Cardiac Stents: Procedure, Benefits, Risks, and Lifelong Care
Understand how cardiac stents restore heart health, what to expect from the procedure, and how to maintain heart wellness after stent placement.
Cardiac Stents: Transforming Heart Health
A cardiac stent is a medical device that has revolutionized the management of coronary artery disease (CAD) and heart attacks. Used to open blocked or narrowed arteries, stents help restore blood flow to the heart, reducing symptoms and improving quality of life.
What is a Cardiac Stent?
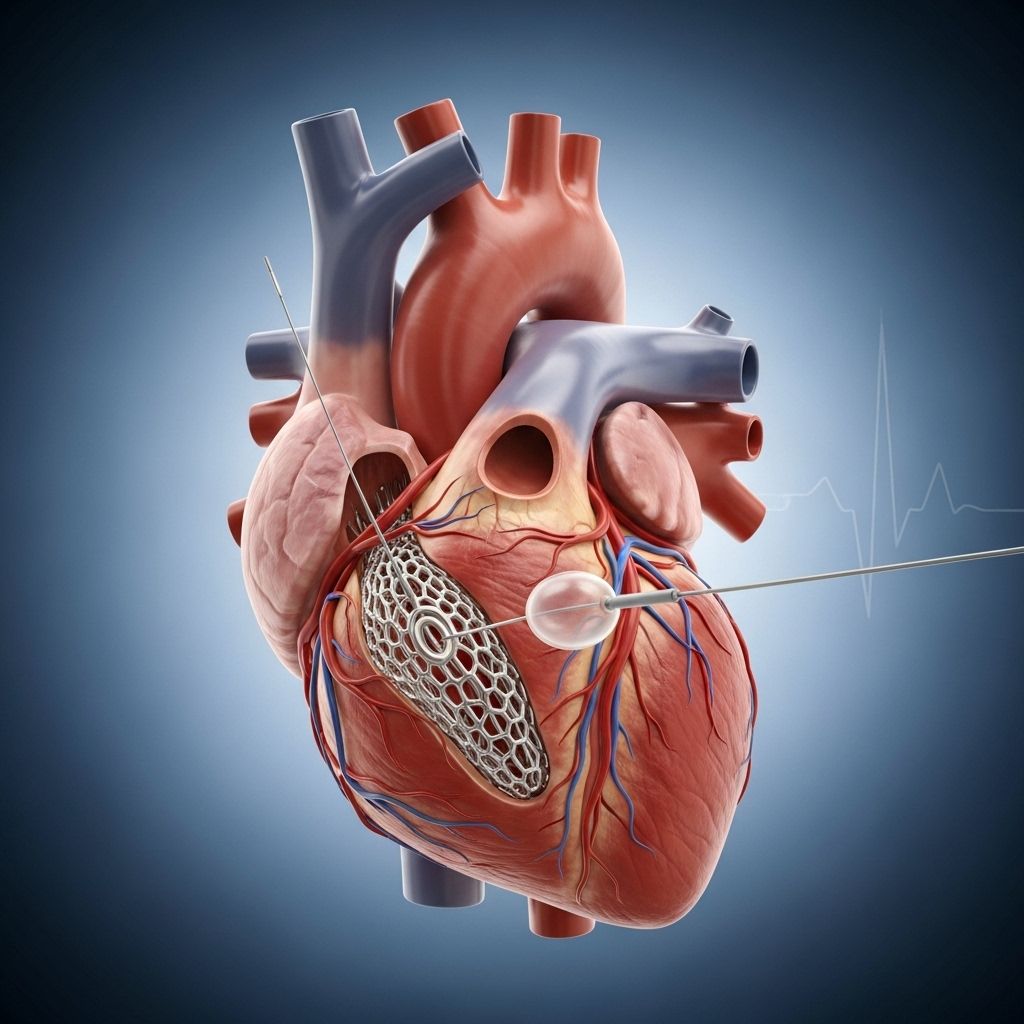
Cardiac stents are tiny, expandable coils constructed from metal mesh. They are designed to reinforce artery walls and keep them open, especially in areas affected by the build-up of fatty plaque—a hallmark of coronary heart disease.
- Stents support artery walls and keep blood moving freely.
- Typical use: treat narrowed or blocked coronary arteries.
- Also used after heart attacks to prevent further damage.
- Usually inserted via a minimally invasive procedure known as coronary angioplasty.
In some cases, particularly when more than two arteries are blocked, coronary bypass surgery may be recommended instead of stenting.
How is a Cardiac Stent Inserted?
Insertion of cardiac stents is a precise, minimally invasive process requiring skillful use of modern surgical technology.
- Preparation: Local anesthesia is administered to numb a small area—usually the groin, arm, or neck—where the procedure begins.
- Catheter Insertion: A thin, flexible tube (catheter) equipped with a balloon and stent is threaded through a blood vessel toward the heart.
- Imaging Guidance: Special dyes and real-time monitors help the physician guide the catheter to the exact site of blockage.
- Stent Deployment: When the catheter reaches the narrowed segment, the balloon inflates, expanding the stent and compressing plaque against the artery wall. This opens the vessel and restores blood flow.
- Finishing: The balloon is then deflated and removed, leaving behind the expanded stent. A filter may be used during the procedure to capture loose fragments of plaque or clots.
After the procedure, patients are typically prescribed medications that help prevent blood clots from forming within the stent. As the artery heals, the tissue grows into the stent mesh, strengthening the vessel.
Types of Cardiac Stents
- Bare Metal Stents (BMS): Simple metal mesh stents that physically open the artery but have a higher risk of restenosis (re-narrowing).
- Drug-Eluting Stents (DES): Coated with medication to reduce the chance of restenosis by preventing excessive tissue growth within the stent.
Drug-eluting stents are commonly used today and are preferred for their lower rates of re-narrowing.
Benefits of Cardiac Stenting
For many individuals with blocked arteries, cardiac stenting offers substantial, often immediate, improvement in heart health.
- Restored blood flow: Stents open blocked arteries, quickly improving circulation.
- Damage prevention: Early stenting after a heart attack can minimize lasting damage to the heart muscle.
- Reduced symptoms: Relief from chest pain (angina) and shortness of breath.
- Fast recovery: Most people recover within days, much quicker than after coronary bypass surgery, which may require six weeks or longer.
- Avoidance of major surgery: Minimally invasive nature reduces risks and discomfort compared to open-heart procedures.
Stenting may eliminate the need for bypass surgery in some cases, but suitability depends on the number of blocked arteries and individual health status.
Risks and Complications of Cardiac Stenting
Like all medical interventions, cardiac stenting carries potential risks. Understanding these helps patients and caregivers be vigilant.
- Allergic reactions: Some may react to the materials or medications used during angioplasty and stenting.
- Procedural risks: Bleeding, damage to vessels or heart tissue, and irregular heartbeat can occur.
- Serious complications (rare): Heart attack, kidney failure, and stroke are rare but possible.
- Restenosis: Scar tissue may form inside the stent, narrowing the artery again and potentially requiring repeat intervention.
- Blood clots: Formation of clots within stents can lead to heart attacks. Lifelong medication is usually prescribed to mitigate this risk.
It’s crucial to report any symptoms like chest pain to your doctor immediately after stenting.
How Long Do Cardiac Stents Last?
Cardiac stents are engineered to be durable and often remain effective for many years. However, their longevity depends on several factors:
| Factor | Impact on Stent Lifespan |
|---|---|
| Type of stent | Drug-eluting stents tend to last longer due to their medication coating. |
| Patient health conditions | Diabetes, hypertension, and high cholesterol can shorten lifespan; well-managed conditions extend it. |
| Lifestyle choices | Healthy diet, exercise, smoking cessation prolong stent effectiveness. |
| Medication adherence | Taking prescribed antiplatelet drugs prevents clots and keeps stents working. |
Restenosis is most likely in the first six months after stenting, but drug-eluting stents minimize this risk. Routine follow-up care ensures lifelong stent patency.
Post-Operative Care and Recovery
The success of cardiac stenting is not just in the operating room, but in meticulous long-term care.
- Activity: Avoid strenuous activity (especially heavy lifting) for several weeks after stenting.
- Diet: Adhere to a heart-healthy diet, such as the Mediterranean diet, focused on fruits, vegetables, lean meats, whole grains, and healthy fats.
- Medications: Antiplatelet therapy is essential to prevent clot formation. Always take medications as prescribed.
- Follow-up appointments: Regular checkups monitor the stent and overall heart health. These may include angiography or non-invasive scans.
- Lifestyle modifications: Smoking cessation, exercise, and weight management are crucial.
Attending all follow-ups and reporting any new symptoms facilitates timely intervention if complications arise.
Medical Guidelines for Coronary Stent Monitoring
- American College of Cardiology (ACC) & American Heart Association (AHA): Recommend regular monitoring, non-invasive imaging, proactive management, and timely intervention to prevent complications.
- European Society of Cardiology (ESC): Advocate for routine visits and advanced diagnostic tools; emphasize personalized care based on patient needs and stent status.
- Society for Cardiovascular Angiography and Interventions (SCAI): Encourage ongoing surveillance, integration of non-invasive monitoring, and clinician training in new techniques.
Careful adherence to these guidelines helps maintain heart wellness and prevents adverse complications following stenting.
Living with a Cardiac Stent
A cardiac stent may require certain adjustments in your daily routine, but thousands thrive after stent placement.
- Adopt lifelong heart-healthy habits.
- Take all prescribed medications as directed; never skip dosages.
- Report unusual symptoms, such as chest pain or shortness of breath, as soon as possible.
- Stay engaged with cardiac rehabilitation programs when recommended.
- Work closely with your healthcare team for optimal long-term outcomes.
Frequently Asked Questions (FAQs)
Q: How do I know if I need a cardiac stent?
A cardiac stent may be recommended if you have narrowing or blockage of a coronary artery, especially if you experience chest pain, shortness of breath, or have a heart attack. Your cardiologist will determine suitability based on your arteries and health.
Q: What can I expect during recovery?
Most patients recover from stenting within a few days. Expect mild discomfort at the incision site and gradual improvement in symptoms. Heavy lifting and intense activity should be avoided initially.
Q: Are lifestyle changes necessary after stent placement?
Absolutely. Heart-healthy lifestyle changes, including diet, exercise, and smoking cessation, are essential to ensure your stent lasts and your heart stays healthy.
Q: Is there any risk of my artery becoming blocked again after stenting?
Restenosis (re-narrowing) is a risk, especially with bare metal stents, but drug-eluting stents substantially reduce this risk. Routine follow-ups help detect and address any issues early.
Q: Will I need to take medication for the rest of my life?
Most patients need lifelong antiplatelet medications to prevent clot formation within the stent. Always consult your doctor before stopping any prescribed drug.
Q: Can I travel or exercise with a stent?
Yes—with your doctor’s approval, most activities are possible after recovery. Consistent exercise is encouraged for heart health; traveling after recovery is generally safe.
Cardiac Stent Care: Dos and Don’ts Table
| Do | Don’t |
|---|---|
| Follow medication and diet recommendations strictly | Ignore symptoms like chest pain or shortness of breath |
| Attend all regular checkups and monitoring appointments | Resume strenuous activity too soon after the procedure |
| Maintain open communication with your healthcare team | Stop medication without doctor approval |
| Adopt heart-healthy habits for life | Neglect recommended lifestyle changes |
Summary
Cardiac stents provide a life-saving solution for those with blocked coronary arteries. When coupled with proper post-procedure care and lifestyle changes, stents can dramatically improve heart health and quality of life. Always follow medical advice closely and prioritize your heart wellness for the best long-term results.
References
- https://www.healthline.com/health/heart-disease/stent
- https://www.dxnimble.com/post-coronary-stent-care-understanding-the-dos-and-donts/
- https://www.dxnimble.com/how-long-do-coronary-stents-last-and-factors-that-influence-their-lifespan/
- https://www.healthline.com/health/stent
- https://www.medicalnewstoday.com/articles/237191
- https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-disease-prevention/art-20046502
- https://www.britannica.com/science/coronary-heart-disease
- https://www.ebsco.com/research-starters/complementary-and-alternative-medicine/natural-treatments-heart-attacks
- https://www.heartandstroke.ca/articles/exercising-when-you-have-heart-disease
- https://www.nhlbi.nih.gov/health/coronary-heart-disease/treatment
Read full bio of medha deb












