Cataract Surgery Complications: Risks, Recovery, and What to Expect
Understand common and rare complications, preventive care, and recovery tips after cataract surgery to safeguard your vision.
Cataract surgery is one of the most commonly performed and successful surgical procedures worldwide. While the vast majority of people experience improved vision and minimal issues following the operation, both common and rare complications can occur. Recognizing the signs of troubles early and understanding how to handle side effects are key to preserving vision and achieving the best outcome. This comprehensive guide covers all the possible complications, prevention tips, and recovery advice associated with cataract surgery.
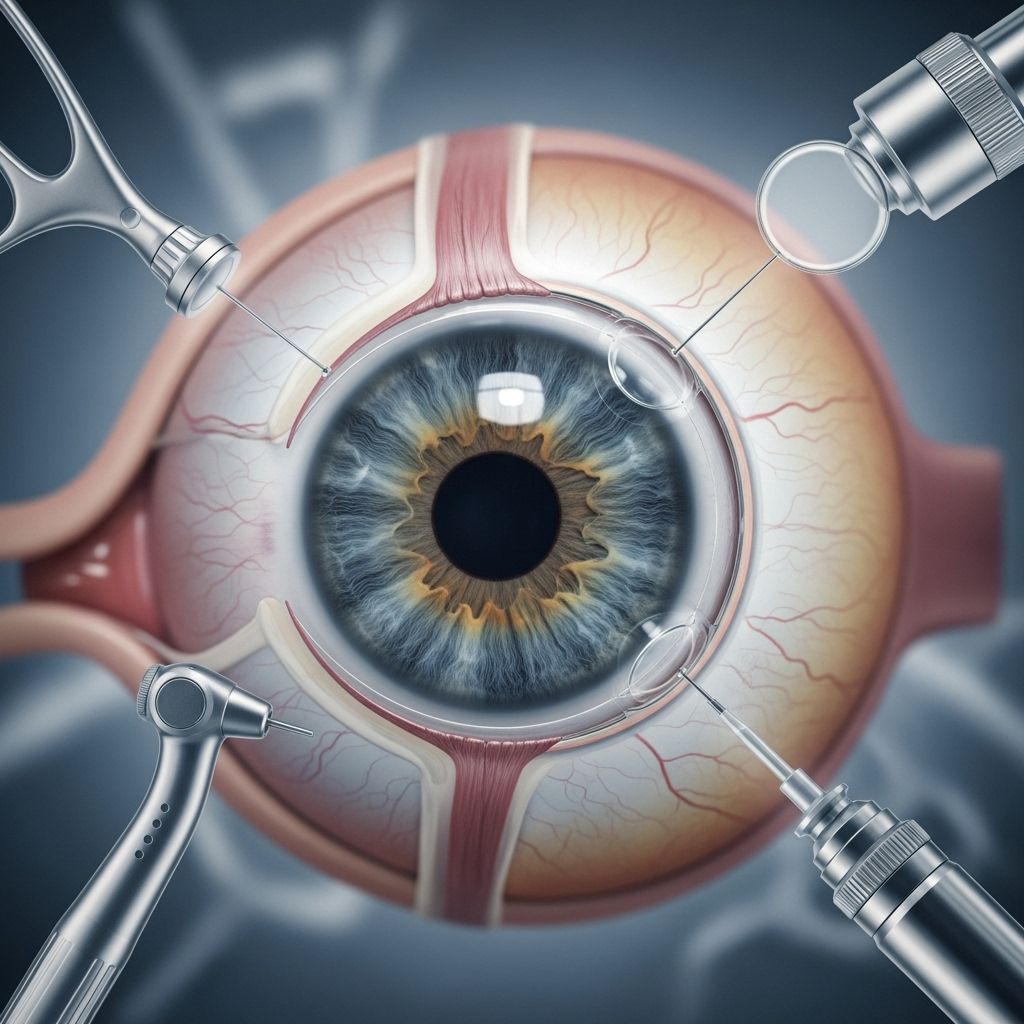
What Is Cataract Surgery?
Cataract surgery involves removing the eye’s cloudy natural lens and replacing it with a clear, artificial intraocular lens (IOL). The procedure is typically outpatient, meaning most patients return home the same day. Modern cataract surgery is highly effective in restoring vision; however, no surgery is entirely risk-free.
Common Complications After Cataract Surgery
Though the rate of serious complications is low, knowing what to expect allows for quicker response and a smoother recovery. Below are the most frequent issues encountered in the weeks or months after cataract removal:
- Posterior Capsular Opacification (PCO): Often called “secondary cataract,” PCO occurs when the back part of the lens capsule (left in place to hold the IOL) becomes cloudy. This affects approximately 14% to 60% of people post-surgery, sometimes developing weeks, months, or even years later. Symptoms include blurred or foggy vision. A straightforward outpatient procedure called YAG laser capsulotomy quickly restores vision in most cases.
- Cloudiness or Blurriness: Many patients report that their vision is blurry for a short period after surgery. This typically resolves within a few days to several weeks as the eye heals. Persistently cloudy vision can signal other underlying issues, such as PCO or corneal swelling.
- Floaters: Small specks or “cobwebs” called floaters may increase after surgery. While most are harmless, a sudden surge or presence of light flashes may indicate a retinal tear or detachment, which requires immediate medical attention.
- Dry Eyes: A gritty or dry sensation in the eyes is common and usually managed with lubricating eye drops. This symptom gradually fades as the eye recovers.
- Eye Pain or Discomfort: Mild irritation, a feeling of pressure, or minor aching can occur for a few days post-surgery. Persistent or severe pain is abnormal and should be evaluated for possible infection, inflammation, or elevated eye pressure.
- Double Vision: Temporary double vision sometimes occurs as the brain adapts to new visual input. This effect generally resolves within days as healing progresses.
Rare but Serious Complications
The following complications are much less common but can seriously threaten vision if not treated promptly:
- Endophthalmitis: This severe infection affects the fluids inside the eye. Symptoms include increasing pain, redness, swelling, and vision deterioration, and typically develop 3 to 7 days after surgery. Incidence is rare (estimated 0.05% to 0.30% of surgeries). Treatment with antibiotics and, in severe cases, surgery is required to save vision.
- Toxic Anterior Segment Syndrome (TASS): A very rare, non-infectious inflammatory reaction often linked to contaminated surgical equipment or medications. Symptoms are similar to endophthalmitis but appear within 12-48 hours. High-dose steroids are the main treatment, and rapid intervention is essential to reduce long-term vision loss.
- Retinal Detachment: Detachment of the retina occurs in roughly 0.4%–2% of cases, more likely in younger patients or those with other eye disorders. Warning signs include sudden onset of floaters, flashes of light, or a shadow/curtain over vision. This is an ophthalmic emergency, and prompt surgery is necessary to prevent permanent blindness.
- Cystoid Macular Edema (CME): Fluid accumulation in the central retina (macula) often results in blurry, distorted central vision. CME is the most common cause of vision decline after otherwise successful cataract surgery, happening in 1–2% of cases. It typically appears 4–8 weeks after the operation and usually responds well to anti-inflammatory eye drops or injections.
- Intraocular Lens (IOL) Dislocation: Although rare, the artificial lens may shift out of position, particularly in people with weak supporting structures or after trauma. Symptoms include sudden blurred or doubled vision. Surgery may be needed to reposition or replace the lens.
- Retained Lens Fragments: Tiny pieces of the original lens may remain after surgery, causing blurry vision, redness, tearing, or light sensitivity. If these fragments are bothersome, surgical removal may be necessary.
- Chronic Corneal Edema: Persistent swelling of the cornea, especially in people with pre-existing corneal endothelial problems (such as Fuchs’ dystrophy). Modern techniques have made this complication much less common (<0.1%).
- Capsular Contraction Syndrome: Extremely rare (0.004% incidence), occurs when the capsule that holds the IOL contracts and reduces the space for the lens. A minor surgical procedure is used to relieve the contraction.
Less Common Side Effects and Risks
- Light sensitivity
- Temporary redness and irritation
- Allergic reaction to anesthesia (very rare)
- Swelling of the eyelids or cornea
- Uncorrected refractive error—that is, needing glasses for best vision after healing
Complications Timeline: When Issues May Arise
| Complication | Typical Onset | Action Needed |
|---|---|---|
| Cloudiness/Blurred Vision | Days to weeks after surgery | Usually self-resolves, monitor. If persistent, evaluation advised. |
| Floaters | Immediately or weeks/months after | If new or increasing, have eyes examined promptly. |
| Endophthalmitis | 3–7 days post-surgery | Seek emergency treatment for pain, swelling, vision loss. |
| Posterior Capsular Opacification (PCO) | Weeks to years after | Laser capsulotomy performed as needed. |
| Cystoid Macular Edema | 2–8 weeks after surgery | Anti-inflammatory medications usually resolve symptoms. |
| Retinal Detachment | Anytime post-surgery | Urgent ophthalmologic intervention required. |
| Dry Eye, Light Sensitivity | First few weeks | Artificial tears, sunglasses, follow-up for persistence. |
Prevention and Risk Reduction After Cataract Surgery
While not all complications can be prevented, you can take several steps to lower your risk and promote optimal healing:
- Use prescribed eye drops as instructed (commonly steroid and antibiotic drops for ~4 weeks)
- Do not rub or press on your eye
- Wear sunglasses outdoors to reduce light sensitivity
- Protect the eye from dust, wind, and water (no swimming for 4–6 weeks)
- Practice good hand hygiene when touching near the eye
- Attend all scheduled follow-up appointments
How Are Complications Treated?
Treatment depends on the specific complication:
- Posterior capsular opacification is treated by a painless, out-patient YAG laser procedure that restores vision immediately.
- Infections are managed with antibiotic or antifungal medications delivered directly to the eye or, if severe, by surgery.
- Corneal swelling and macular edema usually respond to anti-inflammatory eye drops (sometimes combined with oral medications or injections).
- Detached retinas require urgent surgical intervention to reattach the retina and preserve vision.
- IOL dislocation may require repositioning or replacing the lens in a minor surgical procedure.
When to Seek Immediate Medical Attention
- Severe, worsening, or sudden-onset eye pain
- Sudden loss or significant reduction in vision
- Increasing redness and swelling
- Flashes of light or new/frequent floaters
- Dark curtain or shadow moving across your field of vision
If you experience any of these symptoms after cataract surgery, contact your ophthalmologist or go to the nearest emergency facility promptly. Rapid treatment is critical for saving sight in the event of a serious complication.
Long-Term Prognosis and Outlook
For most patients, cataract surgery is life-changing, restoring clarity and improving quality of life. More than 98% of people experience no serious, long-term problems. Even when complications do occur, the majority are manageable with timely medical intervention. Keeping up with routine eye care and reporting new symptoms quickly helps you retain the benefits of your cataract surgery for years to come.
Frequently Asked Questions (FAQs)
Is cataract surgery safe?
Yes. Cataract surgery is considered one of the safest and most effective surgeries in medicine. Most people regain clear vision within days, and complication rates are low. However, as with any surgery, risks remain and vigilance is important, especially in the first few weeks post-surgery.
Why is my vision still blurry after cataract surgery?
It’s normal for vision to be blurry for several days while the eye heals. Blurring that persists beyond a few weeks or worsens may be due to dry eye, swelling, or posterior capsular opacification. If blurriness lasts or worsens, see your surgeon promptly for evaluation.
What is posterior capsular opacification (PCO)?
PCO, also known as a “secondary cataract,” happens when cells cloud the lens capsule behind the implanted IOL. A painless, laser procedure restores vision quickly and permanently for most people.
Can complications develop years later?
Yes, some issues like PCO or retinal detachment can develop months to years after surgery. Any new vision problems—especially sudden ones—should be checked without delay.
How do I know if my discomfort or pain is normal?
Mild discomfort and dryness are expected in the first week or two. Severe pain, swelling, increasing redness, flashes, or new floaters are warning signs and should prompt immediate contact with your eye care provider.
Is there anything I can do to lower my risk of complications?
Follow your post-surgical instructions closely, use all prescribed medications, practice excellent eye hygiene, avoid swimming, and go to all follow-up appointments—even if you feel great.
Key Takeaways
- Cataract surgery is safe and highly successful, but all surgery carries some risks.
- Recognizing signs of complications and acting quickly help prevent long-term consequences.
- Protecting your eyes and following aftercare advice is essential for optimal recovery.
- Contact your eye surgeon with any concerns after your operation, no matter how minor they seem.
Protect your vision—know the risks, follow your aftercare plan, and enjoy the bright, clear world that modern cataract surgery can provide.
References
- https://www.nvisioncenters.com/cataract-surgery/complications/
- https://www.healthline.com/health/eye-health/cataract-surgery
- https://www.healthline.com/health/eye-health/cataract-surgery-complications
- https://precisionvisionlondon.com/the-truth-about-cataract-surgery/
- https://www.medicalnewstoday.com/articles/cataract-surgery-risks
- https://www.medicalnewstoday.com/articles/326346
- https://www.eyecliniclondon.com/blog/potential-cataract-surgery-complications/
- https://armadale-eye.com.au/can-you-have-cataract-surgery-twice/
- https://www.morningtoneye.com.au/food-not-to-eat-after-cataract-surgery/
- https://armadale-eye.com.au/traumatic-cataract/
Read full bio of medha deb












