Chronic Intestinal Pseudo-Obstruction: Life Expectancy and Prognosis
Understanding longevity, prognosis, and care strategies for people affected by chronic intestinal pseudo-obstruction.
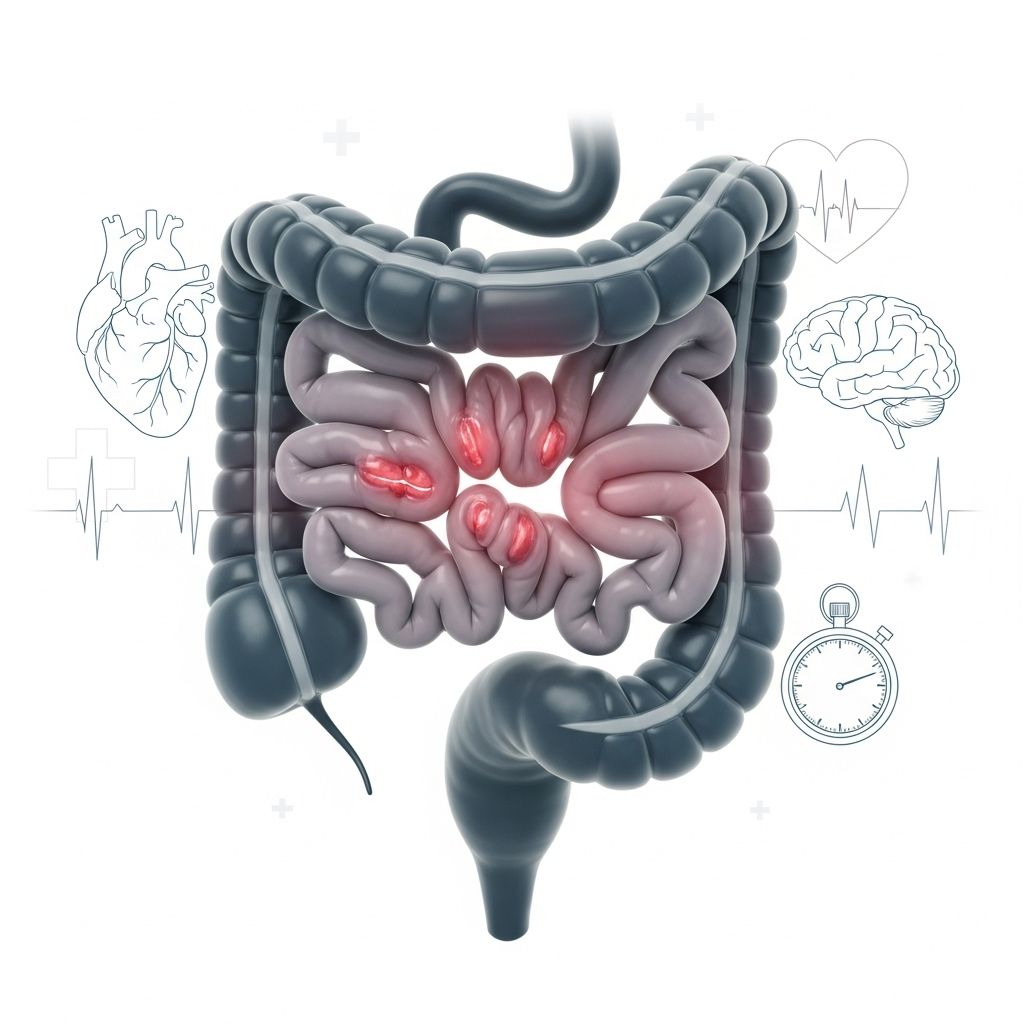
Chronic intestinal pseudo-obstruction (CIPO) is a rare and debilitating disorder affecting the motility of the gastrointestinal tract. It can have a profound impact on nutrition, growth, and life expectancy, especially in infants and children, though adults can also be affected. This article explores what determines the outlook for people with CIPO, how it is managed, and what the latest research reveals about prognosis and survival rates.
What is Chronic Intestinal Pseudo-Obstruction (CIPO)?
CIPO is a disorder where coordinated muscular contractions of the digestive tract fail, mimicking a physical bowel obstruction without any actual blockage. This disrupts the movement of food and waste, resulting in multiple digestive complications. The condition may be caused by defects in the nerves, muscles, or interstitial cells of the intestine and can first appear in infancy, childhood, or adulthood.
- Malnutrition due to poor absorption of nutrients
- Weight loss or failure to thrive in children and infants
- Development of small intestinal bacterial overgrowth (SIBO)
- Progression to intestinal failure, where nutritional support is needed
- Symptoms may include severe bloating, abdominal pain, vomiting, constipation, and distention
How Does CIPO Affect Life Expectancy?
Life expectancy for CIPO is highly variable and influenced by the individual’s age at onset, severity of digestive tract dysfunction, ability to maintain nutrition, and access to specialized treatments like parenteral nutrition (PN) and, in select cases, intestinal transplant. Reliable statistics are limited due to how rare CIPO is, but both clinical experience and research provide insight into survival rates and prognosis:
Survival Rates
A frequently cited study on adults with severe CIPO who required long-term parenteral nutrition found the following actuarial survival rates:
| Time Since Diagnosis | Survival Rate (%) |
|---|---|
| 1 year | 94% |
| 5 years | 78% |
| 10 years | 75% |
| 15 years | 68% |
These numbers suggest that, with effective nutritional support, many adults can live for years after diagnosis, although overall life expectancy is still reduced compared to the general population. For adults, mean survival time may stretch over a decade, particularly with advances in medical care.
Pediatric Survival and Challenges
- Children and infants with CIPO generally have a poorer prognosis than adults.
- Studies report mortality rates as high as 40% in pediatric populations, much of it occurring within the first two years of life due to severe malnutrition, infections, or complications.
- Delayed diagnosis worsens outcomes because early, specialized intervention is critical for preventing life-threatening complications.
What Determines Life Expectancy in CIPO?
Several key factors influence prognosis and overall survival in people diagnosed with CIPO:
- Ability to Maintain Oral Feeding: Individuals who can eat and absorb enough nutrients by mouth tend to have much better long-term outcomes than those requiring ongoing intravenous nutrition.
- Early Diagnosis & Intervention: Early recognition and management may help prevent irreversible complications like liver disease or severe malnutrition.
- Access to Parenteral Nutrition (PN): PN, where nutrients are delivered directly into the bloodstream, can sustain individuals for many years. However, it is associated with serious risks such as bloodstream infections and liver failure.
- Age at Onset: Outcomes are generally more favorable for adults compared to infants and very young children.
- Underlying Health Conditions: Associated diseases (such as autoimmune disorders or neuromuscular syndromes) may worsen the prognosis.
- Infection Risk: Repeated infections, especially related to intravenous catheters for PN, significantly increase the risk of death.
- Complications from Treatment: These include liver dysfunction, short bowel syndrome following surgeries, and other metabolic imbalances.
- Availability of Intestinal Transplant: For select patients, especially those with life-threatening PN complications, intestinal transplantation can improve survival and quality of life.
General Outlook for People with CIPO
The outlook for CIPO varies considerably:
- With treatment (nutritional support, medications, and sometimes surgery), many adults can maintain quality of life and survive beyond ten years after diagnosis.
- Prognosis is poorer in infants and very young children, as severe malnutrition, infections, and complications are more likely.
- Some individuals reach adulthood, particularly if they receive prompt, specialized care and have fewer coexisting conditions.
- Others may die young, especially if the condition is unrecognized, untreated, or complicated by infections or organ failure.
While there is no cure for CIPO, ongoing research is exploring new therapies to improve symptoms and outcomes.
Treatment Options and Impact on Life Expectancy
There is no definitive cure for chronic intestinal pseudo-obstruction, but advances in management have improved both survival and patient well-being.
Management Strategies for CIPO
- Parenteral Nutrition (PN): Long-term intravenous feeding is the mainstay for those unable to absorb enough nutrients through the gut. While it prolongs survival, it requires careful management to reduce infection risk and liver complications.
- Medications: Prokinetic agents may help increase digestive motility. Antibiotics are sometimes used to control bacterial overgrowth in the small intestine.
- Oral or Enteral Feeding: Whenever possible, patients are encouraged to eat or use feeding tubes if at least partial absorption is possible.
- Surgical Interventions: Some may require repeated surgeries for symptom relief or to address complications. However, repeated surgery can result in “short bowel syndrome” which adds new feeding and absorption challenges.
- Intestinal Transplant: For carefully selected individuals with life-threatening complications from PN or severe intestinal failure, transplantation offers a potential solution, though with significant risks.
Complications Associated with CIPO
Because CIPO affects intestinal motility and absorption, it is associated with numerous potential complications:
- Severe malnutrition and vitamin/mineral deficiencies
- Liver disease related to long-term parenteral nutrition
- Catheter-related bloodstream infections in those on intravenous feeding
- Small intestinal bacterial overgrowth (SIBO)
- Short bowel syndrome after multiple surgeries
- Development of kidney stones or gallstones
- Psychosocial stress, anxiety, and depression (quality of life concerns)
Prognosis in Children vs. Adults: A Comparison
| Aspect | Children | Adults |
|---|---|---|
| Typical age at onset | Infancy, early childhood | Usually adulthood, but sometimes young adulthood |
| Mortality Rate | Up to 40% within first years | Approximately 25–32% at 10–15 years |
| Common risk factors for death | Malnutrition, infection, surgical complications | Liver disease, infection, chronic disease (e.g., scleroderma) |
| Improving factors | Early diagnosis, effective nutrition, fewer co-morbidities | Oral feeding possible, few or no autoimmune diseases |
Frequently Asked Questions (FAQs) about CIPO
What causes chronic intestinal pseudo-obstruction?
The cause may be genetic, idiopathic, or secondary to other conditions. In children, birth defects of nerves or muscles in the gut are common causes. In adults, CIPO may be secondary to diseases such as scleroderma, other autoimmune diseases, or neurological conditions.
Can CIPO be cured?
There is currently no cure for CIPO. Treatments primarily focus on improving symptoms, providing adequate nutrition, and reducing complications. Intestinal transplantation may be considered in the most severe cases.
What are the common symptoms of CIPO?
Symptoms may include chronic abdominal pain, severe abdominal bloating, nausea, vomiting, constipation, early feeling of fullness, poor appetite, and failure to thrive (in children).
Who is at risk of having a lower life expectancy with CIPO?
Infants and young children, people with severe malnutrition or liver disease, those with recurring infections, and patients with co-existing major health conditions are at greater risk.
What lifestyle changes can benefit someone with CIPO?
It is important to follow medical advice regarding nutrient intake, maintain good hygiene (especially with intravenous catheters), seek psychosocial support, and have regular monitoring by a multidisciplinary care team.
Does CIPO always lead to intestinal failure?
No, not always. Some individuals can maintain enough digestive function to avoid total intestinal failure, especially if the diagnosis is prompt and they respond well to treatment.
Takeaway: Living with CIPO
Chronic intestinal pseudo-obstruction is a rare, severe disorder with complex management challenges. Its impact on life expectancy and quality of life varies widely according to age, underlying causes, complications, and access to specialized care. Treatment can improve survival and daily functioning but requires a coordinated, long-term approach by a team of experts.
- Early diagnosis, aggressive nutritional support, and careful monitoring for complications are vital regardless of age.
- Prognosis is generally better for adults than young children, though each case is unique.
- There is hope for improved outcomes, as ongoing research aims to develop improved therapies and better transplantation options.
References
- https://www.healthline.com/health/digestive-health/chronic-intestinal-pseudo-obstruction-life-expectancy
- https://pubmed.ncbi.nlm.nih.gov/19367271/
- https://www.jnmjournal.org/journal/view.html?doi=10.5056%2Fjnm22152
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6133590/
- https://en.wikipedia.org/wiki/Intestinal_pseudo-obstruction
- https://www.mountsinai.org/health-library/diseases-conditions/intestinal-pseudo-obstruction
Read full bio of medha deb












