to deposit in the kidneys.
- Most common with alcoholic cirrhosis, but also in viral and autoimmune hepatitis.
- Up to 50% of patients with cirrhosis may develop mesangial IgA deposits (not always causing symptoms).
Implications: Presence of both cirrhosis and IgA nephropathy can accelerate kidney damage. Managing liver health is essential in these cases.
4. Henoch-Schönlein Purpura (IgA Vasculitis)
Henoch-Schönlein purpura (HSP) is a form of vasculitis — inflammation of small blood vessels — caused by IgA immune complex deposition. It is considered the systemic form of IgA nephropathy and most commonly affects children.
- HSP and IgA nephropathy are considered part of a disease spectrum. HSP features skin purpura, joint pain, abdominal pain, and often kidney involvement.
- Kidney disease from HSP is nearly identical histologically to IgA nephropathy.
Note: While HSP is more common in children, kidney involvement can persist or emerge in adulthood, sometimes as isolated IgA nephropathy.
5. Chronic Infections
Various chronic infections are linked to IgA nephropathy. Repeated or long-lasting infections keep the immune system highly active, increasing abnormal IgA immune complexes in circulation.
- Respiratory tract infections (like tonsillitis and pharyngitis) are notorious triggers for blood in urine episodes in IgA nephropathy patients.
- Gastrointestinal infections (such as stomach flu) may also precipitate kidney symptoms.
Prevention: Effective treatment and avoidance of recurrent infections may help reduce kidney flare-ups.
6. Celiac Disease
Celiac disease is an autoimmune reaction to gluten. There is ongoing evidence that celiac disease and IgA nephropathy may co-occur more often than by chance. The relationship may be due to abnormal gut immune responses boosting circulating IgA, which then deposits in the kidneys.
- Symptoms can overlap (gut complaints, fatigue, and kidney involvement).
- Gluten free diet may occasionally benefit those with both celiac disease and mild IgA nephropathy, according to some reports.
Table: Key Conditions Associated with IgA Nephropathy
| Condition | Type | Main Link to IgA Nephropathy | Notes |
|---|---|---|---|
| Henoch-Schönlein purpura | Vasculitis | IgA deposition in small vessels, including glomeruli | Considered systemic IgA nephropathy |
| Inflammatory bowel disease | Autoimmune, GI | Abnormal gut immune response increases circulating IgA | Increased risk for glomerular disease |
| Chronic liver disease | Hepatic | Reduced IgA clearance by damaged liver | High incidence with cirrhosis |
| Autoimmune diseases (SLE, RA, vasculitis) | Autoimmune | Genetic and immune overlaps | May complicate diagnosis and treatment |
| Chronic infections | Infectious | Trigger abnormal IgA immune responses | Episodes often follow infections |
| Celiac disease | Autoimmune, GI | Abnormal gut-derived IgA | Gluten sensitivity may worsen IgA nephropathy symptoms |
Shared Mechanisms and Implications for Management
Understanding how these conditions relate to IgA nephropathy can help patients and providers:
- Optimize management: Monitoring and managing associated conditions can support better kidney outcomes.
- Anticipate complications: Some conditions (e.g., cirrhosis, autoimmune diseases) may accelerate kidney decline.
- Personalize treatment: Addressing associated conditions, such as controlling autoimmunity or preventing infections, can help slow progression of IgA nephropathy.
Frequently Asked Questions (FAQ)
1. Are all people with IgA nephropathy at higher risk of autoimmune diseases?
Not everyone, but a significant subset may have an increased risk or family history of autoimmune conditions, especially if they have additional symptoms outside the kidneys.
2. How does liver disease affect kidney health in IgA nephropathy?
A diseased liver can’t effectively clear IgA from circulation, increasing deposits in kidneys. Managing liver health is thus crucial in patients with both conditions.
3. Does treating celiac disease improve kidney symptoms in IgA nephropathy?
Some observational data suggest that a strict gluten-free diet can reduce kidney symptoms in those with both celiac disease and IgA nephropathy, but this is not universal.
4. Can IgA nephropathy cause other organs to be affected?
IgA nephropathy primarily affects the kidneys. However, its systemic form (Henoch-Schönlein purpura / IgA vasculitis) can cause symptoms in the skin, joints, and digestive tract.
5. How common is progression to kidney failure?
About 20–40% of people with IgA nephropathy develop progressive kidney dysfunction over 20+ years; close monitoring and treating associated conditions can help delay progression.
Key Takeaways
- IgA nephropathy often coexists with systemic and immune-related conditions.
- Monitor for associated issues, especially autoimmune and gastrointestinal diseases.
- Coordinated care with specialists (gastroenterology, hepatology, rheumatology) can improve outcomes for complex cases.
- Early diagnosis and proactive management are vital to slow kidney damage.
References
- https://www.kidneyresearchuk.org/conditions-symptoms/iga-nephropathy/
- https://rarediseases.org/rare-diseases/iga-nephropathy/
- https://www.pennmedicine.org/conditions/iga-nephropathy
- https://my.clevelandclinic.org/health/diseases/5990-iga-nephropathy
- https://www.niddk.nih.gov/health-information/kidney-disease/iga-nephropathy
- https://www.ncbi.nlm.nih.gov/books/NBK538214/
- https://www.kidney.org/kidney-topics/iga-nephropathy
Read full bio of medha deb












