Complications of Chronic Kidney Disease: Risks, Prevention, and Management
Learn about the diverse complications of chronic kidney disease, their impact, and essential prevention and treatment approaches.
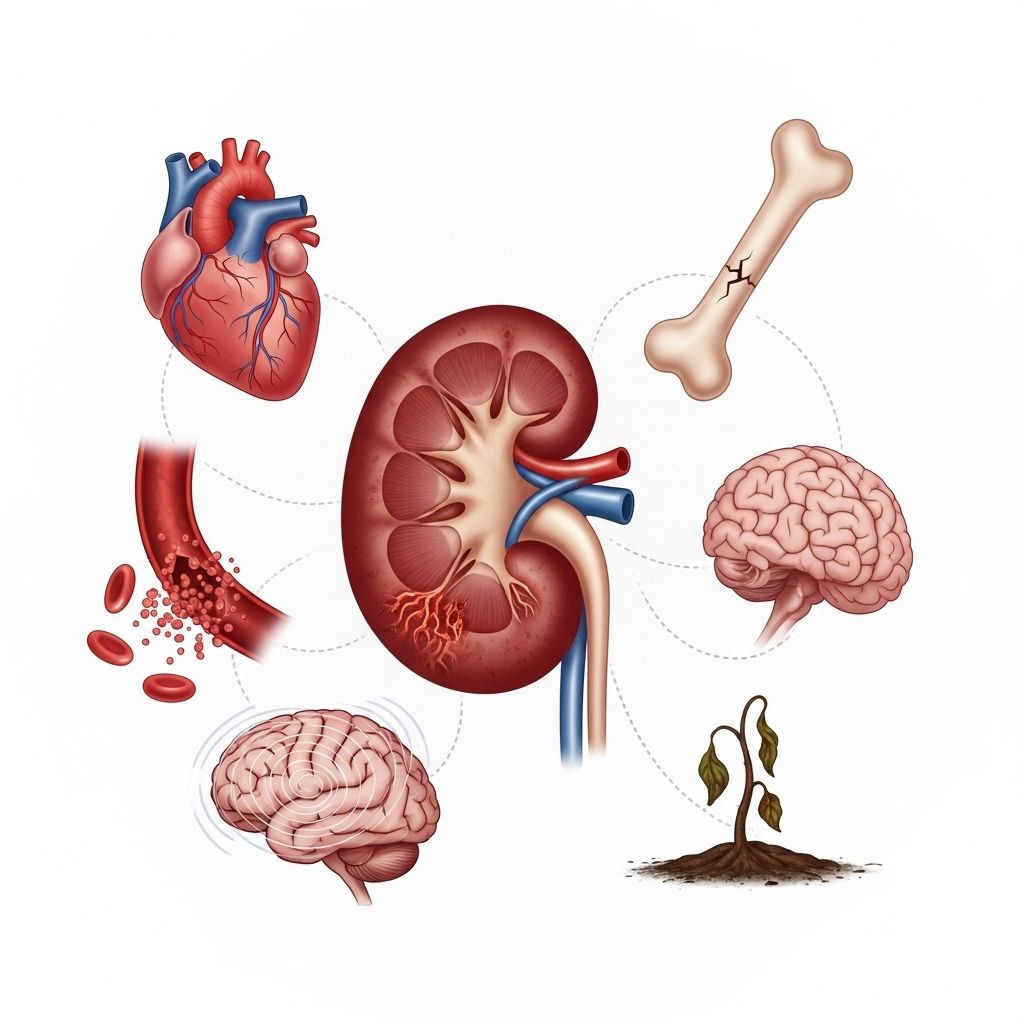
Complications of Chronic Kidney Disease
Chronic kidney disease (CKD) is a progressive condition that impairs the kidneys’ ability to filter waste and regulate bodily functions. As CKD advances, it does not just affect the kidneys—it can lead to significant complications throughout the body. Understanding these risks and their management is crucial to preserving health and quality of life in patients with CKD.
What Are the Complications of Chronic Kidney Disease?
Untreated CKD can result in various systemic complications, each with their own set of symptoms and health impacts. The main complications include:
- Anemia
- Bone Weakness
- Fluid Retention
- Gout
- Heart Disease
- High Blood Pressure (Hypertension)
- Hyperkalemia (High Potassium Levels)
- Neurological and Secondary Complications
Anemia
Anemia is frequently observed in people with CKD, particularly those undergoing dialysis or with end stage renal disease (ESRD). Healthy kidneys release erythropoietin (EPO), a hormone vital for the production of red blood cells. When CKD impairs EPO production, anemia develops, reducing the blood’s capacity to transport oxygen.
- Caused by low levels of EPO, iron, vitamin B12, and folic acid
- Leads to fatigue, weakness, and increased risk of damage to organs such as the heart and brain
- Management includes iron and vitamin supplements, erythropoietin injections, and dietary adjustments
Bone Weakness
CKD impairs the regulation of calcium and phosphorus, resulting in low blood calcium and high blood phosphorus (hyperphosphatemia). This imbalance increases the risk of bone fractures and bone pain, and may present early as muscle spasms or skin sensations.
- Weakening bones subject to fractures
- Symptoms: muscle spasms, numbness or tingling, itching
- Management includes calcium and vitamin D supplementation, phosphate binders, and dietary modifications
Fluid Retention
Impaired filtration can cause the body to retain excess fluids, resulting in edema (swelling of limbs), fluid accumulation in the lungs (pulmonary edema), and increased blood pressure. Severe cases can be life-threatening.
- Swelling in arms, legs, and around the eyes
- High blood pressure, shortness of breath, and fluid in lungs
- Controlled by salt and fluid intake restrictions and prescribed medications
Gout
Gout is a form of arthritis arising from uric acid buildup in the joints—a process normally regulated by healthy kidneys. CKD disrupts uric acid elimination, increasing the risk of painful gout attacks.
- Causes joint pain, swelling, and inflammation
- Triggered by high-purine foods: bacon, turkey, fish, dried beans, peas
- Management through diet modification and medications prescribed by a healthcare professional
Heart Disease & High Blood Pressure
CKD and cardiovascular disease are closely intertwined. Fluid retention and hormonal imbalances in CKD amplify high blood pressure (hypertension), which in turn worsens kidney damage and heightens heart disease risk. CKD can also lead to congestive heart failure.
- High blood pressure can further damage kidneys
- Heart disease risk increases due to arterial stiffness, inflammation, and fluid overload
| Complication | Key Symptoms | CKD Link |
|---|---|---|
| Anemia | Fatigue, pallor | Low EPO, nutrient deficiencies |
| Bone Weakness | Bone pain, fractures | Low calcium, high phosphorus |
| Fluid Retention | Edema, breathlessness | Impaired fluid filtration |
| Gout | Joint pain, redness | Uric acid buildup |
| Heart Disease | Chest pain, fatigue | Hypertension, fluid overload |
| Hyperkalemia | Irregular heartbeat | High potassium levels |
Hyperkalemia (High Potassium Levels)
As CKD impairs the kidneys’ ability to filter potassium, levels can dangerously accumulate in the blood. Hyperkalemia may cause muscle weakness, fatigue, and in severe instances, life-threatening heart rhythm disturbances.
- Signs include irregular heartbeat, muscle cramps
- Dietary potassium restrictions and medications may be necessary
Neurological Complications
CKD increases the likelihood of various neurological problems, particularly for those with end-stage renal disease or undergoing dialysis. However, dysfunction can occur at any CKD stage.
- Cognitive impairment and dementia
- Stroke (ischemic, hemorrhagic, or silent)
- Movement disorders, including Parkinson’s disease
- Seizures
These issues stem from changes in blood chemistry, vascular damage, and toxin buildup that impact the brain and nervous system.
Secondary Complications
- Depression: Chronic illness and lifestyle changes can contribute to depressive symptoms. Nearly 60% of CKD patients may experience depression.
- Skin infections: CKD often causes dry, itchy skin, increasing vulnerability to infections.
- Joint, bone, and muscle pain: Caused by electrolyte imbalances and metabolic disturbances.
- Nerve damage
- Pleural effusion: Buildup of fluid around the lungs
- Liver failure
- Sleep disorders
Preventing Complications
CKD cannot be cured, but progression and complications can be managed and sometimes delayed. Prevention involves coordinated care and self-management strategies:
- Regular blood and urine tests: Monitoring kidney health with eGFR, BUN, creatinine, and urine albumin
- Management of health concerns: Controlling diabetes, cholesterol, and weight
- Dietary guidance: Consulting with a dietitian to maintain proper nutrition
- Exercise: Engaging in physical activity appropriate for individual capability
- Weight maintenance: Maintaining a moderate, healthy weight
- Sleep hygiene: 7–8 hours per night
- Avoidance of smoking and secondhand smoke
- Stress and mental health management: Developing coping mechanisms for stress, anxiety, and depression
- Medication compliance: Taking prescribed medications as directed
- Caution with over-the-counter medicines: Especially NSAIDs and others that may affect kidney function
Treatment Options for CKD Complications
Treatment for CKD and related complications aims to slow disease progression, manage symptoms, and prevent further issues.
- Diet changes: Patients are advised to lower intake of salt, protein, potassium, and fat. For patients with diabetes, carbohydrate management is also important. Ensuring adequate calorie intake maintains healthy weight.
- Lifestyle modifications: Routine exercise, smoking cessation, and stress management contribute to overall health and reduce compounding risk factors.
- Supplements and medications:
- Iron, vitamin B12, and folic acid to treat anemia
- Calcium and vitamin D to strengthen bones
- Erythropoietin injections to promote red blood cell formation
- Phosphate binders to lower blood phosphorus
- Antihistamines for itching
- Medical management:
- Dialysis: Artificially cleanses blood when kidneys fail
- Kidney transplant: Offers longest-term solution for end-stage renal disease
- Infection precautions: Vaccinations recommended include pneumococcal, hepatitis B, and influenza vaccines
CKD Risk Factors and Management
- Diabetes
- High blood pressure
- Heart disease
- Obesity
- Smoking
- Family history of kidney disease
- Increasing age
- Frequent medication use (especially nephrotoxic drugs)
Managing these risk factors by adhering to medical advice and self-care strategies is vital to limiting CKD progression and complications.
Frequently Asked Questions (FAQs)
Q: Why does CKD cause anemia?
A: CKD reduces erythropoietin (EPO) production, a hormone required for red blood cell formation. Nutritional deficiencies also contribute.
Q: How can I prevent bone issues related to CKD?
A: Maintaining proper calcium and phosphorus levels through diet, supplements, and medication as recommended by your doctor is essential.
Q: Is fluid retention dangerous?
A: Yes, excessive fluid accumulation can lead to high blood pressure, swelling, and even fluid in the lungs, making it a critical complication to manage.
Q: Can CKD increase my risk for neurological disorders?
A: Yes, CKD heightens the risk for strokes, cognitive impairment, and movement disorders due to changes in blood chemistry and vascular damage.
Q: What are recommended lifestyle changes for living with CKD?
A: Routine checkups, balanced nutrition, exercise, weight management, avoiding tobacco, and stress reduction are important steps in managing CKD.
Key Takeaways and Next Steps
CKD complications are numerous and interrelated, affecting the quality of life and overall health. Prevention and management through coordinated healthcare, careful monitoring, and patient self-care are fundamental. If you or someone you know is living with CKD, regular communication with healthcare professionals and early intervention are essential to controlling complications and maintaining well-being.
References
- https://www.healthline.com/health/kidney-disease/complications-of-chronic-kidney-disease
- https://www.healthline.com/health/chronic-kidney-disease
- https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/symptoms-causes/syc-20354521
- https://www.medicalnewstoday.com/articles/172179
- https://www.healthline.com/health/video/ckd-stages
- https://www.healthline.com/health/video/foods-to-avoid-with-kidney-disease
- https://globalhealth.washington.edu/news/2017/04/13/healthline-effects-kidney-disease-cardiovascular-health
- https://my.clevelandclinic.org/health/diseases/15096-chronic-kidney-disease
- https://www.uc.edu/news/articles/legacy/healthnews/2007/02/uc-health-line–multidisciplinary-team-focuses-on-preventing-diabetic-kidney-failure.html
Read full bio of Sneha Tete












