Complications of IgA Nephropathy: Understanding Risks and Management
Explore the serious complications of IgA nephropathy and learn how timely detection and management can protect kidney health.
IgA nephropathy (IgAN), also known as Berger disease, is recognized as one of the most common primary glomerular diseases resulting in chronic kidney damage. This comprehensive guide explores the major complications that may arise from IgA nephropathy, their underlying mechanisms, and current strategies for reducing risks and improving long-term outcomes.
What is IgA Nephropathy?
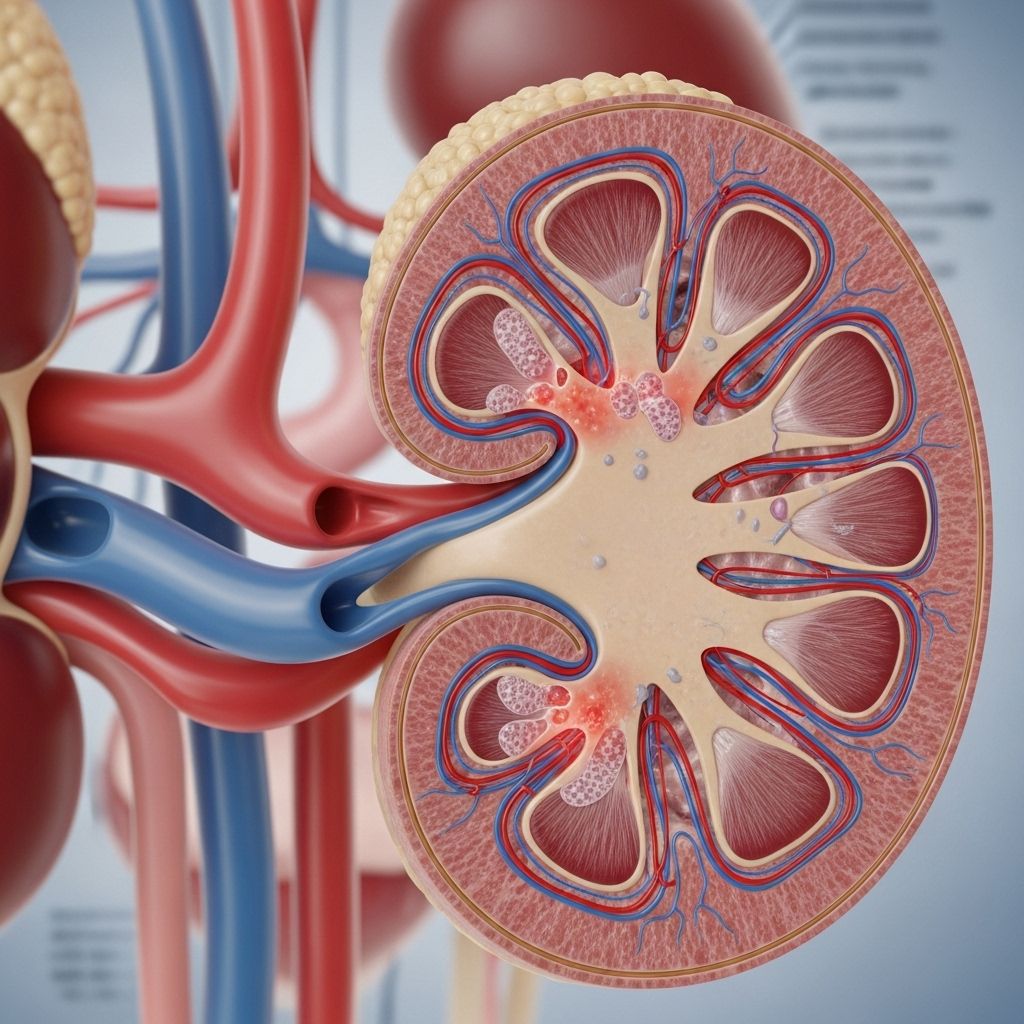
IgA nephropathy is a chronic disease affecting the kidneys, driven by the deposition of immunoglobulin A (IgA) in the glomeruli—the kidney’s tiny blood-filtering units. The buildup of these antibodies causes inflammation, leading to gradual damage and scarring of the kidney tissues. Over time, this can impair the organs’ filtration capability, disrupting essential processes such as blood detoxification, fluid balance regulation, and red blood cell production.
For some, the disease course is slow and mild; for others, it is progressive and may lead to significant complications, including end-stage kidney failure.
Who is at Risk?
- Individuals with a family history of kidney disease
- People of East Asian or Caucasian descent (prevalence varies worldwide)
- Men are more commonly affected than women
- Onset often occurs in late teens to mid-30s
How Does IgA Nephropathy Affect the Kidneys?
IgA deposits incite inflammation in the glomeruli. This process, left unchecked, results in:
- Kidney tissue scarring (fibrosis)
- Loss of filtration efficiency
- Progressive decline in overall kidney function
Kidney impairment from IgAN can develop gradually, often without early symptoms. Yet, persistent damage triggers several notable and potentially serious complications.
Major Complications of IgA Nephropathy
The long-term health risks associated with IgA nephropathy arise as kidney structures become increasingly compromised. The principal complications include:
1. Hypertension (High Blood Pressure)
As kidney damage worsens, blood filtration becomes inefficient. This dysfunction causes a buildup of sodium and fluid in the body, increasing blood volume and blood vessel pressure.
- Prevalence: Common in people with progressive IgAN.
- Mechanism: Poor filtration of sodium and water elevates blood volume; protein loss (proteinuria) exacerbates this effect.
- Risks: Uncontrolled hypertension accelerates kidney damage and significantly increases the risk of heart disease and stroke.
Management: Blood pressure control using medications (ACE inhibitors, ARBs), low-sodium diet, and regular monitoring can help reduce this risk.
2. Nephrotic Syndrome
Nephrotic syndrome describes a collection of symptoms that reflect severe kidney dysfunction. It’s characterized by:
- High levels of protein in the urine (proteinuria)
- Low blood protein levels
- Hyperlipidemia (elevated cholesterol and triglycerides)
- Significant fluid retention (edema), particularly in the legs, ankles, and hands
Common symptoms of nephrotic syndrome include:
- Edema (swelling) in extremities or around eyes
- Significant weight gain from fluid buildup
- Fatigue and weakness
- Foamy or frothy urine
- Lowered appetite
Why it matters: Nephrotic syndrome may further raise the risk of infections, blood clots, anemia, and heart disease due to changes in blood chemistry and immune function.
3. Chronic Kidney Disease (CKD)
CKD is characterized by the persistent, gradual loss of kidney function. Ongoing inflammation and scarring from IgAN can push a person through various stages of CKD, ultimately affecting their body’s ability to regulate waste, fluids, and electrolytes.
- Symptoms (as CKD progresses):
- Fatigue and weakness
- Swelling in legs, ankles, or around the eyes
- Changes in urination patterns (frequency, color)
- High blood pressure that remains difficult to control
- Poor appetite, nausea, or vomiting
- Risks: CKD increases the likelihood of developing cardiovascular disease, anemia, bone disease, and can progress to irreversible kidney failure.
4. Kidney Failure (End-Stage Renal Disease)
In advanced cases, kidney function deteriorates to a degree where it is insufficient for sustaining life. This is termed kidney failure or end-stage renal disease (ESRD).
- Prevalence in IgAN: About 1 in 5 people progress to kidney failure within a decade after diagnosis.
- Symptoms:
- Persistent nausea and vomiting
- Muscle cramps and weakness
- Severe swelling (edema)
- Metallic taste in the mouth
- Mental confusion or difficulty concentrating
Treatment options for kidney failure include:
- Dialysis (hemodialysis or peritoneal dialysis)
- Kidney transplantation
Complications Associated with CKD and Kidney Failure
- Anemia (due to reduced erythropoietin production by the kidneys)
- Abnormal calcium and phosphorus metabolism, leading to bone changes
- Electrolyte imbalances (such as elevated potassium)
- Increased susceptibility to infections
- Heart disease and vascular calcification
Progression and Prognosis of IgA Nephropathy
The course of IgA nephropathy varies widely among individuals. Influencing factors include:
- Genetic predisposition
- Underlying medical conditions (such as diabetes or hypertension)
- Environmental triggers (such as infections)
- Patient adherence to treatment recommendations
Some individuals may remain asymptomatic for years, while others may experience rapid progression to severe kidney dysfunction. It is essential to monitor for complications even in the absence of symptoms.
Symptoms to Watch For
Early IgA nephropathy often goes unnoticed. However, as the disease progresses, certain symptoms may signal kidney involvement:
- Cola or tea-colored urine (from blood in urine, called hematuria)
- Proteinuria (foamy or frothy urine)
- Swelling (edema) in the hands, feet, or face
- Flank or lower back pain
- Persistent fatigue
- Unexplained weight gain
- Loss of appetite
If kidney failure develops, symptoms may include:
- Persistent nausea and vomiting
- Muscle cramps
- Itchy skin and rashes
- Metallic taste in the mouth
- Confusion or cognitive changes
Diagnosis and Monitoring
Because IgA nephropathy can be silent in its early phases, diagnosis is often made after laboratory tests detect abnormal amounts of blood or protein in urine. Further workup may involve:
- Urine analysis for blood and protein
- Blood tests for kidney function markers (creatinine, eGFR)
- Kidney biopsy (definitive diagnosis)
- Imaging studies in select cases
Strategies for Managing and Reducing Complications
While there is no definitive cure for IgA nephropathy, proactive management can slow disease progression and lessen the impact of complications. Key pillars include:
- Blood pressure control: Target levels are generally <130/80 mm Hg for those at risk of CKD.
- Proteinuria reduction: ACE inhibitors and ARBs are effective pharmacologic approaches.
- Diet modification: Low sodium and adequate protein intake, often under the guidance of a dietitian.
- Monitoring and screening: Regular follow-ups with urine and blood tests.
- Treating infections promptly: To reduce immune activation and further kidney damage.
- Lifestyle changes: Smoking cessation, regular physical activity, and weight management.
When to See a Doctor
Prompt medical attention is recommended if you notice:
- Blood in the urine (hematuria)
- Significant, persistent swelling of limbs or face
- Significant changes in urination patterns
- Unexplained persistent fatigue or loss of appetite
Early and ongoing dialogue with a healthcare provider ensures the best chance of intercepting and managing complications early.
Outlook and Living with IgA Nephropathy
While IgA nephropathy can follow an unpredictable course, early detection, regular monitoring, and targeted interventions can reduce your risk of severe complications. Many individuals live with IgAN for years with stable or slowly progressive kidney function.
| Complication | Description | Potential Impact | Management Strategies |
|---|---|---|---|
| Hypertension | Elevated blood pressure due to sodium and fluid retention | Increased risk of further kidney damage, heart disease | Medication, lifestyle changes, sodium restriction |
| Nephrotic Syndrome | High protein loss in urine, low blood protein, swelling | Infections, blood clots, heart disease | Medication to reduce proteinuria, manage fluids |
| Chronic Kidney Disease (CKD) | Loss of kidney function over time | Anemia, bone disease, cardiovascular disease | Monitor kidney function, control blood pressure |
| Kidney Failure (ESRD) | Kidneys unable to support body needs | Life-threatening without treatment | Dialysis, transplantation |
FAQs: Frequently Asked Questions about IgA Nephropathy Complications
What are the earliest signs of IgA nephropathy complications?
The most common early signs include persistent blood in the urine (often appearing dark or cola-colored) and foamy urine due to increased protein. Swelling in the ankles or hands may also suggest declining kidney function.
How quickly do complications develop in IgA nephropathy?
Complications may develop gradually, often over many years. For some, kidney function may remain stable; for others, progression to serious complications like hypertension, proteinuria, or kidney failure can occur within a decade.
Can hypertension from IgA nephropathy be reversed?
Hypertension itself may not be reversible, but it can be well-controlled with proper medication, dietary changes, and regular monitoring, thus slowing further kidney damage.
Is dialysis always required in kidney failure due to IgA nephropathy?
No. Dialysis (or kidney transplantation) is needed only if kidney failure (ESRD) develops and kidney function drops below the threshold required for life. Many people with IgA nephropathy never require dialysis, especially with good early management.
How often should someone with IgA nephropathy see their doctor?
Regular follow-ups are vital—typically every 3–6 months—especially if any complications or risk factors are present. Frequency may increase based on disease severity, symptom changes, or treatment evaluations.
Key Takeaways
- IgA nephropathy is a common cause of kidney disease and can lead to significant complications.
- Major risks include hypertension, nephrotic syndrome, chronic kidney disease, and kidney failure.
- Early detection, lifestyle changes, and medical management can help slow disease progression and reduce complications.
- Regular medical monitoring is essential to preserve kidney health and quality of life.
Always consult with your healthcare provider if you experience concerning symptoms, or if you have a diagnosis of IgA nephropathy and want to understand your risk for complications better.
References
- https://www.healthline.com/health/kidney-disease/complications-iga-nephropathy
- https://davita.com/education/articles/iga-nephropathy-bergers-disease/
- https://www.mayoclinic.org/diseases-conditions/iga-nephropathy/symptoms-causes/syc-20352268
- https://www.niddk.nih.gov/health-information/kidney-disease/iga-nephropathy
- https://www.kidney.org/kidney-topics/iga-nephropathy
- https://unckidneycenter.org/kidneyhealthlibrary/glomerular-disease/iga-nephropathy/
- https://www.kidney.org.uk/iga-nephropathy
- https://picnichealth.com/blogs/iganephropathy-symptoms-and-signs
Read full bio of medha deb












