Congestive Heart Failure and Kidney Disease: Understanding the Connection, Management, and Prognosis
A comprehensive guide to the critical relationship between congestive heart failure and chronic kidney disease, exploring causes, treatment options, and long-term outlook.
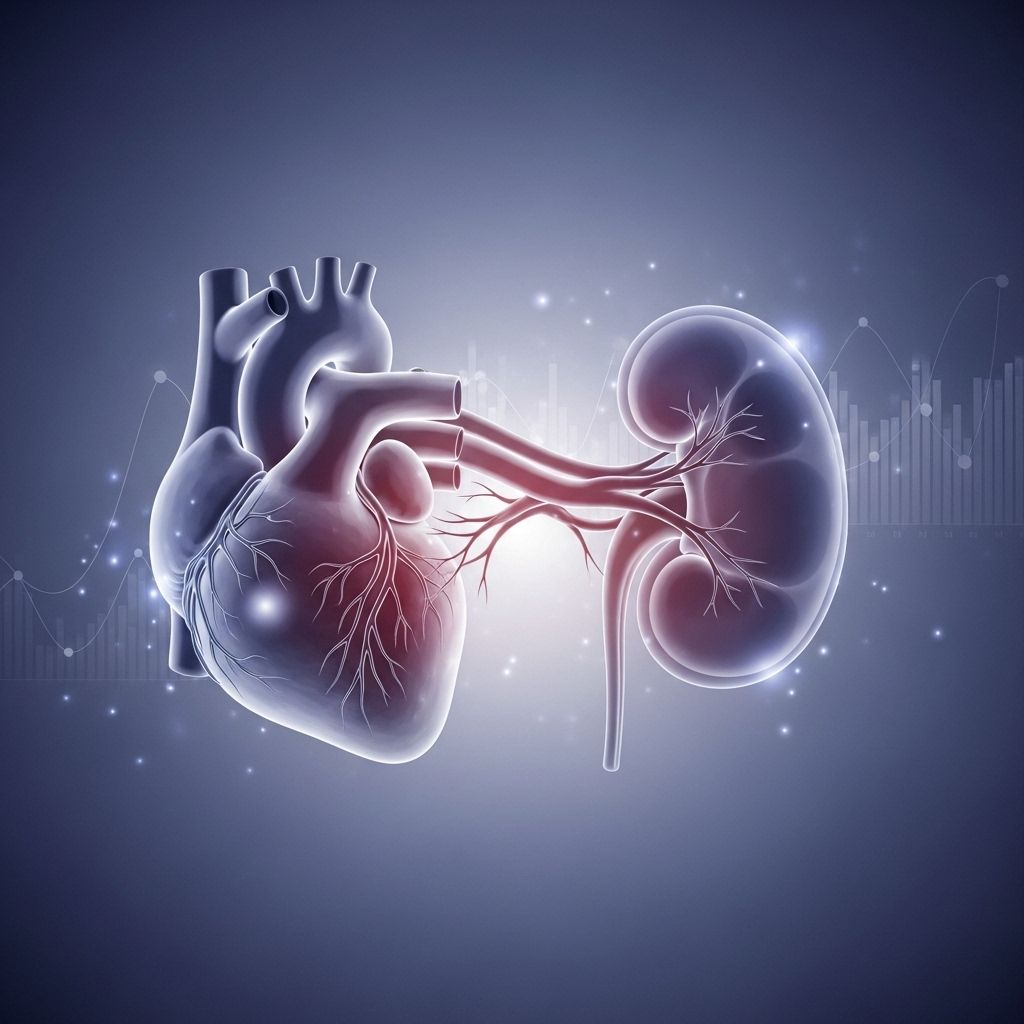
Congestive Heart Failure and Kidney Disease: Why They Often Occur Together
Congestive heart failure (CHF) and chronic kidney disease (CKD) frequently coexist, presenting a dual challenge for those affected. As medical research and clinical observations have shown, the relationship between CHF and kidney disease is bidirectional: heart failure can precipitate kidney dysfunction, and kidney disease can worsen heart failure. Understanding their interconnected nature, risk factors, symptoms, and management options is crucial to improving outcomes for patients and optimizing long-term quality of life.
Both conditions can be managed with medications and lifestyle changes, but severe cases may require invasive treatments such as dialysis or transplants. Early intervention and close collaboration with healthcare providers are key to achieving the best possible prognosis.
What’s the Connection Between CHF and Kidney Disease?
Congestive heart failure develops when the heart is unable to pump enough blood to meet the body’s needs. Common causes and risk factors include:
- Coronary artery disease
- High blood pressure (hypertension)
- Heart valve diseases
- Inherited heart conditions
- Arrhythmias (irregular heartbeat)
- Lack of physical activity
- Excessive substance use (alcohol, drugs)
The kidneys are responsible for filtering waste products and toxins from the bloodstream and maintaining a healthy fluid balance. Kidney disease means the kidneys cannot adequately perform these functions, resulting in hazardous build-up of toxins and retained fluids.
The term “congestive” in CHF refers to fluid buildup in tissues and organs when blood cannot circulate effectively, leading to congestion in the lungs, veins, and other vital tissues.
A Two-Way Relationship
The interplay between CHF and CKD is complex and cyclical:
- CHF reduces the supply of oxygenated blood to the kidneys, impairing their function. This diminished blood flow causes congestion in the veins of organs, including the kidneys, disrupting their ability to filter blood.
- CKD causes fluid and waste retention, increasing blood pressure and straining the heart. Over time, this added burden can compromise the heart’s ability to pump effectively, often resulting in or worsening CHF.
This feedback loop can initiate even in early-stage disease, but the risk of heart failure increases substantially in advanced (stage 4 or 5) CKD.
Both conditions share several major risk factors, most notably:
- Hypertension
- Diabetes
Treatment of CHF becomes more challenging if severe kidney disease is present, as many medications used in CHF may be contraindicated or less effective in impaired kidney function. Additionally, advanced CKD may preclude certain mechanical treatments for heart failure, such as ventricular assist devices.
How CHF Harms the Kidneys
When the heart weakens and struggles to circulate blood efficiently, the following complications commonly arise:
- Reduced oxygenated blood delivery to the kidneys — limits the kidneys’ ability to filter blood properly.
- Venous congestion — fluid accumulates in veins supplying the kidneys, disturbing filtration and pressure balance.
- Impaired renal haemodynamics and ischemic injury — caused by poor blood flow, which may further deteriorate kidney tissue over time.
This process leads to a vicious circle: worsening heart failure further damages the kidneys, and impaired kidneys amplify heart strain, accelerating disease progression.
How Kidney Disease Burdens the Heart
Chronic kidney disease poses unique risks to cardiac function:
- Waste product and toxin accumulation — unfiltered blood stresses the heart and other organs.
- Fluid overload — increases blood pressure and results in swelling, making the heart work harder.
- Chronic stimulation of hormonal systems — elevated renin-angiotensin-aldosterone and sympathetic nervous system activation further increase cardiac workload.
- Anaemia and uraemia — the heart receives less oxygen, and the toxic metabolic state worsens cardiac function.
The cumulative result is progressive cardiac remodeling, fibrosis, and dysfunction — all contributing to a heightened risk of heart failure as kidney disease advances.
Symptoms of Coexisting CHF and Kidney Disease
The classic features of both conditions may overlap or reinforce each other, with increasing severity in end-stage disease:
- Shortness of breath (especially with minimal exertion or lying flat)
- Fatigue and weakness
- Swelling (edema) of the ankles, feet, or sometimes the abdomen
- Decreased urination (as kidney function declines)
- Electrolyte imbalances (dangerous shifts in potassium, sodium, and others)
- Loss of appetite and unintentional weight loss
- Difficulty concentrating or mental confusion
Advanced disease can also result in worsening hypertension, rhythm disturbances, and life-threatening fluid overload. The appearance and severity of symptoms depend on how much each organ system is affected, the speed of disease progression, and individual patient factors.
Shared Risk Factors: What Drives the Overlap?
Several risk factors are common to both heart failure and kidney disease, and managing these risks is at the core of prevention and treatment approaches:
- High blood pressure (hypertension) — damages both the heart and kidney blood vessels, ranking as a primary risk for both diseases.
- Diabetes mellitus — causes blood vessel and organ damage, exacerbating heart and kidney complications.
- Atherosclerosis or coronary artery disease — arterial blockages affect blood flow to multiple organs.
- Obesity — increases the risk of both conditions and may worsen symptoms and disease progression.
- Older age — cumulative wear and tear on both organ systems increases likelihood of dual disease late in life.
- Family history of cardiac or renal disease
Diagnosing CHF and Kidney Disease: Key Tests and Early Detection
Early diagnosis and assessment are vital. Commonly used diagnostic strategies include:
- Blood tests — evaluate kidney function (creatinine, BUN), electrolytes, and markers of cardiac stress or damage.
- Urinalysis — checks for protein, signs of damage, or impaired filtration.
- Imaging studies — echocardiograms, CT, or MRI assess heart structure and efficiency.
- Electrocardiogram (EKG) — detects arrhythmias or changes typical of CHF.
- Blood pressure monitoring
Staging of both CHF and CKD is crucial to inform prognosis and treatment planning.
Treatment and Management Strategies
Therapeutic approaches focus on slowing progression, relieving symptoms, and preventing complications in both diseases.
Medications
- ACE inhibitors and angiotensin receptor blockers (ARBs) — support blood pressure control and protect heart and kidney function, but require close monitoring for adverse effects in advanced kidney disease.
- Diuretics — reduce fluid overload but can sometimes increase the risk of electrolyte disturbances in CKD.
- Beta-blockers — improve heart function and lower mortality in CHF.
- Statins — lower cholesterol, reducing cardiac and renal risk.
- Aldosterone antagonists — may offer benefit in CHF management; dosing must be adjusted for kidney impairment.
- Treatment of anaemia — using iron supplementation, erythropoiesis-stimulating agents, as both conditions commonly involve low red blood cell counts.
Lifestyle Adjustments
- Dietary management — reduce sodium and adjust protein intake as recommended.
- Fluid restriction — to prevent overload.
- Regular, moderate exercise — as tolerated.
- Managing underlying conditions — such as diabetes, hypertension, and cholesterol.
Invasive Treatments
- Mechanical heart pumps — sometimes required in advanced CHF, but may not be an option with severe kidney disease.
- Dialysis — for patients whose kidney function fails.
- Kidney transplantation — may be considered in select cases of end-stage kidney disease.
Care Coordination
- Multidisciplinary approach — involving cardiologists, nephrologists, primary care, and dietitians improves outcomes, manages complex drug regimens, and allows for ongoing adjustment to therapy.
- Patient education and engagement — understanding the conditions and actively managing symptoms are vital to maintaining quality of life.
Outlook for Patients
| Condition | Impact on Prognosis |
|---|---|
| Mild CHF / Early CKD | Often manageable with medications and lifestyle changes. Prognosis better with early intervention. |
| Advanced CHF / Advanced CKD | Significantly higher risk of complications, hospitalizations, and mortality. Requires complex management. |
| End-Stage Heart Failure / Kidney Failure | Often needs dialysis, advanced cardiac support, or transplantation. Symptom burden and risk of death increase sharply. |
While having both conditions worsens prognosis, aggressive management and early detection can slow disease progression and reduce hospitalizations. Renal function is a key predictor of both inpatient mortality and the likelihood of re-admission. Quality of life and long-term survival depend on the stage of disease, effectiveness and appropriateness of treatments, and successful management of shared risk factors.
Frequently Asked Questions (FAQs)
Q: Why do so many people develop both heart failure and kidney disease?
A: Both conditions share common risk factors, such as high blood pressure and diabetes, and cause damage to overlapping organ systems. Their physiological processes can lead each to trigger or worsen the other.
Q: What symptoms should I watch for if I have either CHF or kidney disease?
A: Seek medical attention if you notice worsening fatigue, shortness of breath (especially when resting or lying down), swelling in the legs or abdomen, decreased urine output, loss of appetite, or mental confusion.
Q: Can treating one condition help improve the other?
A: Yes, early and aggressive management of either heart failure or kidney disease can reduce the risk or severity of the other. Controlling blood pressure, managing diabetes, and treating anemia are especially important.
Q: What is the long-term outlook for patients with both CHF and CKD?
A: Outlook varies by the stage and severity of each condition. Early-stage disease may be stabilized for many years with proper management, while advanced disease requires more intensive therapies and may lead to increased risk of complications or death.
Q: Are there any treatments or medications that should be avoided?
A: Certain heart failure medications (such as ACE inhibitors or ARBs) may need dose adjustment or replacement in advanced CKD. Some drugs, like non-steroidal anti-inflammatory agents (NSAIDs), can worsen both conditions and should generally be avoided.
Key Takeaway
Congestive heart failure and chronic kidney disease form a vicious cycle where each condition can trigger or worsen the other. Early diagnosis, close monitoring, and comprehensive treatment strategies are crucial for optimizing quality of life and long-term survival. Working closely with a multidisciplinary healthcare team is essential for navigating the complexities of these overlapping chronic diseases.
References
- https://www.healthline.com/health/kidney-health/chf-and-kidney-failure
- https://revivalresearch.org/blogs/end-stage-congestive-heart-failure-and-kidney-failure/
- https://www.ecrjournal.com/articles/management-heart-failure-patients-chronic-kidney-disease?language_content_entity=en
- https://pubmed.ncbi.nlm.nih.gov/15202610/
- https://www.kidney.org/sites/default/files/Heart_Failure_and_CKD_2018.pdf
- https://snohomishkidney.com/wp-content/uploads/CKD-CHF-Patient-Education-PDF_Sno.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4465636/
- https://freseniusmedicalcare.com/en/media/insights/health-wellness/kidney-disease-heart-failure/
- https://www.cdc.gov/kidney-disease/risk-factors/link-between-diabetes-and-heart-disease.html
Read full bio of medha deb












