Can You Die from Angina? Risks, Complications, and Prevention
Understanding angina, its direct dangers, and how it relates to the risk of heart attack, complications, and prevention.
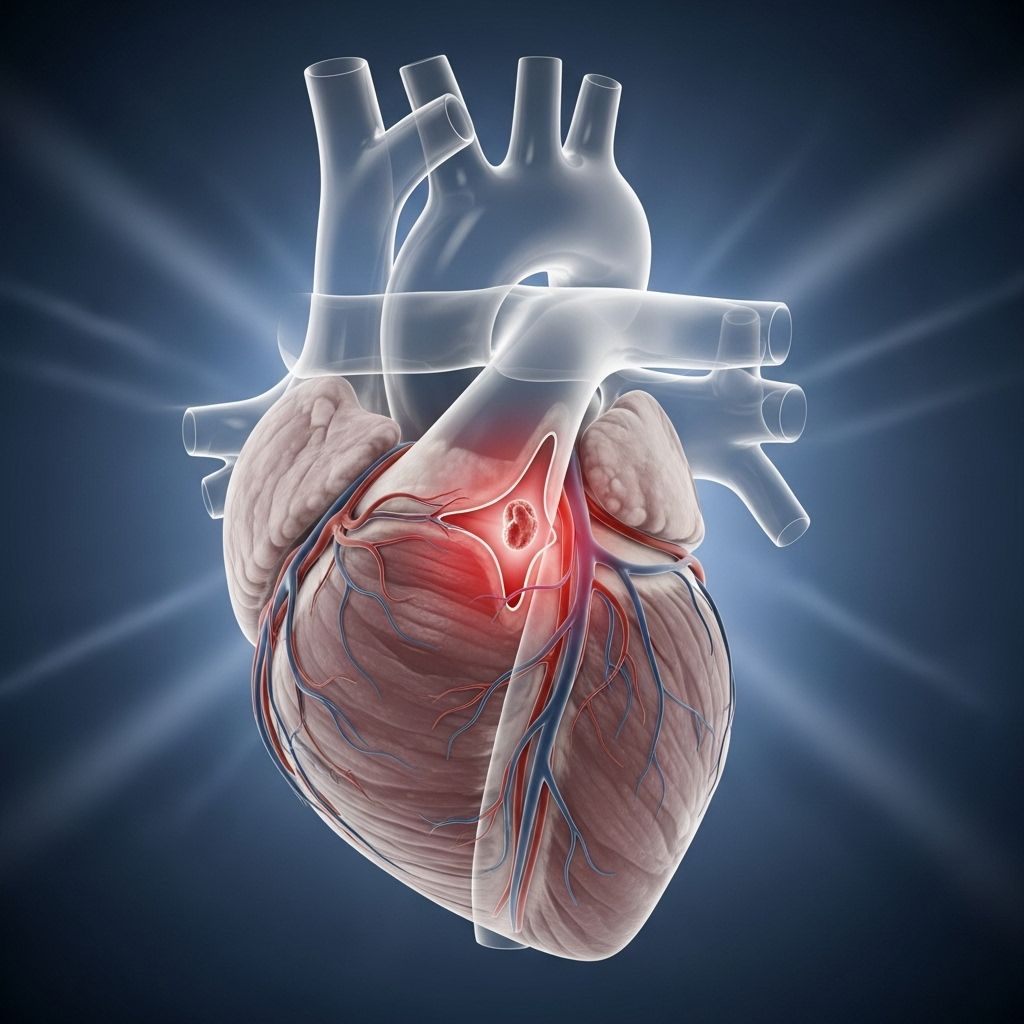
Angina is a common symptom of heart disease, manifesting as chest pain or discomfort when your heart doesn’t receive enough oxygen-rich blood. But how deadly is angina itself? Does it always mean a heart attack is coming? This in-depth article explores these questions, highlighting the differences between angina and heart attacks, complications, when to be concerned, and preventive strategies for improved heart health.
What Is Angina?
Angina refers to chest pain or discomfort that signals a temporary reduction in blood flow to the heart muscle. It is not a condition but a symptom, often associated with underlying coronary artery disease (CAD). This discomfort can also spread to the shoulders, neck, back, jaw, or arms. Angina does not cause permanent damage itself but indicates problems with the heart’s blood supply, making it an important warning sign for more serious conditions like heart attacks.
- Stable angina occurs predictably, typically during physical exertion or stress, and is relieved by rest or medication.
- Unstable angina is more unpredictable, may happen at rest, and is considered a medical emergency.
Does Angina Cause Death?
Angina by itself is not usually fatal. The pain or discomfort from angina usually ceases with rest or medication and does not cause permanent heart muscle injury. However, angina is a strong indicator of underlying coronary artery disease, which can result in serious, potentially fatal complications if left untreated.
It is crucial to remember:
- While angina itself does not kill, it is a significant marker of increased risk for life-threatening events such as heart attack or arrhythmias.
- Unstable angina, which worsens or occurs at rest, can signal imminent heart attack.
- People with angina are more likely to develop serious heart problems over time if the underlying disease is not addressed.
The Link between Angina and Heart Attack
A heart attack (myocardial infarction) happens when blood flow to part of the heart is severely reduced or completely blocked, causing death of heart tissue. Angina develops when there is a reduction in blood flow, but not complete blockage. However, the presence of angina indicates that the coronary arteries are significantly narrowed or compromised, setting the stage for a heart attack.
| Angina | Heart Attack |
|---|---|
| Temporary chest pain, no permanent damage | Chest pain due to permanent damage (heart muscle dies) |
| Triggered by exertion or stress | Often occurs at rest or after exertion |
| Relieved by rest or medication | Does not respond to rest or nitroglycerin |
| Signals underlying heart disease | Medical emergency, requires immediate action |
Key Symptoms Comparison
- Angina: Chest discomfort or pressure, may radiate, usually stops with rest.
- Heart Attack: Severe and persistent chest pain, shortness of breath, nausea, lightheadedness, sweating, pain radiating to arm or jaw, often does not subside with rest.
Can Angina Progress to a Heart Attack?
Not everyone with angina will have a heart attack. Nevertheless, experiencing angina means you are at increased risk of experiencing a heart attack in the future.
- Stable angina generally means there are blockages, but a trigger such as a rupture of a plaque may suddenly block a coronary artery, leading to a heart attack.
- Unstable angina or angina that becomes more frequent, severe, or comes on with less exertion is a red flag—this may indicate a developing heart attack or other complications and demands immediate medical evaluation.
Data shows people with existing angina have a heightened long-term risk of heart attacks, heart failure, arrhythmias, and cardiac death if their underlying heart disease progresses untreated.
Types of Angina and Their Significance
- Stable Angina: Occurs in predictable patterns, e.g., with exercise. Signals coronary artery narrowing; if it doesn’t change in frequency or intensity, the risk of imminent heart attack is lower but present over time.
- Unstable Angina: Sudden onset, worsening, or occurring at rest. Highly dangerous, may signal a developing heart attack or significant blockage. Medical emergency.
- Microvascular Angina: Pain from abnormalities in the heart’s smallest blood vessels. More common in women, and long-term risk remains significant.
- Variant (Prinzmetal’s) Angina: Caused by spasms in coronary arteries, not always associated with atherosclerosis.
What Causes Angina?
- Coronary Artery Disease (CAD): The main cause, where plaque builds up in coronary arteries, restricting blood flow.
- Vasospasm: Spasms cause temporary narrowing of arteries even with no underlying disease.
- Other Conditions: Severe anemia or abnormal heart rhythms can also reduce oxygen supply, provoking angina.
Atherosclerosis (plaque buildup inside arteries) is the most frequent underlying process, often developing over years, sometimes without symptoms until significant narrowing exists.
Recognizing Symptoms of Angina
- Chest pain, pressure, tightness, or squeezing
- Pain extending to shoulders, arms, neck, jaw, or back
- Shortness of breath
- Nausea or indigestion
- Dizziness or lightheadedness
- Fatigue or weakness
- Cold sweat
Not everyone will experience severe pain. Some, especially women and older adults, may present with vague symptoms like fatigue or mild discomfort.
When to Seek Emergency Help
Immediate medical attention is required if:
- Chest pain lasts more than 10 minutes or worsens
- Pain is severe, persistent, or different from your usual angina
- You experience angina at rest or at night
- Symptoms accompany shortness of breath, fainting, or profuse sweating
- Angina doesn’t resolve with prescribed medication (such as nitroglycerin)
Unstable angina cannot be distinguished from a heart attack without medical evaluation, so when in doubt, call emergency services immediately.
Are You at Greater Risk of Complications?
Angina is strongly associated with risk for serious heart problems. Factors that increase risk for complications include:
- Advancing age (especially men over 45 or women over 55)
- Family history of heart disease
- High blood pressure, high cholesterol, or diabetes
- Smoking
- Obesity or physical inactivity
- Chronic stress
- Poor dietary habits
Addressing these risk factors is essential in reducing future complications and improving longevity for those with angina.
How Is Angina Diagnosed?
- Physical examination: Assessment of symptoms, risk factors, and family history
- Electrocardiogram (ECG): Checks for changes indicating decreased blood flow
- Stress testing: Monitors how the heart responds to physical exertion
- Imaging: Echocardiogram or coronary angiography to pinpoint blockages
- Blood tests: To rule out or confirm heart attack
Treatment of Angina: Lowering Your Risk
- Lifestyle changes: Adopting a heart-healthy diet, regular exercise, quitting smoking, managing stress, and maintaining a healthy weight
- Medications: Nitrates (often nitroglycerin), beta-blockers, calcium channel blockers, statins, ACE inhibitors, and antiplatelet agents
- Medical procedures: When blockages are severe, angioplasty or bypass surgery may be required
Treating angina’s underlying cause, rather than just relieving pain, is the key to preventing fatal complications.
Preventing Complications and Protecting Your Heart
- Know and control your risk factors: Manage blood pressure, cholesterol, and blood sugar.
- Follow your treatment plan: Take all medications as prescribed and attend regular check-ups.
- Adopt a heart-healthy lifestyle:
- Eat a balanced diet, low in saturated fat and salt
- Exercise regularly (upon your doctor’s advice)
- Maintain a healthy weight
- Stop smoking and limit alcohol
- Practice stress management techniques
- Respond promptly to new or changing symptoms: Seek emergency care if your angina worsens or is accompanied by other symptoms.
Living With Angina: What to Expect
With appropriate management, many people with angina live long, fulfilling lives. However, ongoing monitoring and adjustment of treatment are usually necessary. Understanding your symptoms, triggers, and the warning signs of heart attack is crucial for long-term health and safety.
Always communicate changes in your condition to your healthcare team, and never ignore new or worsening symptoms.
Frequently Asked Questions (FAQs)
Is angina always a sign of an impending heart attack?
Stable angina is not necessarily a warning that a heart attack is imminent, but it does indicate you are at higher risk over time. Unstable angina, however, is a medical emergency and may precede a heart attack.
How do I distinguish between angina and a heart attack?
Angina typically subsides with rest or medication, while a heart attack causes persistent, worsening pain that does not improve. However, only a healthcare professional can accurately differentiate, so seek help for any new or severe chest pain.
Can angina be cured?
Angina is a sign of underlying heart problems. While symptoms can be managed and risks reduced, the underlying coronary artery disease can be slowed or controlled, but not always cured. Treatment and lifestyle changes are essential.
What lifestyle changes help prevent worsened angina or heart attack?
Main steps include quitting smoking, healthy eating, regular exercise, controlling weight, and managing conditions like diabetes and hypertension.
Should I worry if my angina changes?
Yes. Increasing frequency, duration, or intensity of angina—or angina that occurs at rest—requires immediate evaluation, as this could indicate an unstable situation, increasing the risk of a heart attack or other severe outcomes.
Understanding angina and taking proactive measures greatly reduce the risk of complications. Regular check-ups, adherence to treatment, and lifestyle modifications remain the best protections for your heart health.
References
- https://www.healthline.com/health/heart/angina-vs-heart-attack
- https://www.healthline.com/health/heart/angina-coronary-artery-disease-comparison
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/heart-conditions-angina
- https://www.medicalnewstoday.com/articles/8886
- https://www.ncbi.nlm.nih.gov/books/NBK557672/
- https://medlineplus.gov/angina.html
- https://www.heart.org/en/health-topics/heart-attack/angina-chest-pain/angina-pectoris-stable-angina
- https://www.mayoclinic.org/diseases-conditions/angina/symptoms-causes/syc-20369373
- https://www.thecardiologyadvisor.com/features/angina-vs-heart-attack/
Read full bio of medha deb












