Understanding Chronic Neutrophilic Leukemia: Symptoms, Diagnosis, and Treatment
Discover the rare blood cancer, chronic neutrophilic leukemia—its symptoms, genetic roots, diagnosis, and evolving treatments.
What to Know About Chronic Neutrophilic Leukemia (CNL)
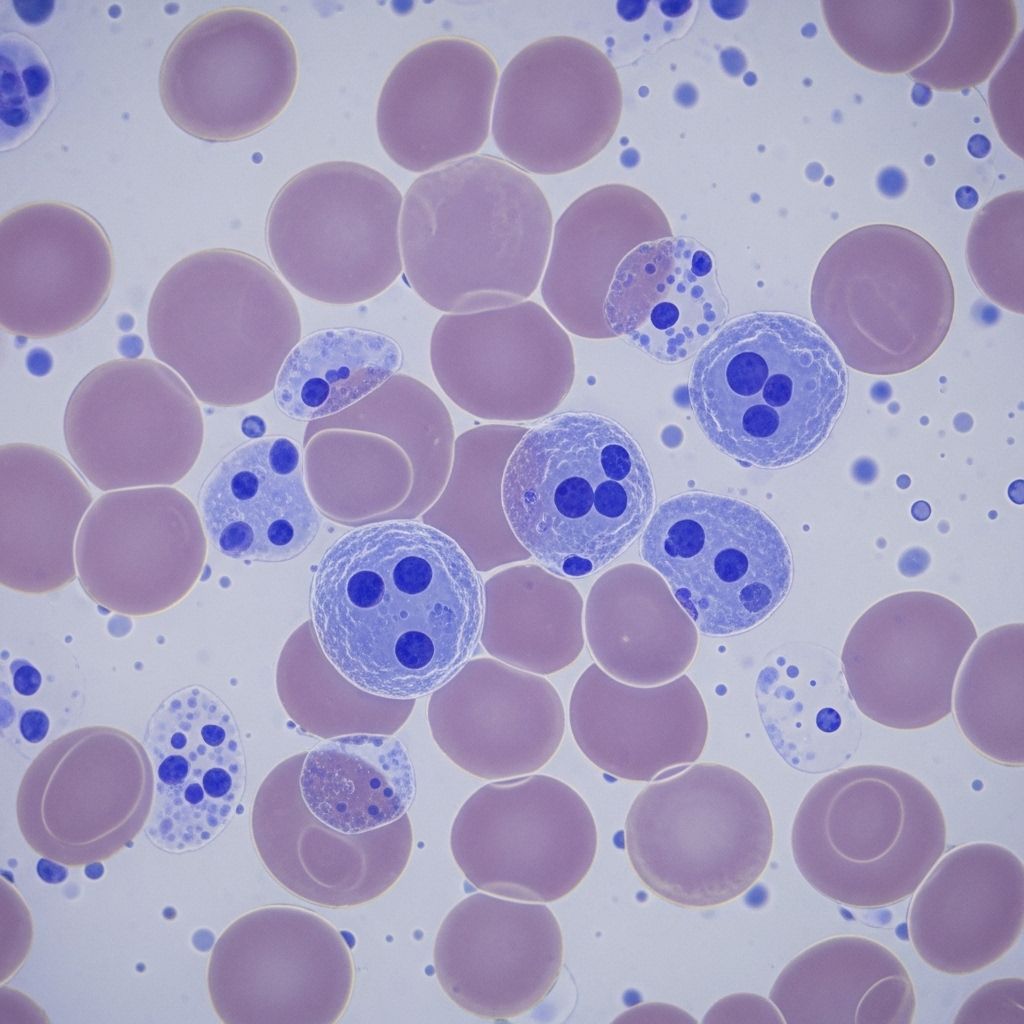
Chronic neutrophilic leukemia (CNL) is a rare, slow-developing cancer of the blood characterized by the abnormal overproduction of mature neutrophils, a specific type of white blood cell. CNL falls under the group of disorders known as myeloproliferative neoplasms (MPNs), with only slightly more than 200 documented cases worldwide. This rarity complicates diagnosis, limits understanding of risk factors, and presents unique challenges for treatment and research advancement.
Although most individuals diagnosed with CNL have no identifiable cause, advances in genetics have linked the disease to distinct mutations. Understanding its symptoms, diagnostic process, treatment options, and outlook can help patients, caregivers, and clinicians navigate this complex disorder more effectively.
What Is Chronic Neutrophilic Leukemia?
CNL is a rare myeloproliferative cancer where the bone marrow produces an abnormally high number of mature neutrophils. These cells, normally essential for defending against infection, proliferate unchecked, disrupting regular blood production and function.
- Category: Myeloproliferative neoplasm (MPN)
- Cells affected: Mature neutrophils (a type of white blood cell)
- Key characteristic: Persistent neutrophilia (excess neutrophils in the blood)
- Prevalence: Extremely rare (~200 reported cases globally)
Unlike acute leukemias, CNL typically follows a slower course, though it may progress to more aggressive disease. The central feature is the sustained overproduction of mature neutrophils in both the bone marrow and bloodstream, without the presence of significant numbers of immature cells (blasts).
Symptoms of Chronic Neutrophilic Leukemia
CNL often presents with no symptoms in its early stages. As the neutrophil count rises and the disease progresses, a range of symptoms may emerge. These can be subtle, non-specific, and overlap with other blood or systemic conditions:
- Fatigue: Feelings of persistent tiredness, even after rest.
- Easy bruising or bleeding: Unexplained bruises or bleeding, possibly due to abnormal platelet function.
- Splenomegaly: Enlarged spleen, sometimes causing abdominal discomfort or a sense of fullness on the left side.
- Pruritus (itchiness): Itching may be present in some cases.
- Abdominal discomfort: Often related to splenomegaly.
- Unintentional weight loss: Reduction in body weight without purposeful dieting or exercise.
- Night sweats: Excessive sweating during sleep.
- Mild bone pain: Particularly as the marrow becomes overpopulated with neutrophils.
- Fever: Occasionally seen, usually low-grade and persistent in advanced disease.
- Recurrent infections: Despite the abundance of neutrophils, their function may be compromised.
Some people may also report general malaise, headaches, or skin changes (such as rashes). In rare advanced cases, serious bleeding (including nosebleeds or gastrointestinal bleeding) and skin lesions related to vasculitis may develop.
Early detection is challenging and the diagnosis is frequently made incidentally during routine blood tests or investigation for unexplained symptoms.
Causes and Risk Factors
The precise cause of CNL is unknown. However, the disorder has been closely linked to genetic mutations in the CSF3R gene. The CSF3R gene provides instructions for the colony-stimulating factor 3 receptor, a protein that regulates neutrophil production.
- CSF3R T618I mutation: Detected in the majority of CNL cases; considered a diagnostic hallmark.
- Other genetic mutations: Mutations in genes such as SETBP1 or ASXL1 may also be present, potentially impacting disease progression or response to therapy.
There are no established environmental, hereditary, or lifestyle risk factors known to predispose an individual to CNL. Its rarity and the fact that it often appears sporadically (without a family history) complicate efforts to identify definitive risk factors.
Most patients are adults, often older individuals, but CNL can affect adults at various ages and has a slightly higher prevalence among males.
Diagnosis of Chronic Neutrophilic Leukemia
Diagnosing CNL requires a detailed evaluation to exclude other causes of high neutrophil counts (such as infection, inflammation, or other cancers). The process typically involves:
- Clinical examination: Physicians may note splenomegaly, bruising, or infection.
- Comprehensive blood counts: Reveal persistently elevated neutrophil levels, with mature neutrophils comprising most of the white blood cells.
- Blood smear: Shows rare or absent immature cells (blasts), with mostly mature-appearing neutrophils.
- Bone marrow biopsy: Key for confirming the diagnosis. Shows hypercellularity with increased mature neutrophils, no significant blast infiltration.
- Genetic testing: Detects mutations in the CSF3R gene and rules out mutations characteristic of other myeloproliferative disorders.
- Exclusion of other conditions: Necessary to rule out chronic myeloid leukemia (CML), chronic myelomonocytic leukemia (CMML), and infections or inflammatory processes.
Table 1: Key Features to Distinguish CNL
| Condition | Main Blood Findings | Genetic Markers |
|---|---|---|
| Chronic Neutrophilic Leukemia (CNL) | Persistent mature neutrophilia | CSF3R mutation (esp. T618I) |
| Chronic Myeloid Leukemia (CML) | Mixed myeloid cell excess (including blasts, basophils, eosinophils) | BCR-ABL fusion gene (Philadelphia chromosome) |
| Infections/Inflammatory Diseases | Neutrophilia (usually transient), other inflammatory markers | None |
Molecular testing for CSF3R mutations is now central to the diagnosis of CNL and helps differentiate it from other causes of high neutrophil counts.
Treatment Options for Chronic Neutrophilic Leukemia
There is no universally established standard treatment for CNL due to its rarity and variability among patients. Treatment is often individualized and may depend on disease severity, patient age, symptoms, underlying genetic mutations, and other health conditions.
Common Treatment Options
- Hydroxyurea: A chemotherapy medication that reduces blood cell counts, often used first-line to control neutrophil proliferation and manage symptoms.
- Interferon-alpha: Sometimes prescribed, especially in younger patients, for its effect on bone marrow activity.
- Leukapheresis: A procedure occasionally used to rapidly lower very high white blood cell counts in emergencies.
- Supportive care: Includes antibiotics for infections, transfusions for anemia or bleeding, and uric acid-lowering agents for gout.
- Targeted therapies: New drugs targeting specific mutations, such as JAK inhibitors (e.g., ruxolitinib), are under investigation in clinical trials but remain off-label for routine care.
- Allogeneic stem cell transplantation: The only known curative strategy but rarely pursued due to patient age and high risk.
Treatment aims to reduce symptoms, prevent complications, and enhance quality of life. Many patients may not need immediate treatment if asymptomatic and stable but require close monitoring for disease progression.
Participation in clinical trials is often encouraged as new therapies emerge, especially for those with advanced or treatment-resistant disease.
Prognosis and Outlook
The outlook for CNL varies. Many people experience an indolent or slow disease course, and symptom control is often possible with existing therapies.
- Slow progression: Many patients remain stable for years, with manageable symptoms and good quality of life.
- Disease transformation: In some cases, CNL can transform into acute myeloid leukemia (AML), a faster-growing cancer with poorer prognosis.
- Risk factors for poor outcome: Progression to AML, failure of standard therapies, or additional high-risk mutations (e.g., SETBP1, ASXL1).
Life expectancy varies but can range from several years following diagnosis. Ongoing surveillance with periodic blood tests is essential for adjusting treatment and identifying progression early.
Frequently Asked Questions (FAQs)
Q: What causes chronic neutrophilic leukemia?
A: While the exact cause of CNL remains unknown, most cases are associated with mutations in the CSF3R gene, which regulates neutrophil production. The disease is not known to be hereditary or triggered by environmental or lifestyle factors.
Q: Is CNL contagious or preventable?
A: Chronic neutrophilic leukemia is not contagious, and there are currently no known preventive measures.
Q: What are the early signs of CNL?
A: CNL is often asymptomatic in the early stages. Common signs that develop later may include fatigue, unexplained weight loss, easy bruising or bleeding, splenomegaly (enlarged spleen), and night sweats.
Q: How is CNL different from other leukemias?
A: Unlike acute leukemia or chronic myeloid leukemia (CML), CNL involves an overproduction of mature neutrophils rather than immature cancerous blasts. Its slow progression and unique genetic profile (CSF3R mutation) set it apart.
Q: Are there any new or experimental treatments?
A: Emerging research is exploring targeted therapies—such as JAK inhibitors—especially for patients with certain genetic mutations or treatment-resistant disease. Participation in clinical trials may be an option for eligible patients.
Key Takeaways
- CNL is a very rare form of blood cancer characterized by overproduction of mature neutrophils.
- Most cases are linked to CSF3R gene mutations.
- Symptoms often appear late and include fatigue, bleeding, splenomegaly, and night sweats.
- Diagnosis requires careful genetic and blood testing to exclude other diseases.
- Treatment is individualized but may involve hydroxyurea, interferon-alpha, or stem cell transplantation in selected cases.
- The prognosis varies; regular monitoring and clinical trials are vital for optimal care.
References
- https://healthtree.org/chronic-neutrophilic-leukemia/community/what-are-the-signs-and-symptoms-of-chronic-neutrophilic-leukemia
- https://www.medicalnewstoday.com/articles/chronic-neutrophilic-leukemia
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9048254/
- https://www.healthline.com/health/leukemia/chronic-neutrophilic-leukemia
- https://silvermpncenter.weill.cornell.edu/patients/conditions-and-complications/chronic-neutrophilic-leukemia
- https://www.myleukemiateam.com/resources/chronic-neutrophilic-leukemia-an-overview
- https://my.clevelandclinic.org/health/diseases/22367-neutrophilia
- https://mpn-hub.com/medical-information/chronic-neutrophilic-leukemia-a-2022-update-on-this-rare-disease-and-its-management
- https://lls.org/sites/default/files/2022-03/FS30_CNL_2022_0.pdf
Read full bio of medha deb