Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP): Symptoms, Diagnosis, and Treatments
CIDP is a treatable neurological disorder causing muscle weakness, sensory loss, and requires prompt diagnosis and management.
Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP): Overview
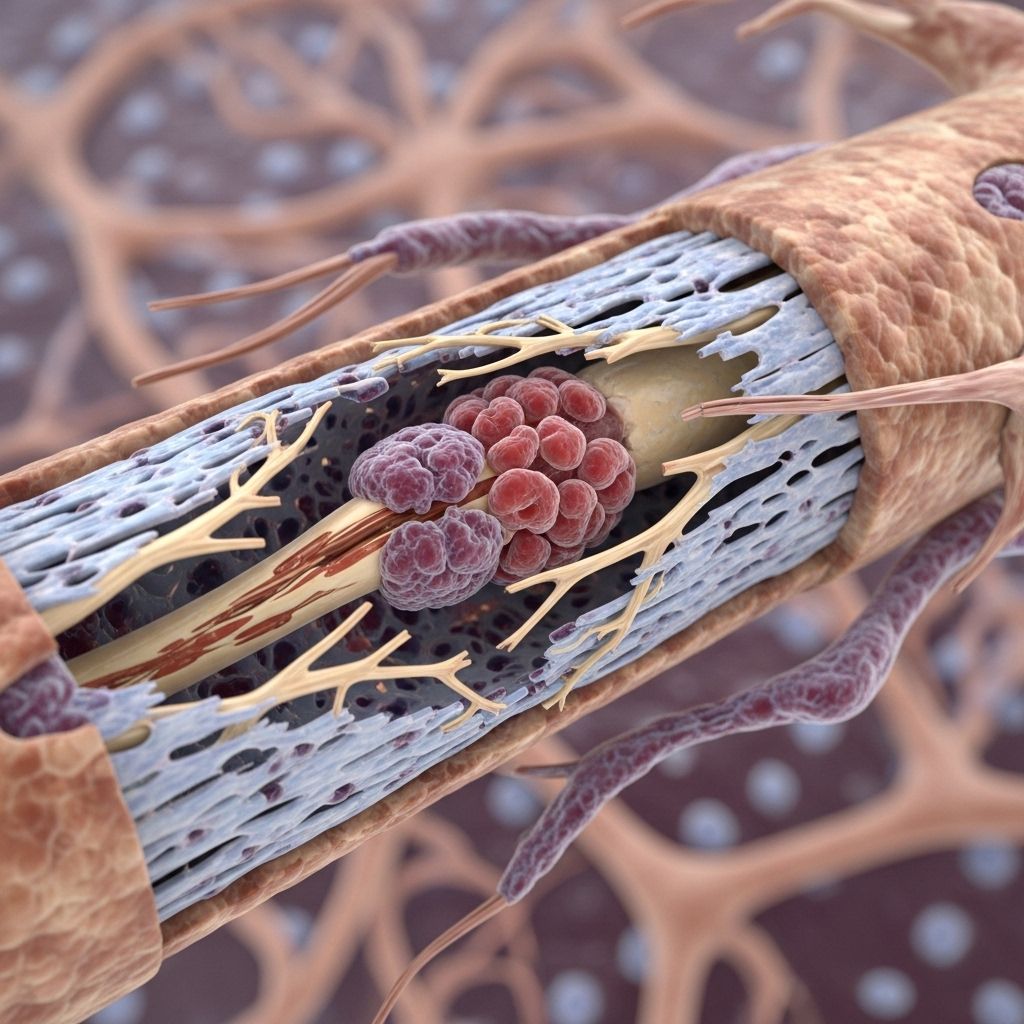
Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP) is a rare autoimmune disorder characterized by progressive weakness and impaired sensory function in the arms and legs. CIDP affects the peripheral nervous system and is marked by the body’s immune system attacking the myelin sheath, which is the protective covering surrounding nerves. This process disrupts the transmission of nerve signals, resulting in substantial neurological symptoms.
CIDP is considered the chronic variant of the acute demyelinating disease Guillain-Barré Syndrome (GBS) and shares similar features, though CIDP develops more gradually and lasts much longer.
What is CIDP?
CIDP is an immune-mediated neurological disorder. The condition involves inflammation of both the nerve roots and peripheral nerves, often leading to progressive muscle weakness and sensory deficits over a period of at least 8 weeks. CIDP can occur in both children and adults, is treatable, and early intervention is recommended to limit permanent nerve damage.
Main Features of CIDP
- Progressive or relapsing weakness and sensory loss in limbs
- Impaired coordination and fine motor skills
- Muscle fatigue and decreased reflexes
- Variable course: monotonic, relapsing, or progressive
Causes and Risk Factors
The precise cause of CIDP is unknown, but it is clear that the body’s immune system mistakenly attacks myelin, the insulating material around nerves. This immune attack is believed to involve multiple pathways, including both humoral and cell-mediated immune mechanisms.
- Autoimmune response: The immune system misidentifies healthy nerve tissue as foreign and damages it.
- Associated conditions: CIDP is sometimes linked to other autoimmune diseases or uncontrolled diabetes.
- Gender and age: CIDP can affect all ages but is slightly more common in men.
Symptoms of CIDP
The hallmark symptoms of CIDP reflect progressive, symmetrical weakness and sensation changes in both arms and legs. Symptoms generally develop over weeks or months, distinguishing CIDP from more acute syndromes such as GBS.
| Symptom | Description |
|---|---|
| Weakness | Gradual, often symmetrical weakness in legs and possibly arms; difficulty rising from chairs, walking, climbing stairs, using hands. |
| Sensory loss | Numbness, tingling, altered sensation starting in feet or hands, progressing upward. |
| Paresthesias | Abnormal sensations such as “pins and needles” or burning. |
| Poor balance | Impaired proprioception and coordination, resulting in frequent falls or unsteady gait. |
| Fatigue | Diffuse muscle fatigue, can be primary (disease-related) or secondary (due to illness impact). |
| Pain | Although less common, some patients experience neuropathic pain or aching muscles. |
| Reflex changes | Loss or decrease in deep tendon reflexes (areflexia). |
| Other disability | Difficulty gripping, tying shoelaces, using utensils, impaired fine motor skills. |
Variants of CIDP Presentation
- Ataxic: Marked problems in balance and coordination.
- Pure sensory: Presents solely with loss of sensation.
- Pure motor: Predominantly muscle weakness.
- Multifocal: Nerve involvement in specific territories causing localized symptoms.
- Atypical patterns: Asymmetric allodynia, painful radiculomyelopathies, cranial nerve involvement.
Diagnosis
Timely and accurate diagnosis of CIDP is essential due to its treatable nature. Diagnosis is primarily clinical but uses several supportive investigations to confirm peripheral nerve involvement and rule out alternative causes.
Key Diagnostic Criteria
- Symptoms lasting over 8 weeks.
- Progressive or relapsing signs including weakness and sensory impairment.
- Electrodiagnostic testing: Nerve conduction studies demonstrating evidence of demyelination, including prolonged or blocked conduction, delayed F-wave, and temporal dispersion.
- Cerebrospinal fluid (CSF) analysis: Increased protein with normal cell count (albumino-cytologic dissociation).
- Imaging: Gadolinium-enhancing hypertrophy of nerves or roots observed in MRI.
- Muscle or nerve biopsy: Evidence of demyelination and remyelination.
Differential Diagnosis
- Toxic, metabolic, infectious, hereditary, or neoplastic neuropathies
- Acute inflammatory demyelinating polyneuropathy (AIDP)
- Multifocal motor neuropathy
- Systemic autoimmune diseases
Treatment Options
Treatment for CIDP focuses on reducing immune-mediated nerve damage. Therapy is most effective when initiated early and is often tailored to the severity and progression of symptoms.
First-Line Treatments
- Intravenous immunoglobulin (IVIG): Regular infusions alter immune response and are often preferred for initial therapy.
- Plasmapheresis: Procedure to remove harmful antibodies from blood.
- Corticosteroids: Oral or intravenous options such as prednisone suppress immune activity.
Other Immunosuppressive Agents
- Mycophenolate mofetil
- Azathioprine
- Cyclophosphamide
- Cyclosporine
- Rituximab (in exceptional cases)
Supportive Therapies
- Physiotherapy: Improves muscle strength, joint mobility, and minimizes contracture development.
- Occupational therapy: Assists with adaptation for daily activities and promotes independence.
- Pain management: Medications or interventions for neuropathic pain, if present.
Complications and Side Effects
- Infusion reactions
- Headache
- Renal impairment or failure
- Infections due to immunosuppression
- Hypercoagulability
Prognosis
The course and recovery in CIDP are highly variable and depend on factors such as age, early intervention, severity, and responsiveness to therapies. Many individuals respond well to treatment, experiencing significant improvements in muscle strength and sensation, while some may be left with partial, permanent deficits.
- Some patients have a single bout with full or partial recovery.
- Others may experience multiple relapses and periods of improvement, requiring adjustments in therapy.
- Persistent symptoms such as weakness or numbness can remain, especially if diagnosis and treatment are delayed.
Aggressive rehabilitation alongside immunomodulatory therapies is instrumental for long-term recovery and maximizing independence.
Living with CIDP: Patient Resources
Given the variable and chronic nature of CIDP, proper support, education, and rehabilitation are crucial for both patients and caregivers.
- Regular follow-up with neurologists
- Access to physiotherapists and occupational therapists
- Guidance for pain management and adaptation to changing mobility or independence
Support Organizations
- GBS/CIDP Foundation International
- GBS Association of NSW
- Local neurology support groups and online communities
Frequently Asked Questions (FAQs)
What is the difference between CIDP and Guillain-Barré Syndrome (GBS)?
CIDP develops over weeks to months and lasts longer, while GBS is a related but acute disease with rapid onset over hours to days. Both involve immune-mediated damage to peripheral nerves and cause similar symptoms, but CIDP is chronic and more treatable with timely intervention.
Can CIDP affect children?
Yes, CIDP can affect people of any age, including children, although it is more common in adults.
Is CIDP curable?
CIDP is considered a treatable cause of acquired neuropathy with many patients achieving substantial improvement. Early diagnosis improves outcomes but some individuals may have lasting symptoms.
What is the most effective treatment for CIDP?
First-line treatments include IVIG infusions, plasmapheresis, and corticosteroids. The best treatment depends on individual response, severity, and side effect profile.
Are there any outpatient support options?
Yes, many organizations offer resources, education, and support for CIDP patients and caregivers, including GBS/CIDP Foundation International and local support networks.
Conclusion
Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP) is a rare, autoimmune neurological disorder requiring early diagnosis and individualized management to maximize patient outcomes. Multidisciplinary care, regular follow-ups, and access to community resources help patients manage the condition and maintain quality of life. Ongoing research continues to improve understanding and develop new treatment approaches for CIDP.
References
- https://en.wikipedia.org/wiki/Chronic_inflammatory_demyelinating_polyneuropathy
- https://www.ncbi.nlm.nih.gov/books/NBK563249/
- https://brainfoundation.org.au/disorders/chronic-inflammatory-demyelinating-polyneuropathy/
- https://my.clevelandclinic.org/health/diseases/cidp-chronic-inflammatory-demyelinating-polyneuropathy
- https://rarediseases.org/rare-diseases/chronic-inflammatory-demyelinating-polyneuropathy/
- https://www.mountsinai.org/health-library/diseases-conditions/chronic-inflammatory-demyelinating-polyneuropathy
- https://www.gbs-cidp.org/cidp/
- https://www.polyneuroexchange.com/cidp
- https://pubmed.ncbi.nlm.nih.gov/38021787/
Read full bio of Sneha Tete












