Cardiomyopathy: Types, Symptoms, Causes, Diagnosis, and Treatment
Explore the progressive heart muscle disease, its types, symptoms, causes, risk factors, and treatments.
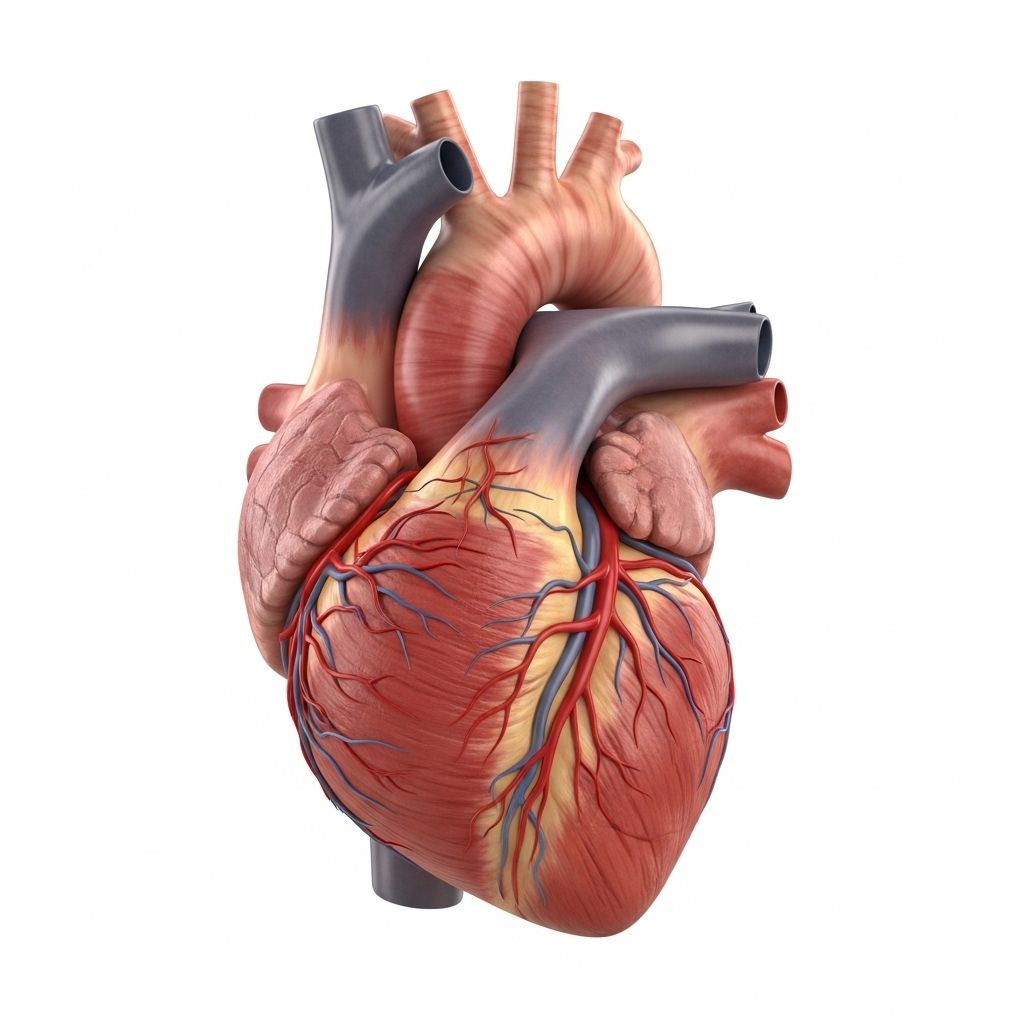
Cardiomyopathy Overview
Cardiomyopathy is a progressive disease of the heart muscle, where the muscle becomes weakened, enlarged, thickened, or stiffened. This affects the heart’s ability to pump blood effectively throughout the body, leading to a range of health complications and, in severe cases, heart failure. Cardiomyopathy can be inherited or develop due to other conditions, such as coronary artery disease, thyroid disorders, or chronic alcohol use.
While some forms of cardiomyopathy are rare, they are serious and require ongoing medical attention. Early detection and proper management may help prevent complications and improve quality of life.
Types of Cardiomyopathy
The term ‘cardiomyopathy’ encompasses several distinct types based on their structural, functional, and clinical features. The main types include:
- Dilated Cardiomyopathy (DCM)
Known as enlarged heart, DCM occurs when the heart chambers, especially the left ventricle, stretch and thin, becoming unable to pump blood efficiently. It’s the most common form and can be inherited or result from coronary artery disease, heart attacks, infections, or exposure to toxins (including alcohol and certain drugs). - Hypertrophic Cardiomyopathy (HCM)
This type leads to thickened heart walls, most often affecting the left ventricle. The thickening makes it harder for the heart to pump blood and increases the risk of electrical disturbances. It is commonly associated with genetic mutations but can also be acquired due to persistent hypertension, aging, diabetes, or thyroid disease. - Arrhythmogenic Right Ventricular Dysplasia (ARVD or ARVC)
A rare, genetic form predominantly affecting young athletes. Here, muscle cells in the right ventricle are replaced by fat and fibrous tissue, leading to abnormal rhythms and increasing the risk of sudden cardiac death. - Restrictive Cardiomyopathy (RCM)
RCM features stiff and inelastic heart muscle, hindering the ventricles from properly filling with blood. This type is uncommon and often secondary to systemic diseases (such as amyloidosis) or scarring of the heart muscle, which may occur after heart transplants. - Unclassified Cardiomyopathies
Some patients may have forms not fitting the above categories, which are termed unclassified cardiomyopathies.
Symptoms of Cardiomyopathy
Symptoms vary depending on the type and severity of cardiomyopathy. Some people may remain asymptomatic for years, while others develop signs as the condition progresses. Common symptoms include:
- Shortness of breath (especially with activity or when lying down)
- Fatigue and general weakness
- Swelling (edema) of the legs, ankles, feet, abdomen, or neck veins
- Palpitations (rapid, pounding, or fluttering heartbeats)
- Chest pain (often after exertion or heavy meals)
- Dizziness or fainting (syncope)
- Difficulty lying flat (orthopnea) due to breathing issues
- Cough (especially when lying down)
- Bloating in the stomach area due to fluid retention
Symptoms typically worsen without treatment. Sudden worsening or severe symptoms (chest pain, fainting, severe shortness of breath) should prompt immediate medical attention.
Causes of Cardiomyopathy
Cardiomyopathy can arise from genetic or acquired causes:
- Genetic mutations (inherited through families)
- Coronary artery disease or prior heart attacks
- Persistent high blood pressure (hypertension)
- Chronic alcohol or illicit drug use
- Thyroid or metabolic disorders
- Diabetes
- Severe electrolyte imbalances
- Infections affecting the heart (such as viral myocarditis)
- Exposure to toxins or certain chemotherapy agents
- Autoimmune diseases (e.g., sarcoidosis, amyloidosis)
- Unknown (idiopathic) factors
Some forms, such as hypertrophic and arrhythmogenic cardiomyopathy, are largely genetic. Others, like dilated cardiomyopathy, may be triggered by external factors or remain idiopathic despite rigorous investigation.
Risk Factors
Certain traits and exposures can increase the risk of developing cardiomyopathy:
- Family history of heart disease or cardiomyopathy
- Age (some types are more common in young or older adults)
- History of heart conditions (e.g., previous heart attacks)
- Chronic hypertension
- Diabetes
- Obesity
- Alcohol or drug abuse
- Infection or inflammation affecting the heart
- Autoimmune disorders
Not everyone with these risk factors will develop cardiomyopathy, but recognizing them may encourage early screening and preventive measures.
When to Seek Medical Care
Immediate evaluation by a healthcare professional is recommended if you experience:
- New, intense, or persistent chest pain
- Fainting (especially with exertion)
- Sudden shortness of breath or difficulty breathing
- Rapid, irregular heartbeat or palpitations
- Severe swelling in the legs or abdomen
If diagnosed, family members of those with genetic forms of cardiomyopathy should also be screened, as early detection can be lifesaving.
Diagnosis
Diagnosis of cardiomyopathy involves a thorough medical history, physical exam, and diagnostic tests:
- Electrocardiogram (ECG/EKG): Measures the electrical activity and rhythm of the heart.
- Echocardiogram: Uses ultrasound to visualize heart structure, movement, and measure wall thickness or chamber size.
- Chest X-ray: Reveals heart shape and evidence of enlarged chambers or fluid in the lungs.
- Cardiac MRI or CT scan: Provides detailed images of heart anatomy and detects scarring or fat replacement.
- Blood tests: Identify underlying causes, inflammation, or organ involvement.
- Exercise Stress Test: Assesses heart function under exertion.
- Cardiac catheterization: Evaluates pressures and detects blocked arteries.
- Genetic testing: Useful for inherited forms and family member screening.
Physicians may also review family history and inquire about specific symptoms to classify the type and severity of cardiomyopathy.
Treatment Options for Cardiomyopathy
While not all forms of cardiomyopathy can be cured, treatment aims to manage symptoms, prevent complications, and improve heart function. Common approaches include:
- Lifestyle changes
– Maintaining a healthy weight
– Regular physical activity (as guided by your doctor)
– Low-sodium, heart-healthy diet
– Limiting alcohol consumption
– Avoiding recreational drugs - Medications
– ACE inhibitors, beta-blockers, and angiotensin receptor blockers (lower blood pressure, reduce heart strain)
– Diuretics (control fluid buildup)
– Anti-arrhythmic drugs (stabilize heart rhythm)
– Blood thinners (reduce clot risk in certain patients) - Surgical Procedures & Devices
– Implantable cardioverter-defibrillators (ICDs) or pacemakers (manage arrhythmias)
– Left ventricular assist devices (LVADs) for severe heart failure
– Heart transplantation (reserved for treatment-resistant, advanced cases) - Disease-specific therapies
– Genetic counseling and targeted treatments for inherited forms
– Novel agents for amyloidosis or sarcoidosis-associated restrictive cardiomyopathy
Treatment is highly personalized and may change over time depending on symptoms, the underlying cause, and the patient’s response to therapy. Regular follow-up is crucial for monitoring disease progression and adjusting treatment.
Prevention
While not all forms of cardiomyopathy can be prevented, some strategies may reduce your risk or slow progression:
- Control high blood pressure, diabetes, and cholesterol
- Limit alcohol intake and avoid drugs
- Maintain a healthy weight and exercise regularly
- Seek early evaluation for symptoms or family history
- Follow heart-healthy diet recommendations
Early intervention and management of risk factors can help prevent heart damage and complications related to cardiomyopathy.
Prognosis and Outlook
The outlook for individuals with cardiomyopathy depends on their type, severity, and how well the condition responds to treatment. With proper management:
- Some patients maintain good function and quality of life for many years.
- Others may experience progressive heart failure or life-threatening arrhythmias requiring advanced therapies.
- Early diagnosis and personalized treatment are critical for improving outcomes.
Regular checkups, medication adherence, and lifestyle modifications are essential for managing the disease and avoiding complications.
Complications
If left untreated, cardiomyopathy can lead to serious complications:
- Heart failure
- Arrhythmias (abnormal heart rhythms)
- Sudden cardiac death (particularly in ARVD/ARVC)
- Blood clots and stroke
- Valve dysfunction
Timely management is crucial for reducing the risk of such complications.
Frequently Asked Questions (FAQs)
Q: Is cardiomyopathy hereditary?
A: Several types, especially hypertrophic and arrhythmogenic cardiomyopathies, have a strong genetic component. Family members should consider screening if a relative is diagnosed.
Q: Can cardiomyopathy be cured?
A: Most types can be managed but not cured. Early treatment and lifestyle changes can improve outcomes and quality of life.
Q: What lifestyle changes help cardiomyopathy?
A: Avoiding alcohol and recreational drugs, maintaining a heart-healthy diet, regular exercise (under medical supervision), controlling blood pressure and diabetes, and adhering to prescribed medications.
Q: How does cardiomyopathy cause heart failure?
A: The weakened or stiffened heart muscle can’t pump enough blood, leading to fluid buildup, fatigue, and other symptoms of heart failure.
Q: When should I see a doctor for symptoms?
A: Seek immediate care for new or severe chest pain, fainting, sudden palpitations, or difficulty breathing. Routine evaluation is warranted for persistent symptoms.
Summary Table: Types of Cardiomyopathy
| Type | Main Feature | Common Causes | Key Risks |
|---|---|---|---|
| Dilated | Enlarged, weakened chambers | Genetic, CAD, toxins, infection | Heart failure, arrhythmias |
| Hypertrophic | Thickened ventricles | Genetic, hypertension | Sudden death, rhythm disturbances |
| Restrictive | Stiff, inflexible muscle | Amyloidosis, scarring | Heart failure |
| Arrhythmogenic (ARVD/ARVC) | Fat/fibrous replacement of muscle | Genetic | Arrhythmias, sudden death |
Conclusion
Cardiomyopathy is a complex, progressive heart muscle disease impacting people of all ages. Understanding its types, symptoms, causes, and treatment options is critical for prompt diagnosis and effective management. If you or your family members have risk factors or symptoms, seek medical advice and consider regular evaluations to safeguard heart health.
References
- https://www.healthline.com/health/heart-disease/cardiomyopathy
- https://www.mayoclinic.org/diseases-conditions/cardiomyopathy/symptoms-causes/syc-20370709
- https://my.clevelandclinic.org/health/diseases/16841-cardiomyopathy
- https://www.healthline.com/health/hypertrophic-cardiomyopathy
- https://www.medicalnewstoday.com/articles/327456
- https://www.cedars-sinai.org/newsroom/healthline-therapy-vs-antidepressants–which-is-best-for-people-with-heart-disease/
- https://www.medicalnewstoday.com/articles/237191
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8445013/
- https://www.healthline.com/health/video/how-to-prevent-heart-disease-according-to-a-cardiologist
- https://www.ahajournals.org/doi/10.1161/strokeaha.107.487710
Read full bio of medha deb












