Complications of Graves’ Disease: Understanding Eye Health Impacts
Explore the full range of eye complications caused by Graves' disease, from mild discomfort to vision-threatening conditions, and discover current treatments.
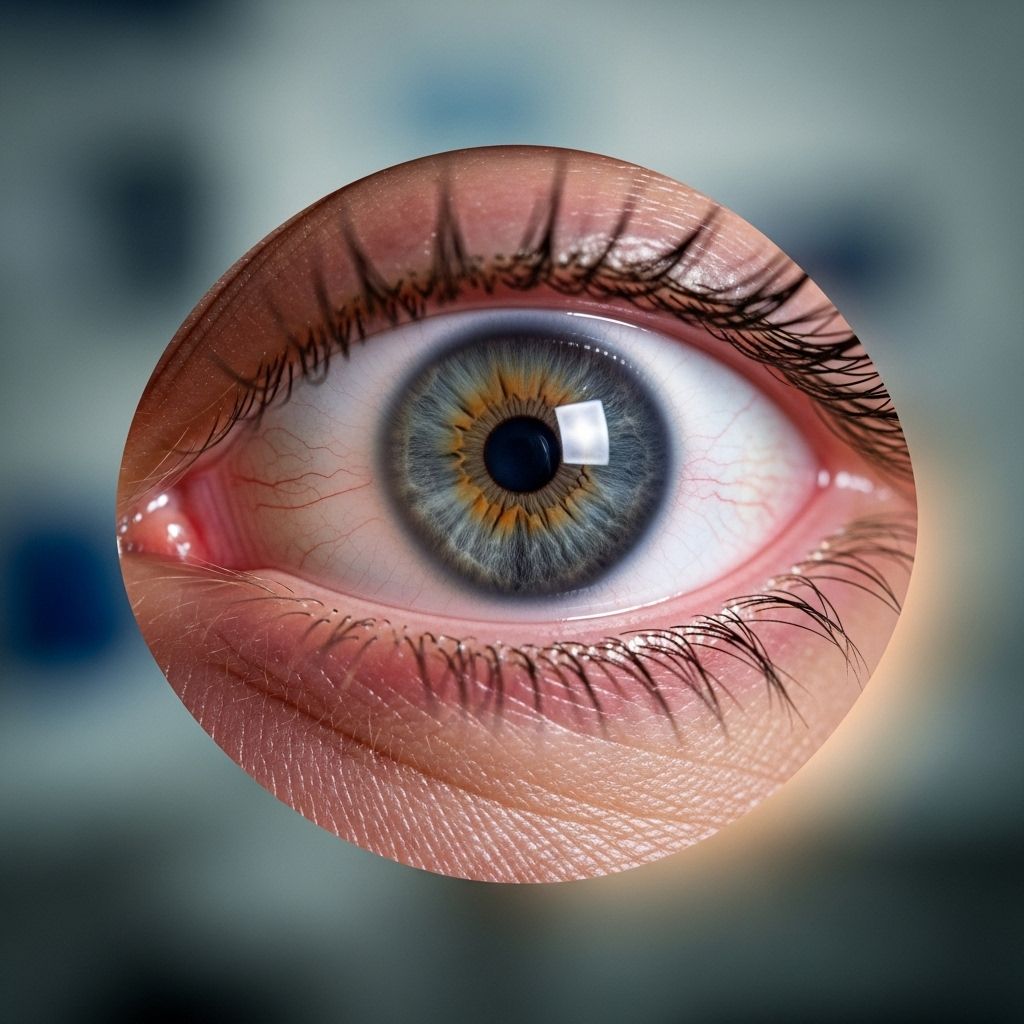
Graves’ disease, an autoimmune condition primarily affecting the thyroid gland, is known for its impact on metabolism and energy levels. However, this disorder can also have significant and sometimes severe effects on the eyes. These effects are collectively referred to as Thyroid Eye Disease (TED) or Graves’ orbitopathy. Recognizing, understanding, and managing these ocular complications is essential for preserving vision and improving quality of life in individuals with Graves’ disease.
What Is Graves’ Disease?
Graves’ disease is the most common cause of hyperthyroidism, a state in which the thyroid gland produces excessive thyroid hormones. While its hallmark symptoms include rapid heartbeat, weight loss, and irritability, up to 25 630% of people with Graves’ disease will also develop eye complications. The underlying mechanism involves antibodies that mistakenly target not only the thyroid gland but also the tissues surrounding the eyes, leading to the development of TED or Graves’ ophthalmopathy.
How Graves’ Disease Affects the Eyes
The eye complications associated with Graves’ disease result from inflammation and swelling in the tissues around the eyes, particularly the muscles and fat behind the eyeball. This inflammation is driven by the body 27s immune response, which, in addition to attacking the thyroid, also targets the connective tissue and muscles in the orbital (eye socket) area.
- Ocular symptoms often develop or worsen independently of thyroid hormone levels.
- Both eyes can be affected, though severity may differ between sides.
- Complications may be mild and self-limiting or progress to severe, vision-threatening disease.
Symptoms and Signs of Thyroid Eye Disease
Recognizing early symptoms of TED is crucial for timely intervention. The condition can manifest with a range of symptoms, from mild irritation to significant changes in eye appearance and function.
- Redness and pain: Caused by swelling and inflammation in the tissues around the eyes.
- Puffiness around the eyes: Periorbital swelling, sometimes accompanied by bruising or a discolored appearance.
- Bulging eyes (proptosis): Outward protrusion of the eyeball due to increased tissue volume in the orbit.
- Dry eye and irritation: Occurs when eyelids cannot fully close, leading to exposure and dehydration of ocular surfaces.
- Watery eyes: Reflex tearing as the dry, irritated eyes overproduce tears.
- Bags under eyes: Swelling and herniation of orbital tissue.
- Double vision (diplopia): Restriction in eye movement due to inflamed or scarred eye muscles.
- Blurred vision: Less commonly, when swelling or corneal exposure interferes with visual clarity.
- Gritty or foreign body sensation: Discomfort reminiscent of having sand in the eyes.
- Light sensitivity: Photophobia or discomfort triggered by bright light.
- Pain with eye movement: Especially when looking up, down, or to the side.
These symptoms can vary in intensity, and not all individuals will experience the complete spectrum of signs. Mild cases might resolve as thyroid function normalizes, though some eye changes may persist without further disease activity.
Serious Complications and Risks
Although many people experience mild symptoms, Graves’ eye disease can occasionally progress to more severe and potentially sight-threatening complications. Understanding these risks underscores the importance of prompt recognition and management.
- Excessive proptosis: Severe bulging of the eyes may lead to an inability to fully close the eyelids, increasing the risk of corneal drying, ulceration, and infection.
- Optic nerve compression: Swollen and fibrotic eye muscles or tissues can press on the optic nerve at the back of the socket, compromising blood flow and nerve function. This is the most dangerous complication, as it can result in irreversible vision loss.
- Corneal ulceration: When the clear covering of the eye (cornea) becomes exposed, dry, or ulcerated, serious vision-threatening infections can develop.
- Glaucoma: Although rare, increased orbital pressure from swelling can interfere with normal eye drainage, leading to increased intraocular pressure and optic nerve damage.
Warning Signs: When to Seek Urgent Help
- Sudden loss of vision
- Severe eye pain or pressure
- Marked changes in color vision or perception
- Rapid progression of bulging or swelling
If any of these symptoms develop, immediate evaluation by an ophthalmologist is essential to prevent permanent damage.
Underlying Causes and Mechanisms
The immune system’s abnormal response in Graves’ disease is central to the development of thyroid eye disease. Antibodies mistakenly attack both the thyroid gland and orbital tissues, including the eye muscles. These antibodies, particularly the thyroid-stimulating hormone receptor antibody (TSHR-Ab), promote inflammation, swelling, and subsequent scarring.
- Inflammation leads to widening and stiffening of extraocular muscles.
- Fat accumulation in the orbit contributes to eye bulging and eyelid changes.
- In severe cases, ongoing scarring reduces the range of motion of the eyes and compresses critical structures, such as the optic nerve.
Who Is at Risk for Eye Complications?
Several factors increase the likelihood of developing thyroid eye disease in people with Graves’ disease:
- Gender: Women are more frequently affected than men.
- Age: The risk increases with age, especially above 40 years.
- Smoking status: Smokers have a significantly elevated risk of developing and worsening TED.
- Uncontrolled thyroid function: Fluctuating or poorly managed thyroid hormone levels can exacerbate eye problems.
- Radioactive iodine therapy: Used to treat hyperthyroidism, this therapy may initially worsen TED symptoms, especially without concurrent steroid prophylaxis.
- Family history and genetic predisposition: A family history of autoimmune thyroid disease can increase susceptibility.
Stages and Classification of Thyroid Eye Disease
Thyroid eye disease typically follows a biphasic course:
- Active (inflammatory) phase: Characterized by swelling, redness, and progressive symptoms; generally lasts six months to two years.
- Inactive (fibrotic) phase: Inflammation subsides but residual scarring, bulging, or double vision may persist.
The severity of TED can be classified as:
- Mild: Mild discomfort, redness, or swelling; minimal or no impact on everyday life.
- Moderate: Noticeable changes in appearance, double vision, significant discomfort or tearing.
- Severe: Sight-threatening complications, marked proptosis, optic nerve involvement, or corneal breakdown.
Diagnosis and Evaluation
Diagnosis is based on a combination of clinical signs, symptoms, and specialized tests:
- Clinical exam: Assessment for characteristic eye and eyelid changes, motility restrictions, and visual acuity.
- Imaging studies: CT or MRI may reveal enlarged eye muscles or orbital fat.
- Blood tests: Analysis of thyroid hormone levels (T3, T4, TSH) and antibodies.
- Visual field and color testing: Used to evaluate optic nerve function when compression is suspected.
Treatment Options for Graves’ Eye Disease
The approach to treating thyroid eye disease is tailored to the severity of symptoms and individual patient needs. Options range from conservative measures to targeted therapies and surgery.
Lifestyle and Supportive Care
- Smoking cessation: Stopping smoking is the most important modifiable factor to reduce risk and severity.
- Lubricating eye drops: Artificial tears help relieve dryness and irritation.
- Cool compresses: Can ease inflammation and swelling.
- Sunglasses: Protect sensitive eyes from wind, sun, and airborne irritants.
- Head elevation during sleep: Can reduce periorbital swelling.
Medical Therapies
- Oral or intravenous corticosteroids: Reduce inflammation in moderate-to-severe active disease.
- Immunosuppressive agents: Medications such as mycophenolate mofetil are sometimes used for patients who do not respond to steroids.
- Monoclonal antibodies: Recent advances have introduced agents like teprotumumab, approved specifically for active, moderate-to-severe TED.
- Radiation therapy: Rarely used, can sometimes help decrease inflammation and improve eye movement.
Surgical Interventions
- Orbital decompression surgery: Removes bone or fat from the eye socket to relieve pressure and reduce proptosis in severe cases.
- Strabismus surgery: Repositions eye muscles to correct double vision.
- Eyelid surgery: Repairs retracted or scarred eyelids, improves closure and appearance.
- Corneal protection procedures: Partially or completely closing the eyelids (tarsorrhaphy) if exposure endangers vision.
Medical and surgical therapies are often used in a stepwise fashion, based on the disease stage and patient response.
Managing Vision Changes and Eye Discomfort
Many people living with Graves’ disease are concerned about losing vision. While total blindness is rare, changes in vision do occur and should be monitored closely. Preventive care and early treatment are essential:
- Attend regular follow-ups with both your endocrinologist and ophthalmologist.
- Monitor for changes in vision, color perception, or eye pain and report them promptly.
- Take practical self-care measures to maintain eye comfort, such as using humidifiers or eye shields at night.
Frequently Asked Questions (FAQs)
Q: Can Graves’ disease cause permanent blindness?
A: Permanent blindness is extremely rare in Graves’ eye disease. However, severe complications such as optic nerve compression or untreated corneal ulceration can lead to vision loss if not addressed promptly.
Q: Will my eye symptoms improve if my thyroid levels are controlled?
A: Controlling thyroid hormone levels is important, but TED often develops or persists independently. Some symptoms may improve with thyroid normalization, but eye changes may remain or require separate treatment.
Q: Are there ways to prevent thyroid eye disease?
A: Not all cases can be prevented, but the most effective protective measure is to avoid smoking. Regular eye exams and careful thyroid management can also reduce risks and help detect complications early.
Q: How is double vision treated in Graves’ eye disease?
A: Double vision may be managed with special glasses (prisms), temporary patches, or surgical correction if persistent.
Q: Do all people with Graves’ disease get eye symptoms?
A: No. Only about 25 630% develop some degree of thyroid eye disease, and severe vision-threatening complications are much less common.
Key Points to Remember
- Graves’ disease is a common cause of thyroid eye disease, which can range from mild irritation to significant vision disturbance.
- Early detection and coordinated care between endocrinologists and ophthalmologists greatly reduce the risk of permanent complications.
- Self-care, lifestyle modifications, and medical therapies are essential components in the management of TED.
- Always seek immediate medical evaluation if vision changes or severe eye symptoms arise.
Resources and Support
- Endocrinology clinics: For the management of underlying thyroid dysfunction.
- Ophthalmology specialists: For assessment and treatment of eye complications and surgical interventions.
- Patient advocacy groups: Offer information, peer support, and resources for individuals living with Graves’ disease and thyroid eye disease.
Table: Common Eye Complications in Graves’ Disease
Read full bio of Sneha Tete












