Cardiac Cirrhosis: Understanding Causes, Symptoms, Diagnosis, and Treatment
A comprehensive guide to cardiac cirrhosis: exploring its connection to heart health, risks, diagnosis, symptoms, management, and long-term outlook.
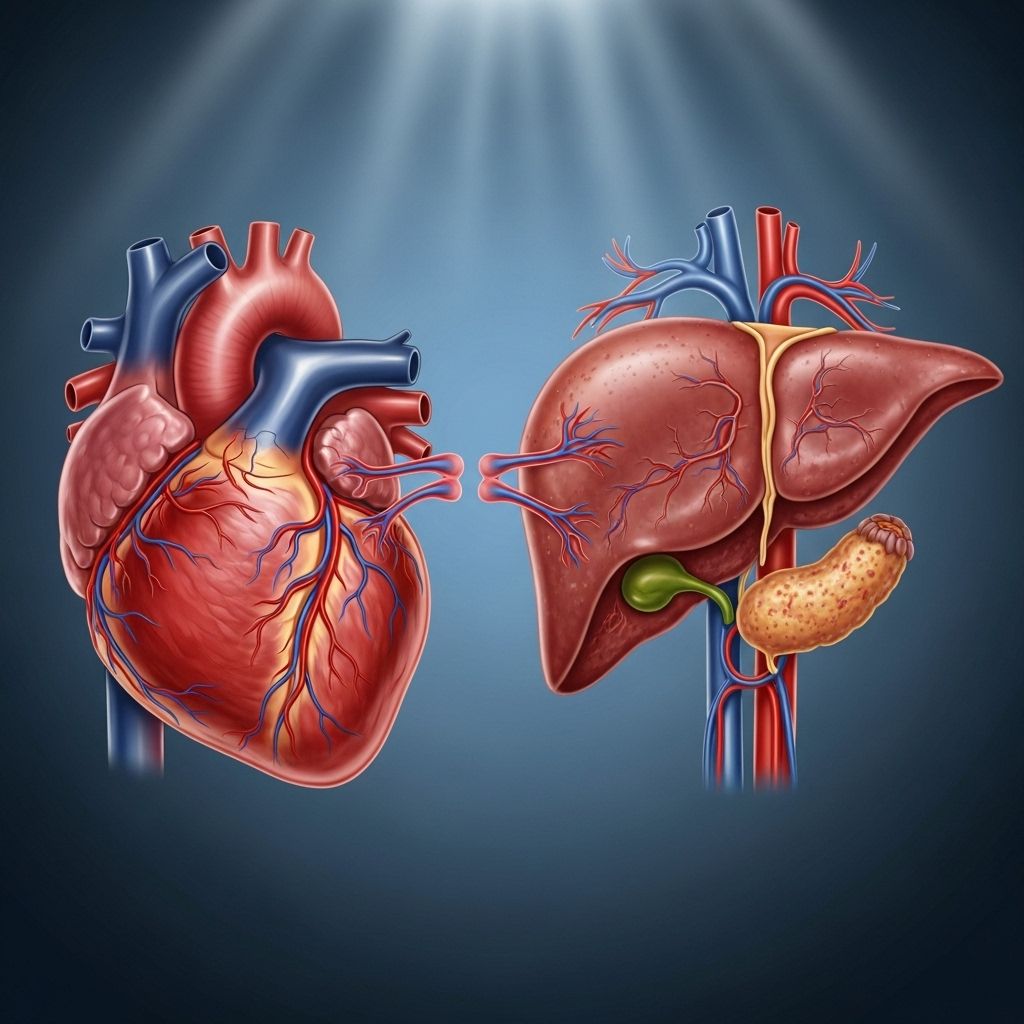
Cardiac Cirrhosis: At the Crossroads of Heart and Liver Health
Cardiac cirrhosis, also known as congestive hepatopathy, is a unique form of liver disease directly linked to chronic heart dysfunction. When the heart fails to pump blood efficiently, especially on the right side, this can lead to increased pressure within the veins surrounding the liver, causing congestion, scarring, and ultimately damage to vital liver tissue. Cardiac cirrhosis exemplifies how the body’s major organs are interconnected, with poor heart health precipitating problems that extend far beyond the cardiovascular system.
What Is Cardiac Cirrhosis?
Cardiac cirrhosis refers to liver damage caused by longstanding heart failure and impaired circulation. If the heart is unable to pump enough oxygenated, nutrient-rich blood to the liver, toxins are less efficiently filtered from the body, and pressure builds within the veins serving the liver. Over time, this pressure leads to fluid buildup and injury to hepatocytes, the specialized cells making up liver tissue. Scarring accumulates, impairing the liver’s ability to perform its many metabolic, detoxification, and synthetic functions.
Cardiac cirrhosis primarily develops as a result of nasal congestion in the liver veins (congestive hepatopathy), secondary to right-sided heart failure. This process also causes chronic passive congestion, inflammation, and fibrosis of the liver.
- Alternate Name: Congestive hepatopathy
- Main Mechanism: Increased venous pressure and blood congestion in the liver due to heart dysfunction
- Primary Outcome: Progressive scarring and impairment of liver function
Why Are Heart and Liver Health Linked?
The liver depends on steady blood flow from the heart to sustain normal oxygenation and pressure. When the heart struggles, especially the right atrium, blood returning from the body pools in veins—including those supplying the liver. This chronic congestion increases resistance, disrupts normal liver architecture, and injures cells. Over time, repetitive injury leads to fibrosis (scarring) and ultimately cirrhosis.
Causes and Risk Factors for Cardiac Cirrhosis
Right-sided heart failure is the central risk factor for cardiac cirrhosis. When the right atrium cannot keep up with blood return, pressure backs up into the veins draining the liver and the vena cava, leading to hepatic congestion and damage. However, multiple cardiovascular and pulmonary diseases can contribute to right-sided heart failure and thus cardiac cirrhosis.
- Chronic lung disease (cor pulmonale): Lung disorders that strain the right side of the heart
- Pulmonary hypertension: High blood pressure in the lungs, increasing resistance to right heart output
- Pulmonary embolism: Clots blocking blood flow to the lungs, pressurizing the right heart
- Valvular heart disease: Especially mitral valve stenosis and tricuspid valve regurgitation
- Constriction due to pericarditis: The pericardium becomes stiff and restricts heart motion
- High systemic blood pressure: Makes it harder for the heart to move blood forward
- Certain congenital heart diseases: Born structural defects may predispose to cardiac cirrhosis later
Many conditions, such as left-sided heart failure, can also eventually lead to right-sided heart failure, increasing the risk of developing cardiac cirrhosis.
Symptoms of Cardiac Cirrhosis
The clinical signs of cardiac cirrhosis can be subtle, especially in the early stages. Frequently, symptoms may overlap with other liver diseases or may be masked by the underlying heart condition. Some individuals may have no symptoms until substantial liver damage occurs.
- Abdominal discomfort or fullness due to liver enlargement and fluid buildup
- Swelling (edema) in the legs, ankles, or abdomen (ascites)
- Fatigue due to poor circulation and impaired liver function
- Jaundice: Yellowing of the skin and eyes
- Enlarged or tender liver: May be felt on physical exam
- Dark urine and pale stools: Indicating altered bile metabolism
- Easy bleeding or bruising: Due to decreased clotting factors from liver dysfunction
- Confusion or altered mental status: A result of toxins affecting the brain (hepatic encephalopathy)
Symptoms can be variable, and sometimes cardiac cirrhosis is only discovered incidentally during workup for abnormal liver enzyme results or imaging findings.
Diagnosis of Cardiac Cirrhosis
Diagnosing cardiac cirrhosis involves careful evaluation of both liver and heart function by your healthcare team. Because the condition can mimic or be masked by other liver or heart disorders, a combination of tests is typically required.
- Physical examination: Looking for telltale signs such as jaundice, edema, liver enlargement, or tenderness
- Blood tests: Checking for elevated liver enzymes, abnormal clotting times, or reduced albumin
- Imaging studies: Abdominal ultrasound is often used initially to screen for liver congestion or enlargement
- Echocardiogram: A noninvasive ultrasound of the heart to evaluate its structure and function, search for right-sided failure, and identify related abnormalities such as valvular disease or cardiomyopathies
| Test | Description |
|---|---|
| Blood tests (LFTs) | Measures liver function and enzyme levels |
| Abdominal ultrasound | Assesses liver size, congestion, and structure |
| Echocardiogram | Evaluates heart structure, pumping function, and detects failure |
| CT/MRI scan | Delineates liver anatomy, detects scarring or masses |
| Liver biopsy (rare) | Confirms liver scarring and damage if diagnosis is unclear |
Complications of Cardiac Cirrhosis
Chronic injury from cardiac cirrhosis can lead to serious complications, many of which are similar to those seen with other types of liver cirrhosis. These complications reflect the liver’s reduced capacity to filter toxins, synthesize proteins, and regulate blood flow.
- Esophageal varices: Due to increased pressure in blood vessels that bypass the liver, these veins bulge and may bleed
- Ascites: Fluid accumulation in the abdomen
- Hepatic encephalopathy: Mental confusion due to accumulation of toxins not cleared by the liver
- Infections: Higher risk for bacterial infections (e.g., urinary tract infections)
- Malnutrition: Impaired protein and nutrient synthesis
- Liver cancer (hepatocellular carcinoma)
- Kidney failure: (Hepatorenal syndrome)
- Splenomegaly: Enlarged spleen due to backflow pressure
- Bleeding problems: Reduced clotting factors increase risk of bleeding and bruising
Treatment of Cardiac Cirrhosis
Managing cardiac cirrhosis centers around addressing the underlying right-sided heart failure and its causes, as well as providing supportive care for liver function. Treatment plans are highly tailored, targeting the mechanism of heart dysfunction driving liver congestion. Early intervention may improve outcomes and avoid further liver damage.
| Underlying Cause | Treatment Approach |
|---|---|
| Chronic lung disease (cor pulmonale) | Identify and manage lung conditions |
| Pulmonary embolism | Anticoagulation therapy |
| Heart valve disorders | Valve repair or replacement surgery |
| Electrical delays (bundle branch block) | Biventricular pacemaker or cardiac resynchronization therapy |
| Left ventricular failure | Medications such as beta-blockers, ARNI, MRA, SGLT2 inhibitors |
Directed medications commonly used for right- and left-sided heart failure include:
- Beta-blockers: Lower blood pressure, ease strain on the heart
- ACE inhibitors/ARBs/ARNI: Manage high blood pressure and protect kidney function
- MRA (Mineralocorticoid receptor antagonists): Reduce swelling and manage blood pressure
- SGLT2 inhibitors: Help regulate blood sugar and lower cardiovascular risk, especially in adults with diabetes
Other supportive measures may involve diuretics for fluid overload, dietary sodium restriction, and careful monitoring of kidney and liver function. Advanced liver disease may require transplant evaluation, though the underlying cardiac dysfunction must also be treated.
Outlook and Prognosis of Cardiac Cirrhosis
The prognosis for cardiac cirrhosis varies and depends on several factors, including the severity of underlying heart failure, how rapidly congestion is reversed, and progression of liver damage. Timely diagnosis and successful management of the heart condition are vital for improving long-term outcomes. Without intervention, ongoing liver injury may culminate in irreversible cirrhosis and life-threatening complications.
- Early identification and intervention can slow or halt progression
- Prognosis worsens when both heart and liver function decline together
- Ongoing medical care and lifestyle modifications are essential for optimal results
Frequently Asked Questions (FAQs)
Q: What makes cardiac cirrhosis different from other forms of cirrhosis?
A: Cardiac cirrhosis is uniquely caused by chronic heart failure, especially right-sided failure, leading to liver congestion. Other forms of cirrhosis often arise from viral infections, alcohol misuse, or autoimmune diseases.
Q: Can cardiac cirrhosis be reversed?
A: Early cardiac cirrhosis may improve if the underlying heart condition is corrected and congestive hepatopathy resolves. Established liver scarring is usually permanent, but further deterioration can often be prevented with proper treatment.
Q: What are the most important symptoms to watch for?
A: Swelling in the legs or abdomen, jaundice, fatigue, and confusion are key signs. However, symptoms can be mild or absent until advanced stages.
Q: How is cardiac cirrhosis diagnosed?
A: Diagnosis involves blood tests for liver function, imaging studies such as ultrasound, and an echocardiogram to assess heart function. Sometimes a liver biopsy may be necessary.
Q: What are the main treatments?
A: Addressing the underlying heart problem is crucial. This may include medications, surgery, and supportive care for liver function. Treating complications and preventing further damage are also important aspects of therapy.
Key Takeaways: Safeguarding Both Heart and Liver Health
- Cardiac cirrhosis is a direct consequence of chronic heart failure and impaired circulation, with far-reaching effects on liver function.
- Prompt diagnosis and treatment of the underlying cardiac disorder can often prevent or slow the progression of liver damage.
- Regular follow-up, healthy lifestyle choices, and management of risk factors are pivotal for preserving organ health and quality of life.
References
- https://www.healthline.com/health/heart/cardiac-cirrhosis
- https://www.medicalnewstoday.com/articles/cardiac-cirrhosis
- https://www.healthline.com/health/cirrhosis
- https://www.medicalnewstoday.com/articles/172295
- https://www.healthline.com/health/video/ask-the-expert-the-risks-of-heart-failure
- https://www.healthline.com/health/video/how-to-prevent-heart-disease-according-to-a-cardiologist
- https://www.chp.gov.hk/en/static/80032.html
- https://www.ncbi.nlm.nih.gov/books/NBK431053/
- https://www.healthline.com/health/video/5-foods-for-your-liver
- https://www.mountelizabeth.com.sg/health-plus/article/fatty-liver-myths-facts
Read full bio of medha deb












