Complications of Heart Disease: Effects, Risks, and Management
Explore the short- and long-term complications of heart disease, key risk factors, common symptoms, and effective management strategies.
Complications of Heart Disease: Long- and Short-Term Effects
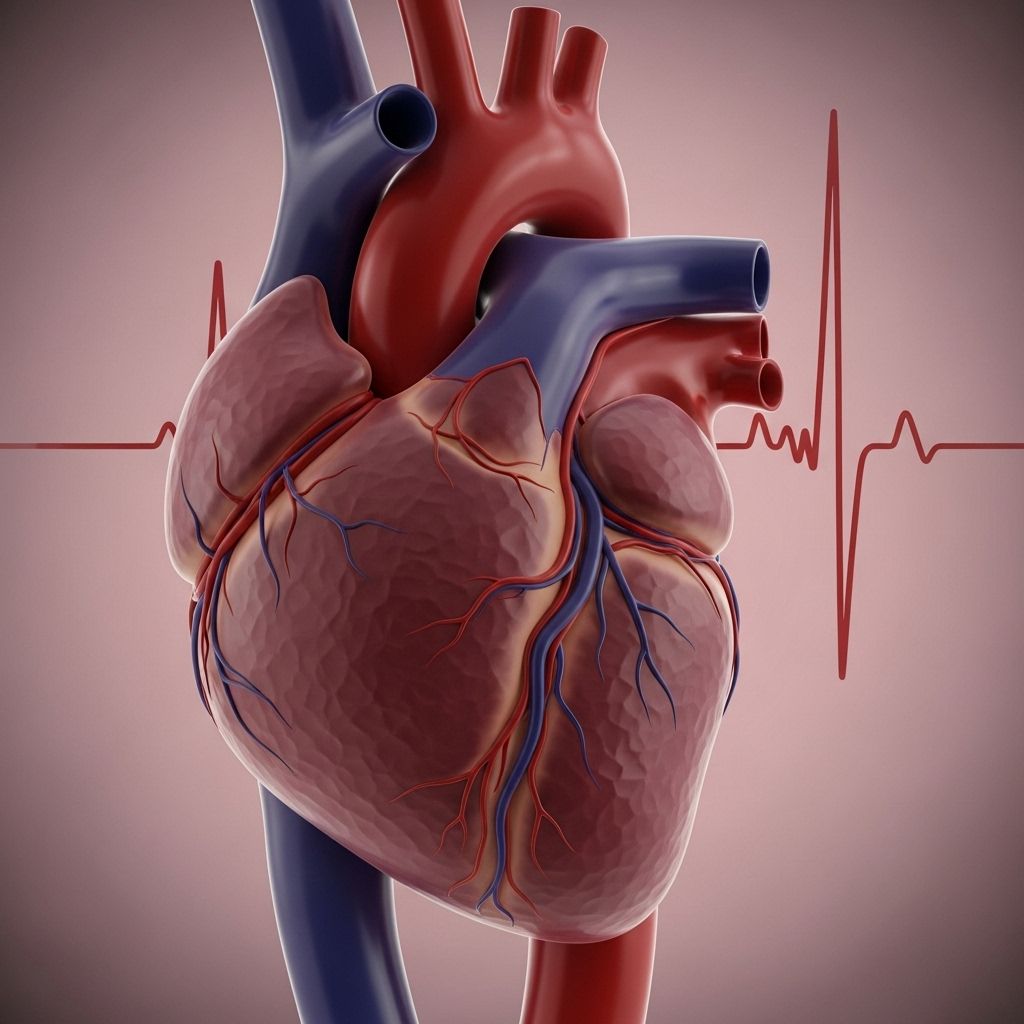
Heart disease is a leading cause of death worldwide, encompassing a broad range of conditions that affect the heart muscle, heart valves, coronary arteries, and heart rhythm. Its complications can impact multiple organ systems and lead to both short- and long-term health issues. Understanding these complications, their symptoms, and ways to manage or prevent them is essential for maintaining cardiovascular health and overall wellbeing.
Overview: What Is Heart Disease?
“Heart disease” is an umbrella term that includes conditions such as coronary artery disease, heart failure, arrhythmias (irregular heart rhythms), and more. It typically involves either structural or functional issues within the heart and its associated blood vessels. According to the Centers for Disease Control and Prevention (CDC), heart disease remains the leading cause of mortality in the United States.
- Affects heart muscle, valves, arteries, rhythm
- Main risk factors: High blood pressure, high cholesterol, smoking, diabetes, obesity
- Treatment: Lifestyle changes, medications, surgical interventions
If left unchecked, heart disease can lead to serious, sometimes fatal, complications affecting organs and overall quality of life.
Major Complications of Heart Disease
Heart disease complications vary depending on the underlying problem but typically share several life-threatening outcomes. Below are the principal complications experienced by affected individuals.
Heart Failure
Heart failure occurs when the heart cannot pump enough blood to meet the body’s needs. While the heart may try to compensate by beating faster, building muscle, or stretching to take in more blood, these adaptations eventually impair heart function.
- Symptoms include: Shortness of breath, dizziness, fluid retention (edema), confusion
- Common causes: Untreated coronary artery disease, high blood pressure, arrhythmias
- Complications: Kidney and liver impairment, blood clots, muscle wasting, pulmonary edema
Early treatment can slow progression, but advanced heart failure is often debilitating and may require complex management, including medications and surgical options.
Heart Attack (Myocardial Infarction)
A heart attack results from a sudden interruption of blood flow to the heart muscle, typically caused by a blockage in a coronary artery. This event damages or destroys part of the heart muscle and can rapidly become life-threatening.
- Symptoms: Severe chest pain, breathlessness, nausea, sweating
- Complications: Heart failure, arrhythmias, cardiogenic shock, heart rupture
Timely treatment, such as restoration of blood flow and medication, is vital to minimize damage and increase survival rates.
Stroke
Stroke occurs when the blood supply to the brain is interrupted, often due to a clot or narrowed artery. Stroke is a common complication of heart disease, especially in those with atrial fibrillation or high blood pressure.
- Symptoms: Sudden weakness or numbness (especially one side), difficulty speaking, vision problems, confusion
- Consequences: Permanent brain damage, paralysis, speech and cognitive deficits
Prevention focuses on controlling blood pressure, treating cardiac arrhythmias, and managing cholesterol and diabetes.
Pulmonary Embolism (PE)
Pulmonary embolism is a sudden blockage of the blood vessel in the lungs, usually caused by a blood clot that has traveled from elsewhere in the body. While similar to stroke in mechanism, it affects the lungs instead of the brain and rapidly deprives the body of oxygen.
- Symptoms: Sharp chest pain upon breathing, shortness of breath, bluish skin, rapid heartbeat
- Emergency: PE requires immediate medical attention to prevent death
Risk for PE is increased in people with heart failure or arrhythmias, as blood clots are more likely to develop.
Cardiac Arrest
Cardiac arrest refers to the sudden cessation of heart function, usually owing to electrical disturbances. It is often triggered by an arrhythmia brought on by underlying heart disease and can result in abrupt loss of consciousness and death if not rapidly addressed.
- Symptoms: Dizziness, heart palpitations, shortness of breath, fatigue, nausea
- Immediate response: CPR and early defibrillation are critical for survival
Cardiac arrest is among the most deadly heart disease complications and demands prompt emergency action.
Peripheral Artery Disease (PAD)
PAD involves the narrowing of arteries outside the heart, especially those supplying the arms and legs, similar to what occurs in coronary artery disease.
- Main symptom: Intense leg pain during walking or exercise
- Risks: Impaired mobility, ulcers, tissue death requiring amputation
Treatment typically includes lifestyle modifications, medications to improve circulation, and sometimes surgical intervention.
Atrial Fibrillation (AFib)
AFib is an arrhythmia causing the upper heart chambers (atria) to quiver rather than beat normally. This disrupts blood flow and can result in blood clots, increasing the risk of stroke or heart failure.
- Symptoms: Irregular heartbeat, fluttering chest sensation
- Consequences: Stroke risk, progressive heart failure
AFib is treatable and rarely fatal, but its association with severe complications makes early detection and management essential.
Angina
Angina refers to chest pain arising from reduced blood flow to the heart. It is commonly a symptom of coronary artery disease and can be stable (predictable, after exertion) or unstable (unexpected, possibly at rest).
- Symptoms: Pressing or squeezing chest pain, pain radiating to neck or arm, shortness of breath
- Risks: Progression to heart attack if blood supply is severely limited
Angina management involves medication, lifestyle changes, and sometimes surgical interventions to restore blood flow.
Table: Major Heart Disease Complications and Symptoms
| Complication | Main Symptoms | Potential Consequences |
|---|---|---|
| Heart Failure | Shortness of breath, edema, confusion | Organ dysfunction, death |
| Heart Attack | Chest pain, breathlessness, nausea | Heart muscle damage, heart failure, death |
| Stroke | Weakness, confusion, speech problems | Permanent disability, death |
| Pulmonary Embolism | Sharp chest pain, blue skin, breathlessness | Sudden death |
| Cardiac Arrest | Dizziness, palpitations, collapse | Immediate death if untreated |
| PAD | Leg pain on walking | Mobility loss, amputation |
| AFib | Irregular heartbeat, chest fluttering | Stroke, heart failure |
Short-Term vs. Long-Term Effects of Heart Disease Complications
Complications may occur suddenly or develop progressively. Early symptoms may be mild or non-specific, while advanced or untreated disease can manifest as severe impairment or acute emergencies.
Short-Term Effects
- Shortness of breath
- Chest pain (angina)
- Dizziness, lightheadedness
- Fatigue
- Edema (swelling)
Long-Term Effects
- Permanent organ damage
- Loss of mobility or independence
- Chronic heart failure symptoms
- Higher risk of recurrent cardiovascular events
- Reduced life expectancy
Prevention and Management Strategies
Many heart disease complications can be prevented or managed through effective lifestyle modifications, medical therapies, and in some cases, surgery.
- Lifestyle Changes: Healthy diet, regular exercise, weight maintenance, stress management, smoking cessation
- Medications: Blood pressure control, cholesterol lowering drugs, anticoagulants (to reduce clot risk), anti-arrhythmic drugs
- Surgical Procedures: Coronary artery bypass grafting (CABG), angioplasty, heart valve repair or replacement
Careful management of risk factors—such as hypertension, diabetes, cholesterol—can slow disease progression and reduce the likelihood of complications.
Frequently Asked Questions About Heart Disease Complications
What are the five major risks for heart disease?
- Smoking
- High blood pressure
- High cholesterol
- Diabetes
- Overweight or obesity
What are common complications of heart failure?
- Arrhythmia (irregular heartbeat)
- Blood clots
- Impaired kidney or liver function
- Muscle wasting
- Pulmonary edema
- Trouble breathing
What are the typical complications after a heart attack?
- Arrhythmias
- Heart failure
- Cardiogenic shock
- Heart rupture
What are frequent complications of coronary artery disease?
- Heart failure (cardiac insufficiency)
- Arrhythmia
- Heart attack
How do you reduce your risk of heart disease complications?
- Eat a balanced, heart-healthy diet
- Exercise daily
- Quit smoking
- Manage blood pressure, cholesterol, and blood sugar levels
- Take prescribed medications consistently
- Undergo recommended screenings and follow-up care
Key Takeaways
- Heart disease is a serious, progressive condition with potentially fatal complications
- Core complications include heart failure, heart attack, stroke, arrhythmias, PAD, and pulmonary embolism
- Prompt recognition and management of symptoms can improve outcomes
- Lifestyle changes, medications, and surgery may be required for prevention and effective disease management
- Regular consultations with a healthcare provider are crucial for those at risk
References
- https://www.healthline.com/health/heart-disease/complications
- https://www.medicalnewstoday.com/articles/237191
- https://lifeprogram.org.au/health-hub/earlysignsofheartdiseaseinmen/
- https://www.healthline.com/health/heart-disease
- https://www.medicalnewstoday.com/articles/257484
- https://www.healthline.com/health/video/how-to-prevent-heart-disease-according-to-a-cardiologist
- https://www.cedars-sinai.org/newsroom/healthline-therapy-vs-antidepressants–which-is-best-for-people-with-heart-disease/
- https://www.healthline.com/health/video/a-cardiologist-explains-what-your-diet-does-to-your-heart
- https://www.healthline.com/health/video/what-happens-to-your-body-with-high-blood-pressure
- https://medlineplus.gov/heartdiseases.html
Read full bio of medha deb












