Cognitive Behavioral Therapy for Insomnia: A Comprehensive Guide
Explore how cognitive behavioral therapy for insomnia transforms sleep patterns and improves overall wellbeing
Insomnia affects millions of adults worldwide, profoundly impacting daytime functioning and overall health. As research has progressed, cognitive behavioral therapy for insomnia (CBT-I) has emerged as the most effective and safest treatment for persistent sleep issues, often preferred over medication. This guide will walk you through what CBT-I is, how it works, how long it takes, the techniques involved, and how it compares with medications. Additionally, practical relaxation strategies and frequently asked questions will help enrich your understanding of this evidence-based approach.
What Is Cognitive Behavioral Therapy for Insomnia?
Cognitive behavioral therapy (CBT) is a form of talk therapy that helps individuals identify and reshape problematic thoughts and behaviors. When tailored for insomnia, CBT-I specifically targets sleep-related challenges, aiming to:
- Address negative patterns of thinking about sleep
- Replace sleep anxiety with more positive expectations
- Modify behaviors contributing to poor sleep
While CBT covers a spectrum of mental health issues such as anxiety, depression, and eating disorders, CBT-I focuses on insomnia by reframing maladaptive beliefs about sleep and fortifying behaviors that foster restful nights.
Prevalence and Burden of Insomnia
- Approximately 30% of adults report symptoms of insomnia.
- Chronic insomnia (lasting at least three months, 3+ nights per week) affects around 10% of adults.
- Risks include impaired mental health, cardiovascular disease, diabetes, and reduced quality of life.
CBT-I: Core Components and Process
CBT-I blends several psychological and behavioral strategies to disrupt the cycle of insomnia. Key components include:
- Sleep Restriction Therapy: Limits time in bed to actual sleep duration, gradually increasing it as sleep efficiency improves.
- Stimulus Control Therapy: Strengthens the association between bed and sleep by guiding behaviors (e.g., only going to bed when sleepy, leaving the bed when awake for more than 20 minutes).
- Sleep Hygiene Education: Provides tips and routines to create an optimal sleep environment (e.g., limiting caffeine, maintaining consistent schedules).
- Cognitive Restructuring: Challenges and reshapes inaccurate fears and beliefs about sleep.
- Relaxation Training: Employs techniques to reduce physical and mental hyperarousal before bedtime.
CBT-I Session Structure
CBT-I typically includes 4 to 12 weekly sessions, each lasting about an hour. Sessions may be delivered:
- One-to-one with a therapist
- Group settings
- Remotely via video or phone
- Digital modules or self-help books
Modern research confirms that web-based and digital CBT-I options can match the effectiveness of face-to-face therapy, providing accessibility for many.
How CBT-I Works: The Psychological Approach
| CBT-I Component | Main Objective | Example Technique |
|---|---|---|
| Cognitive Restructuring | Reduce sleep-related anxiety and negative thinking | Identifying exaggerated beliefs (‘I’ll never sleep’) and replacing them with realistic expectations |
| Behavioral Modification | Break habits that worsen insomnia | Adopting a consistent bedtime routine |
| Stimulus Control | Strengthen bed-sleep connection | Getting out of bed if not sleeping within 20 minutes |
| Sleep Restriction | Increase sleep efficiency gradually | Limiting time in bed initially, then titrating up |
| Sleep Hygiene | Optimize sleep environment and habits | Avoiding screen use before bed |
CBT-I Timeline: How Long Does It Take?
For most adults, meaningful improvement begins within 4 to 12 weeks. Adherence to scheduled sessions and techniques is crucial for lasting benefits. Group therapy and digital options allow patients to progress flexibly, though commitment remains key.
CBT-I vs. Medications: Evidence and Recommendations
- CBT-I is endorsed as the main treatment for chronic insomnia by the American College of Physicians.
- Medicines might be indicated for short-term use only if CBT-I alone is insufficient.
- CBT-I provides comparable efficacy to medications with fewer side effects and lower risk of dependence.
- Long-term use of sleep medication can lead to tolerance, dependence, and adverse effects.
Comparative Benefits: CBT-I vs. Pharmaceuticals
| Criteria | CBT-I | Medications |
|---|---|---|
| Long-term efficacy | High, with sustained improvements | Can decline as tolerance develops |
| Side effects | Minimal, mainly commitment and effort | Possible drowsiness, dependence, withdrawal |
| Risk of misuse | Low | Medium to high |
| Recommended for chronic insomnia | Yes (first-line) | Occasionally (short-term) |
Techniques to Relax: Enhancing CBT-I
CBT-I frequently incorporates relaxation strategies to decrease nighttime tension and racing thoughts. Recommended methods include:
- Meditation: Mindfulness exercises to quiet the mind before sleep.
- Progressive muscle relaxation: Targeting muscle groups to unwind physical tension.
- Biofeedback: Using devices or apps to monitor and control physiological stress markers.
- Bedtime yoga: Gentle poses to slow breathing and promote comfort.
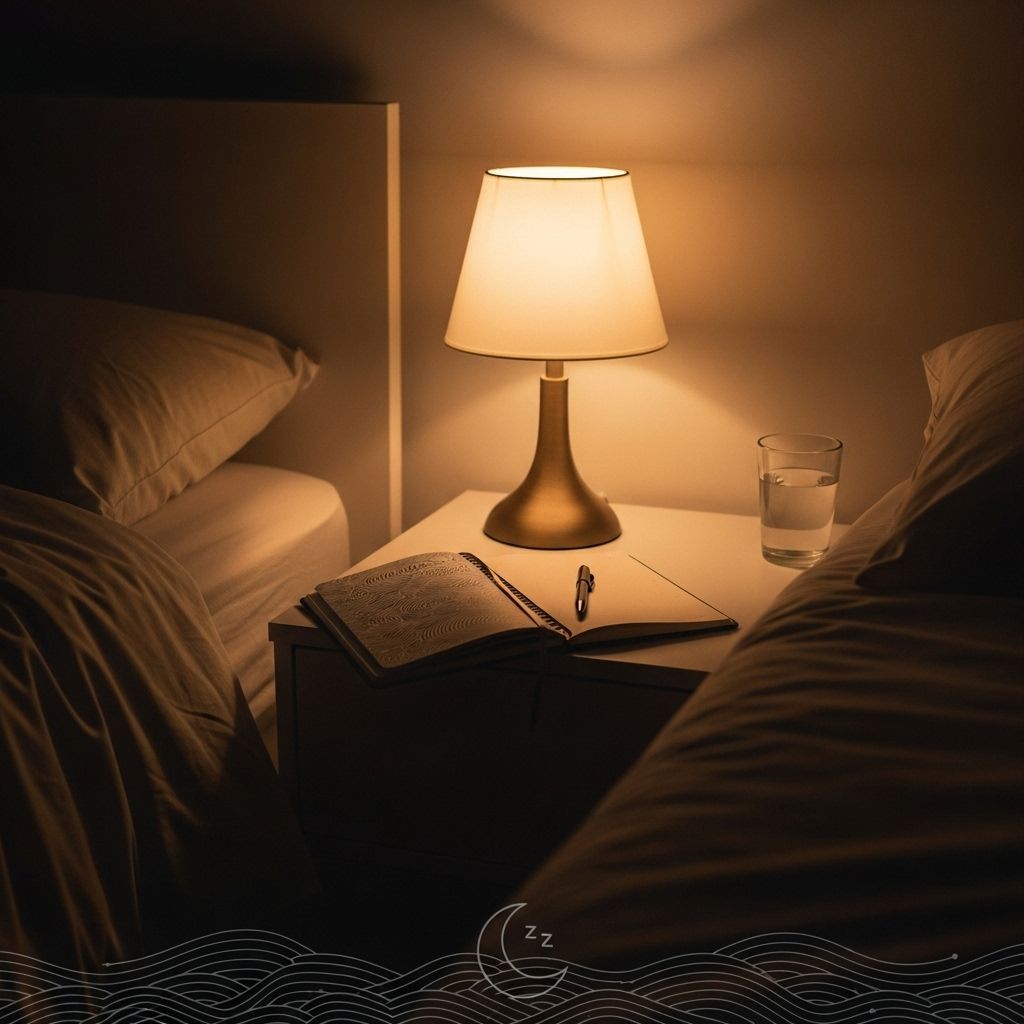
Scheduling a nightly wind-down period—a “buffer zone” between daily stresses and bedtime—helps the body transition to sleep readiness.
Integrating Relaxation into Sleep Hygiene
- Listen to soothing music
- Use guided meditation apps
- Practice slow, deep breathing exercises
Who Can Benefit from CBT-I?
- Individuals with chronic insomnia
- Those suffering sleep-related anxiety
- People with co-occurring mental health challenges (depression, anxiety)
- Anyone unable to sustain sleep through medication alone
CBT-I: Scientific Evidence and Outcomes
- CBT-I yields moderate to large and durable improvements in sleep quality, latency (time to sleep), sleep efficiency, and wake time after sleep onset.
- Digital CBT-I (dCBT) platforms further increase access, showing similar efficacy for both nighttime and daytime symptoms of insomnia.
- Improved sleep also mediates better functional health, psychological wellbeing, and relationships.
Meta-analyses consistently show CBT-I is the gold standard, outperforming other interventions on most insomnia metrics over time.
Frequently Asked Questions (FAQs)
Q: What is the goal of cognitive behavioral therapy for insomnia?
A: CBT-I aims to change both negative thinking patterns and unhelpful behaviors that perpetuate insomnia, establishing a healthier sleep mindset and routine.
Q: How many sessions does CBT-I require?
A: Most individuals experience strong improvements after 4–12 one-hour weekly sessions. Some may benefit from shorter or longer therapy, based on severity.
Q: Are relaxation techniques required or optional in CBT-I?
A: While not mandatory, relaxation, such as meditation or progressive muscle relaxation, is highly recommended to boost CBT-I’s effectiveness.
Q: Can CBT-I be done virtually or through self-help books?
A: Yes, web-based modules and self-guided resources have been shown to be just as effective as traditional in-person therapy for many people.
Q: Is CBT-I suitable if I also have depression or anxiety?
A: Absolutely. CBT-I is effective even with co-occurring mental health conditions, especially as it can address overlapping problems.
Key Insights for Sustained Sleep Health
- CBT-I is the first-line, non-drug treatment for chronic insomnia according to leading medical authorities.
- Combining cognitive and behavioral methods maximizes sustained recovery.
- Digital CBT-I offers convenience, privacy, and efficacy comparable to in-person therapy.
- Relaxation, sleep hygiene, and commitment are crucial for lasting success.
If you or someone you know regularly struggles with sleep, CBT-I offers proven, practical solutions. It transforms not just nighttime rest, but daytime mood, performance, and quality of life.
References
- https://www.healthline.com/health/insomnia/cognitive-behavioral-therapy-for-insomnia
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10002474/
- https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2704019
- https://www.healthline.com/health/healthy-sleep/sleep-restriction-therapy
- https://www.mayoclinic.org/diseases-conditions/insomnia/in-depth/insomnia-treatment/art-20046677
- https://aasm.org/digital-cognitive-behavioral-therapy-for-insomnia-platforms-and-characteristics/
Read full bio of medha deb