Chronic Neutrophilic Leukemia: Causes, Symptoms, Diagnosis, and Treatment
Unraveling the complexities of a rare blood cancer driven by neutrophil overproduction.
Chronic Neutrophilic Leukemia (CNL): Causes, Symptoms, Diagnosis, and Treatment
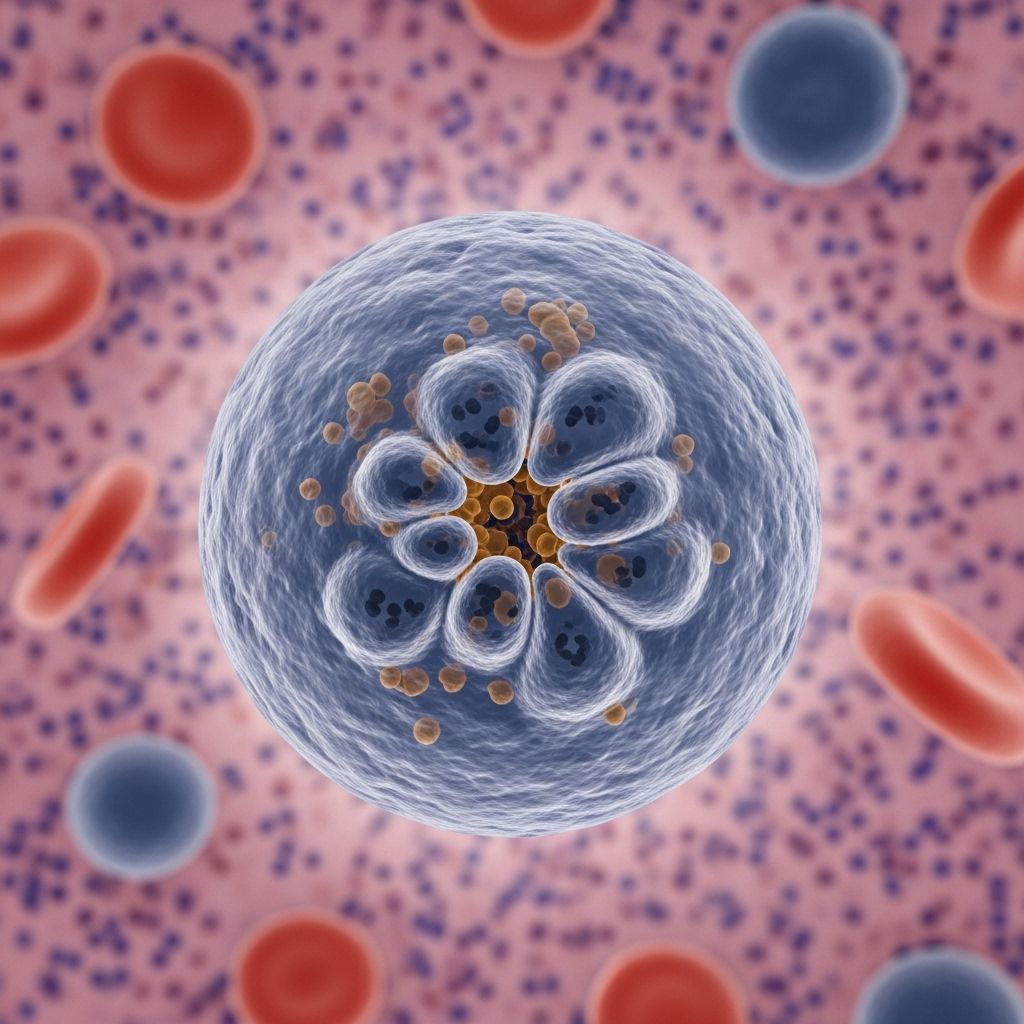
Chronic neutrophilic leukemia (CNL) is a rare hematologic cancer characterized by the uncontrolled proliferation of mature neutrophils, a type of white blood cell crucial for immune defense. CNL belongs to a group of disorders known as myeloproliferative neoplasms (MPNs), in which the bone marrow produces excessive blood cells. Fewer than 300 cases have been reported globally, which presents unique challenges for diagnosis, research, and treatment. This article offers an in-depth overview of CNL, including causes, symptoms, diagnostic procedures, treatment options, prognosis, and frequently asked questions.
What Is Chronic Neutrophilic Leukemia?
CNL is a rare myeloproliferative neoplasm primarily involving the overproduction of mature neutrophils in the bone marrow and peripheral blood. Unlike other leukemias, CNL typically progresses slowly and may remain asymptomatic for years. However, over time, an excessive number of neutrophils can disrupt normal blood function and cause systemic symptoms.
- Category: Blood cancer (leukemia), specifically myeloproliferative neoplasm.
- Prevalence: Exceptionally rare, with slightly over 200 confirmed cases worldwide.
Symptoms of Chronic Neutrophilic Leukemia
CNL often goes unnoticed in its early phase, as many individuals may show no symptoms. When present, symptoms are generally the result of elevated neutrophil counts and their effect on blood and organ systems.
Common Symptoms
- Fatigue — feeling persistently tired or weak even after rest
- Easy bruising or bleeding — often due to abnormal platelet function
- Splenomegaly — enlarged spleen, sometimes causing discomfort or a feeling of fullness in the left upper abdomen
- Pruritus (itching)
- Abdominal discomfort
- Unexplained weight loss
- Night sweats
- Mild bone pain
Less commonly, CNL can present with skin changes (such as rashes or lesions), fevers, and symptoms from increased blood viscosity. In rare cases, severe hemorrhagic events such as epistaxis (nosebleeds), gastrointestinal bleeding, or even intracranial hemorrhages can occur. Some patients experience hyperuricemia (excess uric acid), leading to gout or kidney stones, and others may report easy bruising not explained by trauma or medications.
Causes and Risk Factors
Genetic Mutations
Most cases of CNL are linked to somatic mutations, particularly in the CSF3R gene (colony-stimulating factor 3 receptor). The most well-studied mutation is CSF3R T618I, found in the majority of CNL patients. This genetic fault causes stem cells in the bone marrow to produce excessive neutrophils that do not function normally.
- CSF3R mutations: Strong diagnostic marker for CNL; present in 80–90% of patients.
- Other mutations: Recent research has identified additional, less common mutations in other genes (such as SETBP1, ASXL1, and SRSF2) in some patients.
Unknown Primary Cause
The exact cause of CNL remains unknown. Most cases arise sporadically, with no hereditary component. Environmental or lifestyle risk factors have not been conclusively identified due to the disease’s rarity.
Known Risk Factors
- No established risk factors due to limited case numbers
- Higher prevalence in older adults, typically diagnosed later in life
- Very rare under age 40; majority diagnosed between 60–80 years
- No known association with gender, ethnicity, or lifestyle
How Is Chronic Neutrophilic Leukemia Diagnosed?
Diagnosing CNL is challenging and often requires ruling out other causes of neutrophilia, such as infections or other myeloproliferative disorders. The diagnosis relies on clinical findings, laboratory results, and genetic testing.
Key Steps in Diagnosis
- History and Physical Exam: Identification of symptoms such as fatigue, splenomegaly, or bruising. Examination may reveal an enlarged spleen or, rarely, liver.
- Blood Tests:
- Markedly elevated white blood cell (WBC) count, primarily mature neutrophils
- Occasional anemia (low red blood cell count)
- Platelet counts may be normal or reduced
- Elevated uric acid and lactate dehydrogenase (LDH) levels in some cases
- Peripheral Blood Smear: Shows mature neutrophilia without significant numbers of immature white cells (blasts).
- Bone Marrow Biopsy: Helps confirm excessive neutrophil production, infiltration of bone marrow, and to evaluate for fibrosis or dysplasia.
- Genetic and Molecular Testing: Screening for CSF3R mutations and exclusion of BCR-ABL1 fusion gene (which would indicate chronic myeloid leukemia instead).
Differential Diagnosis
It is crucial to distinguish CNL from other causes of sustained neutrophilia, including:
- Chronic myeloid leukemia (CML)
- Other myeloproliferative neoplasms (e.g., polycythemia vera, essential thrombocythemia, primary myelofibrosis)
- Reactive neutrophilia from infections or inflammation
- Other hematologic malignancies
Treatment Options for Chronic Neutrophilic Leukemia
There is currently no standard or universally accepted treatment protocol for CNL. Therapy is typically individualized and guided by symptoms, disease progression, genetic profile, and overall health status.
Common Treatment Approaches
- Cytoreductive therapy: Medications such as hydroxyurea are used to reduce white blood cell counts and alleviate symptoms. Hydroxyurea is considered the mainstay in symptomatic or high-burden cases.
- Targeted therapy: Agents targeting specific genetic mutations, such as JAK inhibitors (e.g., ruxolitinib), have shown some benefit, especially in those harboring CSF3R mutations. However, no targeted therapy is currently FDA-approved specifically for CNL.
- Interferon-alpha: May be considered, especially in younger patients or those not tolerating other treatments.
- Allogeneic stem cell transplantation: The only potentially curative option but is associated with significant risks. Reserved for eligible patients with advanced or refractory CNL.
- Supportive care: Includes management of symptoms, prevention of infections, and control of complications such as bleeding or gout.
Experimental and Emerging Treatments
- Clinical trials are ongoing to identify novel treatments, gene therapies, and improved targeted agents.
- Next-generation tyrosine kinase inhibitors are under consideration for select genetic variants.
Prognosis and Outlook
The course of CNL is variable and often chronic but may accelerate or transform into acute leukemia (blast crisis) in rare cases. Prognosis depends on several factors:
- Age at diagnosis and general health
- Presence of additional genetic mutations (such as SETBP1 or ASXL1)
- Response to initial therapy
- Severity of symptoms or complications (such as infections, bleeding, or transformation to acute myeloid leukemia)
Early detection and appropriate management can help improve quality of life. Many patients have stable disease for years, while others face a more aggressive progression.
Living With Chronic Neutrophilic Leukemia
Because CNL is so rare, few support groups exist, but connecting with patient networks for rare blood cancers or myeloproliferative disorders can provide valuable information and emotional support.
Tips for Managing CNL
- Adhere strictly to scheduled medical appointments and lab tests
- Report new symptoms, especially fever, bleeding, or pain, to your healthcare provider promptly
- Ask about genetic counseling if you have questions about family risk
- Consider clinical trial enrollment if standard treatments are not effective
- Practice infection prevention, as neutrophil dysfunction may increase risk
Frequently Asked Questions (FAQ)
What are the main symptoms of chronic neutrophilic leukemia?
Fatigue, easy bruising or bleeding, splenomegaly (enlarged spleen), itching, abdominal discomfort, weight loss, night sweats, and mild bone pain are common symptoms. Some patients may experience frequent infections or gout due to high uric acid levels.
Is chronic neutrophilic leukemia hereditary?
No, CNL is not considered hereditary. Most cases are linked to spontaneous mutations in the CSF3R gene that occur during a person’s lifetime rather than being inherited from family members.
How rare is CNL?
It is exceptionally rare, with just over 200 cases reported worldwide since the first description. This rarity complicates research, diagnosis, and the development of evidence-based therapies.
Does CNL always require immediate treatment?
No. Some cases with mild symptoms may be monitored without immediate intervention. Treatment is typically started only if symptoms develop, blood counts rise significantly, or complications occur.
What is the outlook for people with CNL?
The outlook is highly variable. Some people live with relatively stable disease for years, while others may develop complications or transformation to acute leukemia. Prognosis is influenced by age, mutation profile, and response to treatment.
Summary Table: CNL at a Glance
| Aspect | Details |
|---|---|
| Disease Category | Myeloproliferative neoplasm (MPN) |
| Key Cell Type | Neutrophils (mature white blood cells) |
| Genetic Association | CSF3R mutation (esp. T618I) |
| Most Common Symptoms | Fatigue, bruising, enlarged spleen, bone pain |
| Standard Treatment | No standard; hydroxyurea, targeted therapies, or stem cell transplant |
| Potential Complications | Bleeding, infections, evolution to acute leukemia |
| Prognosis | Variable; ranges from indolent to aggressive |
References and Support
- Discuss diagnosis and management with a hematologist experienced in myeloproliferative neoplasms.
- Access reputable sources, such as national leukemia foundations and cancer support organizations, for further information and community support.
References
- https://healthtree.org/chronic-neutrophilic-leukemia/community/what-are-the-signs-and-symptoms-of-chronic-neutrophilic-leukemia
- https://www.medicalnewstoday.com/articles/chronic-neutrophilic-leukemia
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9048254/
- https://www.healthline.com/health/leukemia/chronic-neutrophilic-leukemia
- https://silvermpncenter.weill.cornell.edu/patients/conditions-and-complications/chronic-neutrophilic-leukemia
- https://www.myleukemiateam.com/resources/chronic-neutrophilic-leukemia-an-overview
- https://my.clevelandclinic.org/health/diseases/22367-neutrophilia
- https://mpn-hub.com/medical-information/chronic-neutrophilic-leukemia-a-2022-update-on-this-rare-disease-and-its-management
- https://lls.org/sites/default/files/2022-03/FS30_CNL_2022_0.pdf
Read full bio of medha deb