Cardiac Asthma: Causes, Symptoms, Diagnosis, and Treatment
Explore the causes, symptoms, and essential treatments for cardiac asthma, a heart failure complication that mimics classic asthma.
Everything You Need to Know About Cardiac Asthma
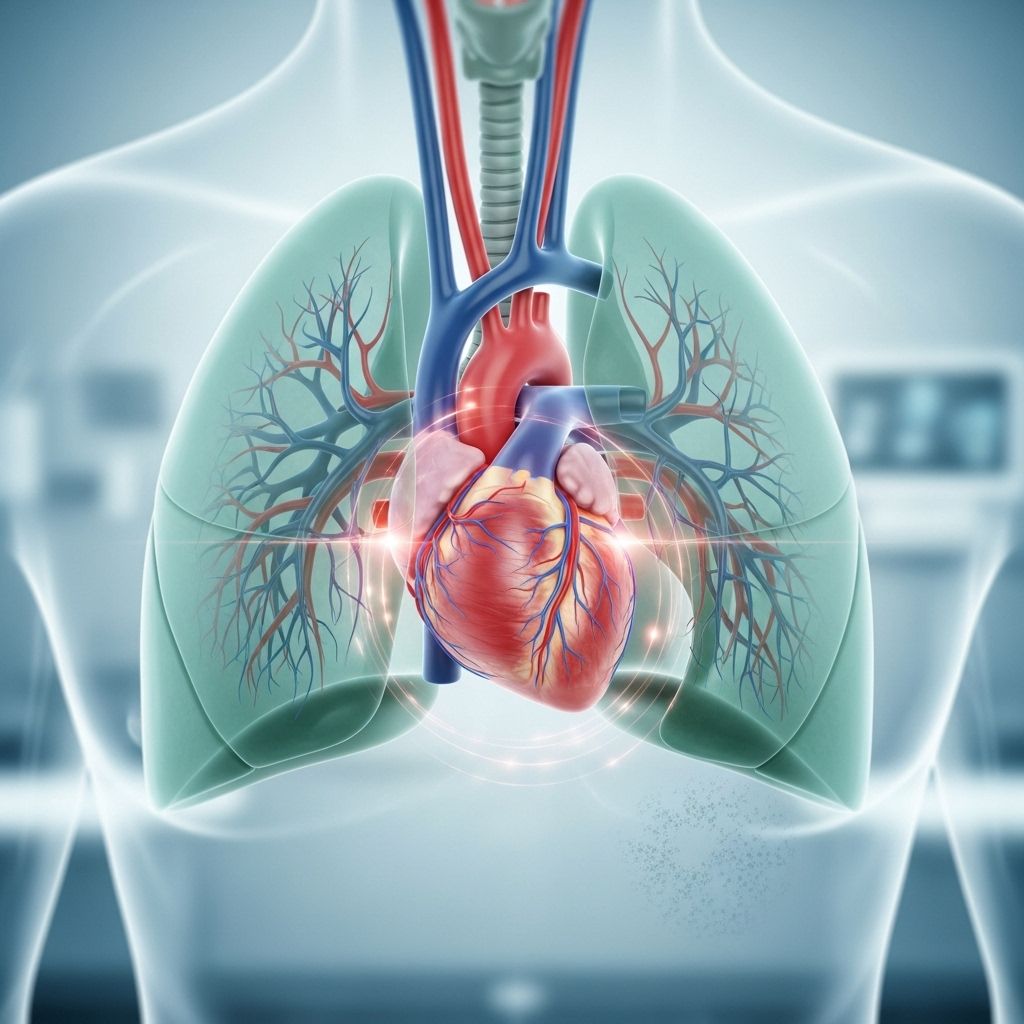
Cardiac asthma refers to a group of respiratory symptoms—especially wheezing, shortness of breath, and coughing—triggered by congestive heart failure. While the symptoms mimic classic asthma, the underlying cause is rooted in heart dysfunction rather than airway inflammation. Accurate recognition and management are critical, as cardiac asthma can be potentially life threatening if left untreated.
What Is Cardiac Asthma?
The medical term cardiac asthma describes asthma-like breathing difficulties caused by fluid accumulation in the lungs due to heart failure. Coined by Dr. James Hope in 1833, the term remains relevant in modern cardiology.
- Cardiac asthma is not a true form of bronchial asthma.
- Symptoms result from the heart’s inability to pump blood efficiently, backing up pressure into pulmonary blood vessels.
- This backup causes leakage of fluid into the lungs, leading to pulmonary congestion and edema.
The heart consists of four chambers: the left and right atria, and the left and right ventricles. In heart failure, where the left ventricle cannot pump effectively, blood pressure rises within the veins of the lungs, and fluid escapes into the lung tissue. This impairs normal oxygen exchange and leads to the respiratory distress characteristic of cardiac asthma.
Symptoms of Cardiac Asthma
Cardiac asthma shares numerous similarities with classic bronchial asthma, leading to frequent misdiagnoses. However, key differences exist. The symptoms primarily result from fluid congestion rather than airway inflammation.
- Wheezing: High-pitched whistling sounds when breathing out, caused by narrowed airways due to fluid pressure.
- Coughing: Often persistent, and can sometimes produce frothy or blood-tinged sputum.
- Shortness of breath (dyspnea): Can occur suddenly, often worsening when lying down (orthopnea).
- Difficulty breathing at night: Symptoms frequently worsen at night or after lying down for an extended period.
- Waking up suddenly from sleep: Also called paroxysmal nocturnal dyspnea.
- Rales: Crackling sounds on lung examination, associated with fluid in the air sacs.
- Chest tightness: Often present with underlying heart failure.
Other features may include rapid breathing, difficulty performing physical activities, swelling in the legs, and fatigue.
Comparing Cardiac Asthma and Bronchial Asthma
| Feature | Cardiac Asthma | Bronchial Asthma |
|---|---|---|
| Underlying Cause | Heart failure (fluid overload in lungs) | Airway inflammation or allergic reactions |
| Key Triggers | Exertion, lying down, heart disease | Allergens, cold air, exercise, irritants |
| Response to Asthma Medications | Poor; classic bronchodilators less effective | Good; bronchodilators and steroids are effective |
| Sputum | Can be frothy, sometimes blood-tinged | Usually clear or mucus-like |
| Associated Symptoms | Leg edema, fatigue, rapid heart rate | Allergic symptoms (runny nose, itching), eczema |
Recognizing these differences helps clinicians avoid misdiagnosis, ensuring the right treatment is provided.
What Causes Cardiac Asthma?
The root cause of cardiac asthma is heart failure, particularly involving the left side of the heart. Heart failure leads to fluid backing up into the lungs, disrupting normal breathing. Some causes and risk factors include:
- Coronary artery disease: Narrowing or blockage of heart arteries, usually from atherosclerosis (plaque and cholesterol buildup).
- Past heart attacks: Heart muscle damage compromising pumping function.
- Abnormal heart rhythms (arrhythmias): Such as atrial fibrillation.
- High blood pressure (uncontrolled): Increases cardiac workload, eventually weakening the heart.
- Heart valve disorders: Leaky or narrowed valves restricting efficient blood flow.
- Cardiomyopathy: Diseases of the heart muscle itself.
- Myocarditis: Inflammation of the heart muscle, often due to viral infections.
- Congenital heart defects: Structural problems present at birth.
- Diabetes: A risk factor for cardiovascular disease.
- Thyroid disorders: Especially hyperthyroidism, increasing cardiac demand.
- Severe lung disease: Can increase pressure in the heart and lung circulation.
- Obesity: Increases the risk of both heart and lung complications.
- Kidney failure: Compromises the body’s ability to manage fluid balance.
- Anemia: Especially if severe, increases cardiac strain.
- Obstructive sleep apnea: Interrupted breathing during sleep stresses the heart.
Often, more than one of these factors coexists, amplifying the risk of cardiac asthma development.
Diagnosis
Diagnosing cardiac asthma requires careful distinction from classic asthma and other respiratory conditions. Accurate diagnosis is vital since treatment strategies differ markedly.
- Medical history and physical exam: Doctors assess symptoms, heart disease risk factors, and listen for abnormal lung sounds like rales.
- Chest X-ray: Reveals fluid accumulation, heart enlargement, or pulmonary edema.
- Electrocardiogram (ECG/EKG): Identifies arrhythmias or heart muscle damage.
- Echocardiogram: Soundwave imaging shows heart function, valve status, and chamber sizes.
- Lung function tests: Can help differentiate cardiac from bronchial asthma.
- Blood tests: Assess kidney function, anemia, thyroid disorders, and markers like BNP indicating heart stress.
- Pulse oximetry or blood gas tests: Check oxygen and carbon dioxide levels in the blood.
Emergency symptoms, such as severe shortness of breath, require immediate evaluation. Misdiagnosis as classic asthma is common, but a thorough approach can reveal the correct diagnosis.
Causes and Risk Factors
While the direct cause is always heart failure or left-sided cardiac dysfunction, certain populations face higher risk:
- Elderly individuals: Heart failure prevalence—and therefore, cardiac asthma—rises with age.
- People with untreated or chronic high blood pressure
- Patients with a previous history of heart disease or heart attack
- People with underlying metabolic, renal, or endocrine disorders
Managing these risk factors plays a vital role in preventing cardiac asthma episodes.
Treatment Options for Cardiac Asthma
Unlike conventional asthma therapies, the hallmark of cardiac asthma treatment is addressing the underlying heart failure and reducing lung fluid overload. This approach is fundamental, as classical bronchodilators are usually minimally effective.
Medications
- Diuretics (furosemide): Help eliminate excess fluid from the body, easing pressure in the lungs.
- Nitroglycerin: Dilates blood vessels, reducing cardiac workload and pulmonary congestion.
- Morphine: Sometimes used to reduce respiratory distress in acute, severe cases (under expert supervision).
- ACE inhibitors: Lower blood pressure and reduce heart strain for longer-term control.
- Beta-blockers: Slow heart rate and lower blood pressure to stabilize the heart’s function.
Individualized treatment plans may include additional agents based on the patient’s overall health and other underlying conditions.
Oxygen and Respiratory Support
- Oxygen therapy: Provided if blood oxygen levels are dangerously low.
- Noninvasive ventilation: Devices like CPAP or BiPAP help keep airways open, easing breathing.
- Mechanical ventilation: In severe or life-threatening cases where standard support fails, intubation may be required.
These interventions are adjusted depending on the severity and immediate risk to the patient’s health.
Surgical and Interventional Approaches
- Coronary angioplasty or bypass surgery: Restores blood flow where blockages are present.
- Valve repair or replacement: Corrects valve dysfunction causing heart failure.
- Implantable cardiac devices: Pacemakers or implantable defibrillators for arrhythmia management in select cases.
- Heart transplant: The final option for advanced, unresponsive heart failure.
How to Manage and Prevent Episodes
- Strictly adhere to all prescribed heart failure medications and instructions.
- Monitor daily weight to detect early fluid retention.
- Adopt a low-sodium diet to help limit fluid buildup.
- Limit fluid intake as directed by a healthcare provider.
- Maintain regular physical activity, as tolerated.
- Control comorbid conditions such as high blood pressure, diabetes, and thyroid disorders.
- Immediately report any sudden changes in breathing or swelling to a healthcare provider.
Outlook and Prognosis
Cardiac asthma is a serious sign of underlying heart failure. When managed appropriately and promptly, symptoms can improve, and repeated episodes can be reduced.
Prognosis depends on:
- The underlying cause of heart failure
- The severity of lung fluid buildup
- Timeliness of treatment
- Presence of other chronic diseases
Frequent cardiac asthma episodes usually indicate deteriorating heart function and may require intensive heart failure management by a cardiologist. Long-term lifestyle changes, medication adherence, and regular follow-ups are essential to minimize future risks.
Frequently Asked Questions (FAQs)
Q: Can cardiac asthma be cured?
A: Cardiac asthma itself can improve or resolve with effective treatment and management of underlying heart failure. However, cure is only possible if the underlying heart problem can be fully reversed. Most people require ongoing therapy and lifestyle adjustments.
Q: Are inhalers or classic asthma medications useful for cardiac asthma?
A: Bronchodilator inhalers and corticosteroids, common in classic asthma, generally do not provide significant relief for cardiac asthma, since the cause is not airway inflammation but fluid overload.
Q: How is cardiac asthma different from bronchial asthma?
A: Cardiac asthma is triggered by heart failure and lung fluid overload, whereas bronchial asthma is an inflammatory airway disease often linked to allergies or irritants.
Q: When should I seek immediate medical attention?
A: Severe breathing difficulties, coughing up pink frothy sputum, sudden swelling in the legs, or chest pain all warrant immediate emergency medical care.
Q: Who is most at risk for cardiac asthma?
A: Older adults, those with known heart failure, people with previous heart attacks or valve disorders, and those with poorly controlled high blood pressure or kidney disease face the highest risk.
Q: Can lifestyle changes reduce the risk?
A: Yes! Effective management of blood pressure, cholesterol, diabetes, along with avoiding smoking and limiting alcohol, lowers the risk of heart failure and related cardiac asthma episodes.
Key Takeaways
- Cardiac asthma mimics classic asthma but results from heart failure and pulmonary fluid overload.
- Symptoms include wheezing, cough, and shortness of breath—often misdiagnosed as bronchial asthma.
- Treatment focuses on reducing lung fluid and supporting heart function, not standard asthma therapies.
- Proper diagnosis and compliance with heart failure management are vital for a positive outlook.
- Ongoing monitoring and healthy lifestyle choices significantly lower long-term risks.
References
- https://www.uspharmacist.com/article/cardiac-asthma-not-your-typical-asthma
- https://www.healthline.com/health/heart-disease/cardiac-asthma
- https://www.heart.org/en/news/2024/05/17/how-are-asthma-and-heart-health-linked
- https://www.ahajournals.org/doi/10.1161/01.CIR.4.6.920
- https://www.healthline.com/health/asthma
- https://www.medicalnewstoday.com/articles/cardiac-asthma
- https://www.healthline.com/health/video/asthma
- https://www.nhlbi.nih.gov/news/2022/asthma-linked-cardiovascular-disease-risks
Read full bio of medha deb












