CAR T-Cell Therapy for Small Cell Lung Cancer: Innovations and Challenges
Discover how CAR T-cell therapy is transforming the outlook for small cell lung cancer with new innovations and ongoing challenges.
Small cell lung cancer (SCLC) is a highly aggressive form of lung cancer known for rapid growth, early metastasis, and a tendency to relapse even after initial treatment success. Although chemotherapy and immunotherapy remain standard, the prognosis for most patients is poor, creating an urgent need for innovative treatments. One of the most promising developments in recent years is chimeric antigen receptor (CAR) T-cell therapy, a novel form of immunotherapy that genetically engineers a patient’s own immune cells to better recognize and destroy cancer cells. This article explores the science, current research, benefits, risks, and future landscape of CAR T-cell therapy in the context of SCLC.
Understanding Small Cell Lung Cancer
SCLC accounts for approximately 15% of all lung cancer cases. Unlike non-small cell lung cancer (NSCLC), SCLC tends to grow rapidly and is often diagnosed at an advanced stage, with about two-thirds of patients presenting with metastatic disease at diagnosis. SCLC is highly sensitive to chemotherapy initially, but relapse is common, and subsequent treatments are much less effective, resulting in a median survival of just over a year for most patients.
- Rapid growth and early spread are hallmarks of SCLC.
- Limited treatment options are available after first-line therapy fails.
- Prognosis is poor due to aggressive disease behavior and high relapse rate.
What Is CAR T-Cell Therapy?
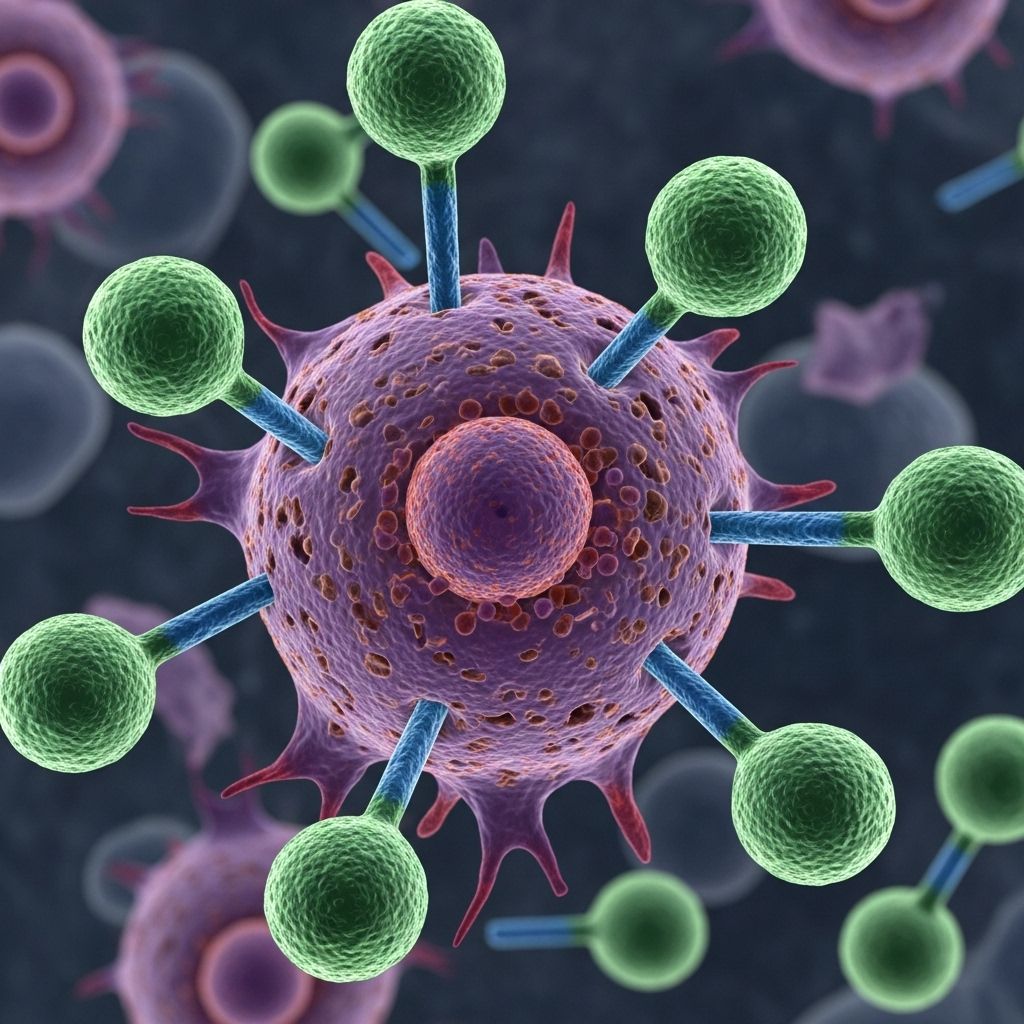
CAR T-cell therapy is a form of immunotherapy that modifies a patient’s own T cells — a type of white blood cell — to help them better identify and attack cancer cells. The process involves extracting T cells from the patient, engineering them in a laboratory to express a chimeric antigen receptor (CAR) that recognizes specific antigens on cancer cells, and then infusing these supercharged cells back into the patient.
How CAR T-Cell Therapy Works
- Collection: Blood is drawn from the patient to isolate T cells.
- Modification: The T cells are genetically altered in the lab to produce CARs on their surfaces.
- Multiplication: Millions of these engineered T cells are grown in the lab.
- Infusion: The modified CAR T cells are infused back into the patient’s bloodstream, where they seek out and destroy cancer cells expressing the target antigen.
This approach has demonstrated remarkable success in some blood cancers, including certain types of leukemia and lymphoma, and is now being explored for solid tumors such as SCLC.
The Role of CAR T-Cell Therapy in SCLC
Due to SCLC’s aggressive nature and propensity for recurrence, there is robust scientific interest in applying CAR T-cell therapy to this malignancy. Research focuses especially on the use of CAR T cells designed to target delta-like ligand 3 (DLL3), a protein highly expressed on SCLC cells but limited on normal tissues.
DLL3: The Target Antigen
- DLL3 is an abnormal protein found on the surface of most SCLC cells.
- Because DLL3 is largely absent from healthy tissues, it makes an attractive target for therapies, limiting collateral damage to normal cells.
Notable Innovations: Armored CAR T Cells
A major breakthrough in recent research involves engineering CAR T cells to secrete interleukin-18 (IL-18), an inflammation-regulating protein that boosts immune system action inside tumors. These are referred to as “armored” CAR T cells and have exhibited dramatically increased anti-tumor activity in animal models.
- IL-18-secreting CAR T cells multiply more effectively and persist longer in the body.
- These cells remember the DLL3 antigen, enhancing the likelihood of ongoing tumor surveillance.
- Armored CAR T therapy also increases the presence of tumor-infiltrating lymphocytes, further strengthening anti-tumor immunity.
Combination Approaches: Immune Checkpoint Inhibitors
Studies show that combining IL-18-secreting CAR T cells with immune checkpoint inhibitors — drugs that block cancer’s ability to hide from the immune system — can further enhance cancer cell killing.
Benefits and Potential of CAR T-Cell Therapy in SCLC
- Personalized treatment: Each CAR T product is tailored to an individual’s unique cancer profile.
- Target specificity: By focusing on markers like DLL3, CAR T cells are less likely to harm healthy tissue.
- Durable responses: Animal models have shown complete eradication of recurrent tumors with armored CAR T cells.
- Memory effect: Engineered T cells may persist, recognizing and destroying cancer cells that reappear.
Current Research and Clinical Trials
While the majority of CAR T-cell success stories are from blood cancers, several preclinical and early clinical studies are paving the way for SCLC therapy.
| Innovation | Findings | Status |
|---|---|---|
| DLL3-targeted CAR T cells | Effective tumor targeting, notable safety in preclinical models. | Preclinical/early clinical |
| Armored CAR T cells secreting IL-18 | Enhanced anti-tumor activity, improved survival, less T cell exhaustion, stronger memory response. | Preclinical |
| Combination with immune checkpoint inhibitors | Stronger, longer-lasting responses in animal models. | Preclinical |
| Clinical trial with tarlatamab (DLL3-targeted drug) | Tumor shrinkage in 32–40% of previously treated patients, with some lasting over nine months. | Phase II clinical trial |
Notably, the immunotherapy tarlatamab (though not a CAR T product) targets DLL3 and has recently shown meaningful tumor responses in clinical trials, further supporting DLL3 as a viable target for SCLC treatment innovation.
Challenges and Limitations
Despite promising advances, CAR T-cell therapy for SCLC faces several obstacles that must be addressed before the treatment becomes widely available:
- Solid tumor environment: SCLC tumors create a hostile, immunosuppressive microenvironment that impedes T cell function and survival.
- Antigen escape: Tumors can evolve and stop expressing the target antigen, evading CAR T-cell detection.
- Safety concerns: Serious immune-related side effects, including cytokine release syndrome (CRS) and neurological toxicity, can occur and must be carefully managed.
- Treatment resistance: Some patients may not respond or may experience disease recurrence after CAR T-cell therapy.
- Manufacturing complexity: Creating patient-specific CAR T products is time-consuming, expensive, and may be impractical for some fast-progressing SCLC cases.
Pioneering Approaches on the Horizon
Researchers are actively developing new strategies to overcome the hurdles faced by CAR T-cell therapy in SCLC and other solid tumors:
- Armored CAR T cells: Engineering cells to secrete cytokines (such as IL-18) increases potency and persistence.
- Allogeneic (off-the-shelf) CAR T cells: Universal donor-derived CAR T treatments may make therapy faster and more accessible.
- Dual-targeting CARs: Designing receptors that recognize more than one marker may limit antigen escape.
- Combination therapies: Integrating CAR T cells with checkpoint inhibitors or other immunomodulatory drugs could amplify efficacy.
- Improved delivery systems: Direct injection into tumors or alternative infusion routes are being explored to enhance tumor penetration and activity.
What to Expect: Process of Receiving CAR T-Cell Therapy
CAR T-cell treatment is a multi-step process that can last several weeks. The typical stages are:
- Evaluation: Determining if the patient is a candidate for CAR T therapy, based on disease status and health.
- Collection: Leukapheresis procedure draws and separates T cells from the patient’s blood.
- Cell Engineering: The lab modifies the T cells, which then expand to large numbers over weeks.
- Pre-conditioning: Chemotherapy may be administered to prepare the body for CAR T infusion.
- Infusion: The finished CAR T cells are returned to the patient via IV.
- Monitoring: Intensive observation for side effects and early response over the next days and weeks, usually in a hospital or specialized center.
Potential Side Effects and Risks
Like other advanced immunotherapies, CAR T-cell therapy carries risks:
- Cytokine release syndrome (CRS): Overactivation of the immune system causing high fever, low blood pressure, and potentially severe complications. Most cases are manageable.
- Neurotoxicity: Confusion, seizures, or brain swelling in rare cases. Usually reversible but potentially serious.
- Risk of infections: Immune suppression during therapy can increase susceptibility to infection.
- Other reactions: Fatigue, muscle pain, and low blood counts may occur.
Close medical supervision in an expert cancer center is crucial during and after treatment.
Who Might Benefit?
At present, nearly all clinical trials for CAR T-cell therapy in SCLC are focused on individuals who:
- Have relapsed or refractory SCLC that progressed after standard treatments.
- Are otherwise healthy and fit enough to undergo the intensive workup and side-effect management required for CAR T therapy.
Frequently Asked Questions (FAQs)
Q: What is the current status of CAR T-cell therapy for SCLC?
A: CAR T-cell therapy for SCLC is still considered experimental and is only available through clinical trials at specialized cancer centers. Preclinical studies are highly promising. Further human trials are ongoing.
Q: What makes DLL3 a promising target for CAR T therapy?
A: DLL3 is selectively expressed on most SCLC tumor cells but not on healthy tissues, which allows for precise targeting with minimal off-tumor effects.
Q: How is CAR T-cell therapy different for solid tumors compared to blood cancers?
A: Solid tumors like SCLC pose challenges such as difficult tumor penetration, immunosuppressive microenvironments, and potential antigen escape. Blood cancers are generally more accessible to immune cells and have demonstrated greater success with CAR T-cell therapy thus far.
Q: Are there risks of serious side effects?
A: Yes. CAR T-cell therapy can cause serious side effects, particularly cytokine release syndrome and neurotoxicity. These require close medical monitoring.
Q: Is CAR T-cell therapy a cure for SCLC?
A: While early animal studies show complete tumor responses, there is no evidence yet that CAR T therapy can cure SCLC in humans. Ongoing trials seek to determine its true potential.
Outlook and Future Directions
CAR T-cell therapy represents a cutting-edge advance in the quest to improve survival and quality of life for people with SCLC. Ongoing innovations — including armored CAR design, new target selection, and sophisticated combinations with other drugs — offer hope for future breakthroughs. However, much work remains to overcome the unique hurdles presented by SCLC and bring these treatments from research to routine clinical practice. Participation in clinical trials is crucial for both advancing science and providing patients access to potentially transformative therapies.
References
- https://www.roswellpark.org/newsroom/202304-new-car-t-cell-strategy-highly-effective-against-small-cell-lung-cancer-preclinical
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11082704/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7475572/
- https://www.cancer.gov/news-events/cancer-currents-blog/2023/tarlatamab-previously-treated-sclc
- https://cdmrp.health.mil/lcrp/research_highlights/23Weiss_Savoldo_highlight
- https://www.mdanderson.org/cancerwise/what-s-new-in-car-t-cell-therapy–solid-tumor-advances.h00-159617856.html
- https://hollingscancercenter.musc.edu/news/archive/2024/08/23/new-therapy-for-small-cell-lung-cancer-offered-at-hollings
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1448438/full
Read full bio of medha deb












