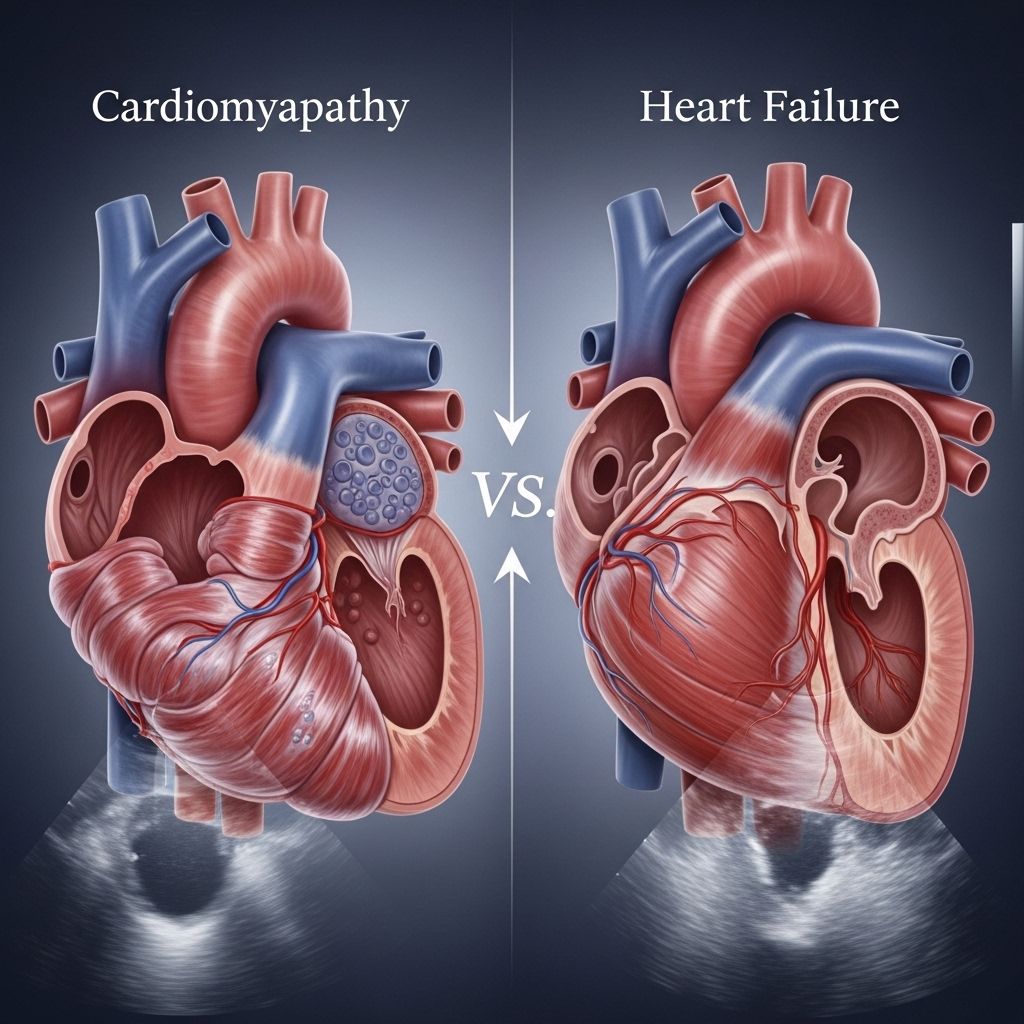
Cardiomyopathy vs. Heart Failure: Differences, Symptoms, and Treatment
Understand how cardiomyopathy and heart failure are connected, how they differ, and why early diagnosis matters for your heart health.
Cardiomyopathy vs. Heart Failure: A Comprehensive Overview
Both cardiomyopathy and heart failure are conditions that affect how well your heart pumps blood throughout your body. Although related, they have different causes, mechanisms, symptoms, and treatment approaches. Understanding their relationship and how they differ is essential for early intervention and effective management.
Understanding the Basics: Definitions and Key Differences
Cardiomyopathy is a general term that refers to diseases of the heart muscle. These diseases weaken, enlarge, or stiffen the heart muscle, making it difficult for the heart to pump blood efficiently.
Heart failure is a syndrome in which the heart can no longer pump blood effectively enough to meet the body’s requirements for oxygen and nutrients. Heart failure can result from various conditions, including cardiomyopathy, valve disease, high blood pressure, or other structural and rhythm problems.
- Cardiomyopathy: Disease affecting the heart muscle itself.
- Heart Failure: Condition where the heart’s pumping ability is insufficient for the body’s needs. It is often the final outcome of sustained heart muscle damage from various causes, including cardiomyopathy.
Cardiomyopathy as a Cause; Heart Failure as a Result
It’s important to remember that while cardiomyopathy can lead to heart failure, the two are not synonymous. Many people with cardiomyopathy do not immediately have heart failure, but over time, untreated cardiomyopathy may progress to it.
How the Heart Pumps: A Quick Refresher
The heart is a muscular organ with four chambers. Its primary role is to pump oxygenated blood to the body and return deoxygenated blood to the lungs for oxygenation. Heart muscle health and strength are essential for this task. When the muscle is weakened, thickened, or stiffened, its pumping ability is reduced, and symptoms of cardiovascular compromise develop.
Main Causes: Why Do These Conditions Develop?
| Cardiomyopathy | Heart Failure |
|---|---|
| Genetic mutations (often familial) | High blood pressure (hypertension) |
| Viral infections of heart muscle (myocarditis) | Valve disorders (e.g., aortic stenosis) |
| Alcohol abuse or toxins | Arrhythmias (abnormal heart rhythms) |
| Chronic high blood pressure | Coronary artery disease (blocked arteries) |
| Autoimmune conditions | Cardiomyopathy and other heart muscle diseases |
| Metabolic disorders (rare) | Congenital heart defects (present at birth) |
Types of Cardiomyopathy
- Dilated Cardiomyopathy (DCM): The heart muscle is stretched and thinned (dilated), which reduces pumping efficiency.
- Hypertrophic Cardiomyopathy (HCM): The heart muscle thickens abnormally, often due to genetic mutations. This can affect the flow of blood out of the heart.
- Restrictive Cardiomyopathy: The heart muscle becomes stiff, restricting filling with blood between beats.
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): Fatty or fibrous tissue replaces the muscle in the right ventricle, leading to arrhythmias.
Types of Heart Failure
- Heart Failure with Reduced Ejection Fraction (HFrEF): The heart muscle loses its strength to contract and pump blood.
- Heart Failure with Preserved Ejection Fraction (HFpEF): The heart muscle is stiff and cannot fill properly, but its pumping (ejection) strength may be normal.
- Right-Sided Heart Failure: Fluid backs up into the belly, legs, and feet (often due to lung issues).
- Left-Sided Heart Failure: Fluid may back up into the lungs, causing shortness of breath.
Symptoms: How Do Cardiomyopathy and Heart Failure Feel?
Symptoms can overlap, but their severity and presentation may provide clues. Many people with early or mild cardiomyopathy may not notice any symptoms until the disease advances. Heart failure generally produces noticeable symptoms sooner, especially with exertion or when more severe.
| Symptom | Cardiomyopathy | Heart Failure |
|---|---|---|
| Shortness of breath | Often after exercise | Worse when lying flat; can cause waking at night |
| Fatigue | Often after physical exertion | May present as muscle weakness |
| Irregular heartbeat (arrhythmia) | Common, can cause palpitations | May develop due to disease progression |
| Swelling in legs/ankles (edema) | Can indicate advanced disease or progress to heart failure | Common, sudden swelling can indicate rapid worsening |
| Chest pain | May occur after exertion or heavy meals | Usually during or after a heart attack |
| Dizziness or fainting (syncope) | Can occur at any time | Often due to heart failure medications or posture changes |
Diagnosis: How Are These Conditions Identified?
- Physical exam: Listening for abnormal heart sounds, check for edema, or jugular vein distention.
- Blood tests: Can help detect organ damage or infections.
- Electrocardiogram (ECG): Records abnormal rhythms or signs of a thickened heart muscle.
- Echocardiogram: Ultrasound imaging evaluates heart size, structure, and function.
- Stress tests: Measure the heart’s response to exertion.
- Cardiac MRI or CT: Gives detailed images of heart structures and function.
- Genetic testing: May be recommended if there is a family history, especially for cardiomyopathy.
Progression and Outlook: What Can You Expect?
Both cardiomyopathy and heart failure are typically progressive—without lifestyle changes and medical treatment, they tend to worsen over time. However, the outlook may be much improved with early diagnosis and appropriate management.
- Approximately 1 in 500 adults may have cardiomyopathy, but many go undiagnosed in early stages because symptoms are minimal.
- Heart failure is more common with age. About 2% of the U.S. adult population has heart failure, rising to 8.5% among adults aged 65–70.
It is possible to have cardiomyopathy without progressing to heart failure, especially with timely treatment. However, without management, the risk of developing heart failure increases considerably.
Treatment Options: Addressing Cardiomyopathy and Heart Failure
Treatment aims to slow progression, improve symptoms, and prevent serious complications like sudden cardiac death or advanced heart failure. Management is usually multimodal and tailored to the underlying cause and severity.
Lifestyle Changes
- Limit salt intake to reduce fluid retention.
- Eat a heart-healthy diet (rich in fruits, vegetables, whole grains).
- Avoid excessive alcohol and tobacco use.
- Exercise regularly—as directed by a healthcare provider.
- Manage underlying conditions like diabetes or high blood pressure.
Medications
- ACE inhibitors and ARBs: Lower blood pressure and reduce heart strain.
- Beta-blockers: Slow the heart and reduce workload.
- Diuretics: Alleviate fluid buildup.
- Antiarrhythmics: Control abnormal rhythms.
- Aldosterone antagonists: Reduce sodium retention and strain.
Devices and Surgery
- Implantable cardioverter-defibrillators (ICDs): Prevent sudden cardiac death from serious arrhythmias.
- Pacemakers: Help regulate heart rhythm.
- Left ventricular assist devices (LVADs): Support heart function in advanced cases.
- Heart transplant: In cases of end-stage heart failure where other treatments are not effective.
Special Considerations for Children
In children and younger people, cardiomyopathy is often genetic, while heart failure is more likely due to a congenital heart defect present from birth. Early detection and genetic counseling can guide family planning and intervention.
Prevention: Steps to Protect Your Heart
- Maintain normal blood pressure and cholesterol.
- Exercise most days of the week.
- Avoid substance abuse, including alcohol and recreational drugs.
- Control diabetes and treat infections promptly.
- Know your family history and get regular check-ups if you’re at higher risk.
When to See a Doctor: Warning Signs
- Shortness of breath that is new, worsening, or occurs at rest
- Chest pain—especially if associated with exertion or eating
- Dizziness, fainting, or near-fainting spells
- Leg swelling unresponsive to rest and elevation
- Irregular heart rhythm (palpitations)
Seek emergency attention for severe shortness of breath, sudden chest pain, or fainting.
Frequently Asked Questions (FAQs)
Is cardiomyopathy the same as heart failure?
No, cardiomyopathy refers specifically to diseases of the heart muscle, while heart failure is a general condition describing the inability of the heart to pump blood effectively. While cardiomyopathy often leads to heart failure, they are not identical.
Can you have cardiomyopathy without heart failure?
Yes, you can have cardiomyopathy without symptoms of heart failure, especially in early or mild forms. However, there is an increased risk of progressing to heart failure over time if not managed appropriately.
What symptoms should prompt medical evaluation for these conditions?
Symptoms such as shortness of breath, persistent fatigue, swelling in the legs or ankles, palpitations, chest pain, or dizziness should prompt timely consultation with a healthcare provider, especially if there is a family history of heart complication.
How are these conditions treated?
Treatment focuses on addressing underlying causes, symptom relief, and preventing progression. This often involves lifestyle modifications, medications, and, for advanced cases, devices or surgical options. Early intervention significantly improves outcomes.
Can people with cardiomyopathy or heart failure live a long life?
Many people, especially those who are diagnosed early and follow their treatment plans, can live well for years with either condition. Survival and quality of life have improved considerably thanks to advances in care.
Takeaway
Understanding the differences between cardiomyopathy and heart failure helps guide the right treatment, improves quality of life, and may prevent serious complications. If you have family members with heart disease or are experiencing persistent symptoms, proactive management is crucial. Always consult your healthcare provider for a tailored approach and regular monitoring of your heart health.
References
- https://now.optum.com/article/health/heart/cardiomyopathy-vs-heart-failure
- https://www.medicalnewstoday.com/articles/cardiomyopathy-vs-heart-failure
- https://resources.healthgrades.com/right-care/heart-failure/cardiomyopathy-vs-heart-failure
- https://www.nyp.org/heart/cardiomyopathy
- https://www.ncbi.nlm.nih.gov/books/NBK209980/
- https://nyulangone.org/conditions/cardiomyopathy-heart-failure/types
- https://www.mayoclinic.org/diseases-conditions/cardiomyopathy/symptoms-causes/syc-20370709
- https://www.cardiomyopathy.org/about-cardiomyopathy/heart-failure
- https://my.clevelandclinic.org/health/diseases/16841-cardiomyopathy
Read full bio of Sneha Tete












