Can Optometrists Diagnose Macular Degeneration? Roles, Tests, and Next Steps
Explore how optometrists detect, diagnose, and help manage macular degeneration, and when to see a specialist.
Can an Optometrist Diagnose Macular Degeneration?
Macular degeneration is a common, progressive eye condition that leads to central vision loss, particularly in older adults. One crucial question frequently asked is whether an optometrist can adequately diagnose this condition during routine eye exams or if it requires more specialized care. This comprehensive guide details the roles of optometrists in detecting macular degeneration, the diagnostics they use, and when it’s necessary to seek care from an ophthalmologist or retina specialist.
About Optometrists: Your Primary Eye Care Providers
Optometrists are healthcare professionals with specialized training in basic eye care. They provide vision assessments, prescribe glasses and contact lenses, and diagnose a variety of eye conditions. Here’s what to know about their education and capabilities:
- Educational journey: Optometrists typically undergo a four-year undergraduate degree followed by four more years at a college of optometry to earn a Doctor of Optometry (OD) degree.
- Scope of practice: Optometrists can perform comprehensive eye exams, diagnose some infections and conditions, prescribe corrective lenses, and in some locations, conduct minor procedures like laser correction for cataracts.
- Limits: While adept at identifying early eye problems, optometrists are not usually licensed to perform major surgeries or manage advanced, sight-threatening eye diseases independently.
For serious or advanced conditions such as macular degeneration, optometrists often play a key role in initial detection and referral to specialists for further treatment.
What is Macular Degeneration?
Macular degeneration—specifically age-related macular degeneration (AMD)—is a condition where the macula, a small but vital part of the retina, gradually deteriorates. This loss impacts central vision, making daily tasks like reading, driving, and facial recognition challenging.
| Feature | Description |
|---|---|
| Location | Macula, center of the retina |
| Function | Sharp, detailed central vision |
| Main population affected | Adults over 50 |
| Symptoms | Blurring or loss of central vision, distortion, difficulty with detailed tasks |
Types of Macular Degeneration
- Dry AMD: The most common form. It occurs gradually as parts of the macula thin and waste products build up, causing slow vision loss.
- Wet AMD: Less common but more severe. Abnormal, leaky blood vessels grow under the retina, often leading to rapid central vision loss.
Both types require early detection for best outcomes, but their treatments and progression rates differ significantly.
How is Macular Degeneration Diagnosed?
Diagnosis of macular degeneration involves several specialized eye tests, most of which can be initiated by an optometrist during a routine eye exam:
- Visual acuity testing: Measures clarity of vision at various distances using an eye chart.
- Pupil dilation: Special eye drops are used to dilate (enlarge) the pupil, allowing the provider to examine the back of the eye, including the retina and macula, for visible changes.
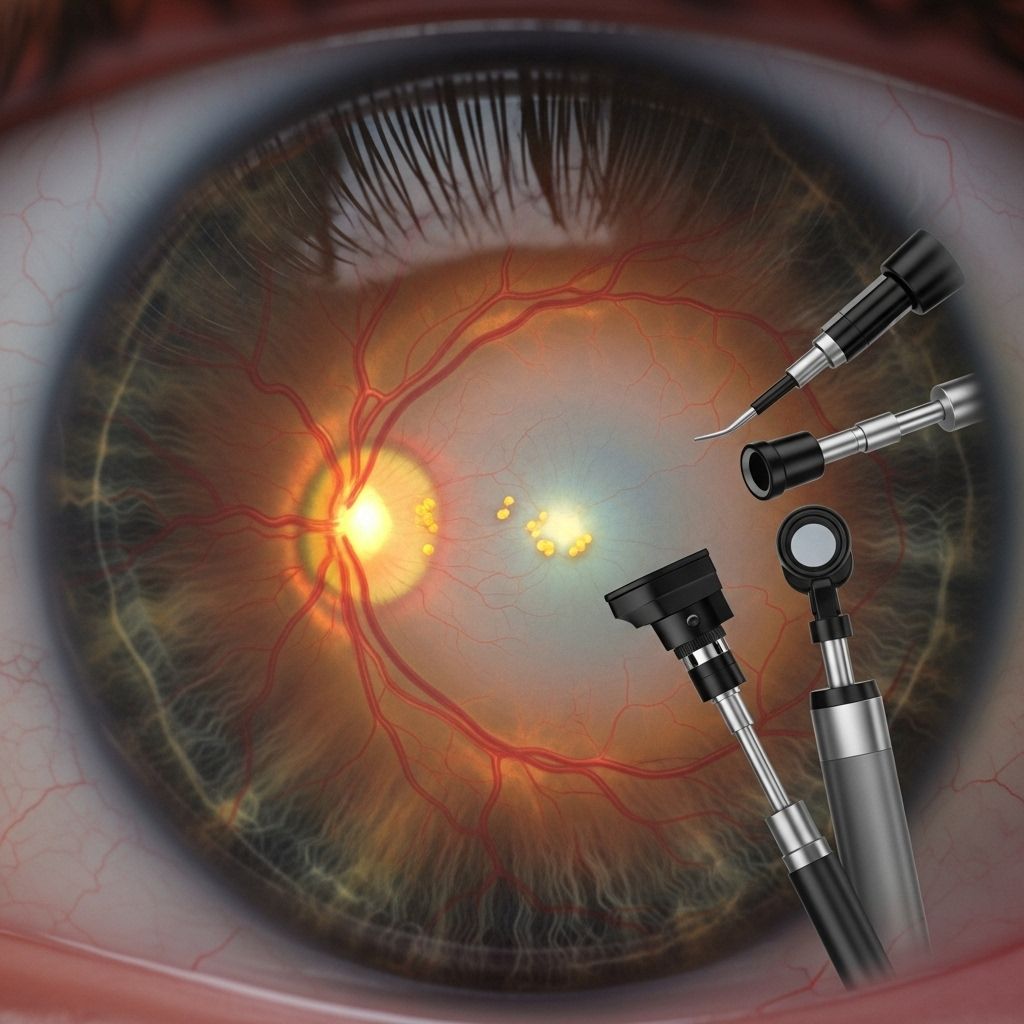
- Retinal imaging: Techniques such as fundus photography or OCT (optical coherence tomography) generate detailed images of the retina, revealing thinning, fluid buildup, or drusen (yellow deposits typical in AMD).
- Fundoscopy/ophthalmoscopy: After dilation, a bright beam of light is directed into the eye to inspect the interior structures for any abnormalities.
- Tonometry: Measures internal eye pressure, which, while most relevant for glaucoma, may be part of routine exams assessing overall eye health.
- Autofluorescence: Specialized photos identify damaged retinal tissue and quantify progression, especially in advanced dry AMD.
- Fluorescein angiography: For suspected wet AMD, a dye is injected into a vein, then retinal blood vessels are examined for leakage or abnormal growth.
Many modern optometry practices have access to advanced imaging tools like OCT. However, if the findings suggest advanced disease or complex presentation, patients are often referred to an ophthalmologist or retina specialist for confirmation and more detailed management.
Comparison Table: Optometrist vs. Ophthalmologist in Diagnosing and Treating AMD
| Provider | Diagnosing AMD | Treating Early AMD | Treating Advanced AMD |
|---|---|---|---|
| Optometrist | Yes (initial detection, some imaging) | Yes (lifestyle advice, monitor progression) | No (refers to specialist for therapies) |
| Ophthalmologist | Yes (comprehensive diagnosis) | Yes (full scope or referral) | Yes (medical and surgical treatments) |
Detailed Review: Diagnostic Tests for Macular Degeneration
An eye exam for suspected AMD usually involves a combination of the following:
- Visual Acuity Test: Determines how well you see at different distances.
- Dilated Eye Exam: Allows a thorough look at the retina and macula for drusen or pigment changes.
- OCT (Optical Coherence Tomography): Non-invasive scan providing detailed images and cross-sections of the retina, critical for detecting thinning or swelling.
- Fundus Photography: Documents the back of the eye for progression tracking.
- Fluorescein Angiography: Used mainly if wet AMD is suspected, identifies abnormal vessel growth and leakage.
- Amsler Grid: A simple grid test used to check for wavy lines or missing areas in your central vision.
Some of these tests are standard in optometry clinics; others, like angiography, are typically performed by ophthalmologists or retina specialists.
Can Optometrists Treat Age-Related Macular Degeneration?
Optometrists can identify the early signs and risk factors for AMD, offer lifestyle guidance, and monitor progression but do not provide advanced medical or surgical treatments for the disease. If AMD is suspected or confirmed—especially if it’s progressing—patients are almost always referred to an ophthalmologist or retina specialist for further assessment and care.
Role of Optometrists in AMD Management
- Monitoring and Early Detection: Through regular exams, optometrists monitor changes over time, allowing for timely referrals when disease progression is detected.
- Preventive Counseling: Recommendations may include dietary modifications, increased antioxidant intake, smoking cessation, and UV protection to slow AMD progression.
- Supplements: For certain patients, optometrists may recommend AREDS2 supplements (formulated specifically for macular health) to help reduce the risk of advanced AMD.
Definitive treatment for wet AMD—primarily anti-VEGF injections—must be administered by an ophthalmologist or retina specialist. These therapies do not reverse damage but may slow further vision loss and, occasionally, improve some vision.
Similar Conditions Detected by Optometrists
Optometrists are trained to detect and distinguish AMD from other common retinal and ocular diseases, including:
- Diabetic retinopathy: Damage to the retinal blood vessels due to long-term diabetes.
- Retinal detachment: Separation of the retina from the underlying tissues, a medical emergency.
- Glaucoma: Gradual damage to the optic nerve, often associated with high eye pressure.
- Hypertensive retinopathy: Damage caused by chronic high blood pressure.
Routine eye exams are essential for distinguishing among these conditions and ensuring appropriate referral and timely intervention.
Other Eye Conditions Diagnosed in Routine Optometric Exams
Besides AMD, optometrists can diagnose and co-manage:
- Cataracts
- Dry eye syndrome
- Conjunctivitis (“pink eye”)
- Refractive errors (myopia, hyperopia, astigmatism, presbyopia)
Early detection of these conditions, as with AMD, can greatly improve outcomes and quality of life.
When Should You See an Ophthalmologist for Macular Degeneration?
While your optometrist is crucial for routine screening and initial detection, the following situations necessitate specialist attention:
- You have a confirmed diagnosis of macular degeneration, especially if vision problems are worsening quickly.
- Advanced imaging (OCT or angiography) or specialized treatment (such as injections) is recommended.
- There is evidence of a complication, such as leaking vessels (wet AMD) or vision-threatening progression.
Frequently Asked Questions (FAQs)
Can an optometrist make a definitive diagnosis of macular degeneration?
Yes, optometrists can detect signs and often make the initial diagnosis of AMD using examination techniques and imaging. However, advanced or unclear cases usually require confirmation and treatment planning by an ophthalmologist or retina specialist.
What is the difference between an optometrist and an ophthalmologist in managing AMD?
Optometrists specialize in primary eye care, screening, and early management. Ophthalmologists are medical doctors with advanced training who can provide the full range of diagnostic, medical, and surgical treatments for AMD and other complex eye conditions.
What are the first signs of macular degeneration?
Early symptoms may include slight blurring or distortion of central vision, trouble recognizing faces, shadowy or dark spots in the center of your vision, or trouble reading in low light. Regular exams are essential, as symptoms can be subtle in the beginning.
Are there steps I can take to reduce my risk of macular degeneration?
Yes. Avoid smoking, eat a diet rich in leafy greens, maintain a healthy weight and blood pressure, wear sunglasses to block UV light, and ensure you attend routine eye exams for early detection.
What happens after a diagnosis of AMD?
After diagnosis, your optometrist or ophthalmologist will discuss lifestyle changes, possible use of special supplements, and whether additional specialist treatment is needed. Ongoing monitoring is necessary, as macular degeneration can progress.
Key Takeaways
- Optometrists are often the first to detect macular degeneration during routine eye exams, using advanced imaging and clinical evaluation.
- Definitive diagnosis and advanced management are provided by ophthalmologists or retina specialists, who can perform treatments such as anti-VEGF injections.
- Early detection and intervention are crucial in slowing vision loss and maintaining quality of life.
Summary Table: What Optometrists Can and Cannot Do in Macular Degeneration
| Action | Optometrist | Ophthalmologist/Retina Specialist |
|---|---|---|
| Routine screening | Yes | Yes |
| Initial diagnosis | Yes | Yes |
| Prescribe supplements/lifestyle guidance | Yes | Yes |
| Advanced diagnostics (OCT, fundus photo) | Often | Yes |
| Anti-VEGF injections | No | Yes |
| Surgical management | No | Yes |
| Monitor stable disease | Yes | Yes |
In conclusion, while optometrists are highly skilled at detecting and diagnosing macular degeneration in its early stages—with some offering detailed imaging and monitoring—referral to a specialist is essential for advanced management and treatment. Regular eye exams remain the cornerstone of preventing and mitigating vision loss associated with AMD.
References
- https://www.healthline.com/health/eye-health/can-an-optometrist-diagnose-macular-degeneration
- https://www.brightfocus.org/resource/the-eye-exam-for-macular-degeneration/
- https://spectrumeyecarenc.com/do-optometrists-treat-age-related-macular-degeneration/
- https://www.macularsociety.org/diagnosis-treatment/how/
- https://www.medicalnewstoday.com/articles/can-an-optometrist-diagnose-macular-degeneration
- https://www.macular.org/about-macular-degeneration/what-is-macular-degeneration/finding-a-doctor/what-kind-of-doctor-do-i-need-to-see
- https://brighteyesny.com/blog/how-an-optometrist-diagnoses-and-treats-macular-degeneration/
- https://myoptometristcalgary.ca/blog/How+Does+An+Eye+Doctor+Diagnose+Macular+Degeneration/84
Read full bio of Sneha Tete












