Can Diabetic Neuropathy Be Reversed? Understanding Options and Limitations
Discover the realities of diabetic neuropathy: causes, treatment strategies, and tips to slow progression and improve quality of life.
Can Diabetic Neuropathy Be Reversed?
Diabetic neuropathy is a common complication of diabetes that leads to nerve damage, pain, and various other symptoms, particularly in the limbs. Many people with diabetes wonder if this complication can be reversed, or, at the very least, what measures can be taken to stop its progression and lessen its effects.
This comprehensive guide addresses whether diabetic neuropathy is reversible, explains why reversal is challenging, reviews the effects of neuropathy, and offers practical tips for management and prevention of further nerve damage.
Is It Possible to Reverse Diabetic Neuropathy?
Current evidence and clinical consensus are clear: nerve damage from diabetes cannot be reversed. The body does not have the ability to naturally repair or regrow damaged nerve tissue caused by diabetic neuropathy .
- While you cannot undo existing nerve damage, it is possible to stop neuropathy from worsening with early and aggressive management.
- With optimal care and blood sugar control, some symptoms may improve or even disappear, which may feel like reversal—but underlying nerve damage remains.
- Early intervention is critical. Sometimes, very mild neuropathy can be halted or symptoms lessened significantly if addressed promptly.
Why Isn’t Diabetic Neuropathy Reversible?
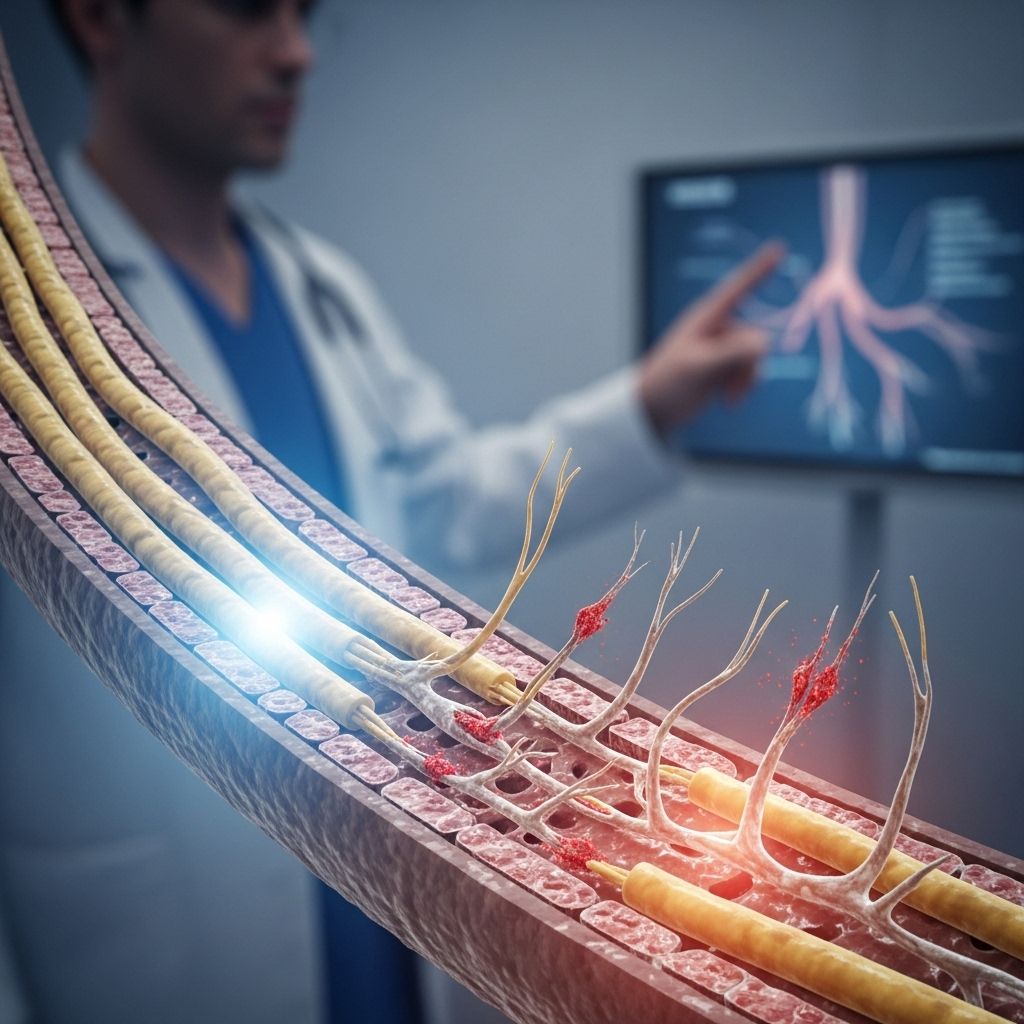
Diabetic neuropathy refers to damage affecting the peripheral nerves (responsible for sensation and movement) and sometimes the autonomic nerves (which control involuntary bodily functions). The primary causes of this damage include:
- Chronic high blood sugar (hyperglycemia) – This is the major risk factor, leading to inflammation and impaired blood flow to nerves.
- High blood fats (triglycerides) – Can injure nerve fibers and cells.
- Oxidative stress and inflammation – Harm nerves and their supporting tissues.
- Once nerve cells and fibers are lost, the body’s nerve regeneration capacity is very limited in adults.
Because the underlying biology of nerve repair is so constrained, modern medicine focuses on slowing progression and managing symptoms.
Types and Effects of Diabetic Neuropathy
More than half of people with diabetes experience some form of neuropathy during their lives. The four main types are:
- Peripheral neuropathy – Affects the legs, feet, hands, and arms; symptoms include pain, tingling, numbness, and, in severe cases, weakness.
- Autonomic neuropathy – Impacts nerves controlling internal organs, resulting in digestion, bladder, sexual, or heart rate problems.
- Proximal neuropathy – Sudden pain and weakness in the hip, thigh, or buttock, often on one side, also called diabetic amyotrophy.
- Focal neuropathy – Affects isolated nerves, often causing sudden muscle weakness or pain, such as in carpal tunnel syndrome or eye muscles.
Symptoms and consequences may include:
- Pain, burning, tingling, or numbness (often in the feet or hands)
- Reduced ability to feel temperature and pain, raising risk of infections and injuries
- Muscle weakness, balance problems, and slow wound healing (leading to foot ulcers)
- Digestive issues, bladder issues, blood pressure irregularities, and sexual dysfunction
Table: Types of Diabetic Neuropathy and Their Common Symptoms
| Type | Major Symptoms | Primary Affected Area |
|---|---|---|
| Peripheral | Pain, tingling, numbness, weakness | Feet, legs, hands, arms |
| Autonomic | Digestive, urinary, sexual, cardiac issues | Internal organs |
| Proximal | Severe pain, weakness, atrophy | Hips, thighs, buttocks |
| Focal | Sudden localized weakness or pain | Individual nerves (hands, head, torso) |
Managing Diabetic Neuropathy: Strategies to Slow Progression
Though cure is not currently possible, effective management can reduce symptoms, prevent further damage, and improve quality of life. These strategies are strongly recommended:
Blood Sugar Control
- Maintaining optimal blood glucose levels is the cornerstone of managing neuropathy.
- Stable blood sugars prevent new nerve injury and can sometimes reduce the severity of symptoms.
Managing Other Risk Factors
- Keep blood pressure in check (target usually <140/90 mmHg; your doctor may recommend lower)
- Manage cholesterol and triglycerides
- Avoid or quit smoking (which worsens circulation to nerves)
Medications and Symptom Relief
- Pain from neuropathy is often managed with antidepressants, anticonvulsants, or topical treatments (such as capsaicin cream or lidocaine patches).
- Pain relievers (acetaminophen, NSAIDs) may help, but stronger medications should be monitored closely by a healthcare provider.
- Emerging research is investigating nerve growth factor therapies, antioxidants, and gene therapy, but these are still under development.
Lifestyle and Complementary Therapies
- Regular exercise supports healthy blood flow, helps control blood sugar, and strengthens muscles.
- A balanced diet rich in B vitamins, antioxidants, and healthy fats may support nerve health (but supplements should only be used as advised by a doctor).
- Physical therapy helps maintain strength, mobility, and balance.
- In some cases, acupuncture or massage can provide additional symptom relief.
Foot Care and Injury Prevention
- Daily foot inspections for cuts, blisters, redness, or swelling are crucial.
- Wear well-fitted, cushioned shoes, and avoid barefoot walking to reduce injury risk.
- Seek medical attention promptly for ulcers, sores, or signs of infection.
Latest Research and Emerging Treatments
The medical community continues to research interventions that may eventually aide nerve regeneration or symptom reversal in diabetic neuropathy:
- Alpha-lipoic acid and acetyl-L-carnitine have shown potential in improving symptoms in some small studies.They’re generally considered as adjuncts, not standalone treatments.
- Stem cell and gene therapy approaches are being investigated but are not yet clinically available for routine neuropathy treatment.
- The concept of treating with vascular endothelial growth factor (VEGF) to improve blood flow to nerves is being studied, though results are preliminary .
At this time, these options should be considered experimental and are not recommended without medical supervision.
Practical Tips for Living With Diabetic Neuropathy
- Keep regular appointments with your diabetes care team.
- Report new or worsening symptoms as soon as possible—early intervention matters.
- Monitor your blood sugars at home and aim to keep them in your target range most of the time.
- Prioritize safe physical activity and healthy eating, and avoid alcohol or substances that can worsen nerve damage.
- Consider working with a podiatrist for specialized foot care.
Frequently Asked Questions (FAQs)
Can diabetic neuropathy ever be reversed?
No, current medical evidence shows that once nerves are damaged by diabetes, they cannot be completely repaired or regrown.
Why do some people say their symptoms improved or went away?
With proper management, it is sometimes possible to reduce or eliminate symptoms. However, this does not mean the underlying nerve damage is gone—it is simply well-controlled or compensated for.
How can I prevent diabetic neuropathy from worsening?
- Maintain excellent blood sugar control
- Manage blood pressure and cholesterol
- Avoid smoking and limit alcohol use
- Get regular exercise suited to your abilities
- Perform daily foot checks and skin care
Are there any supplements that work for diabetic neuropathy?
Some supplements like alpha-lipoic acid and B vitamins have been studied, but results are mixed and should only be used under medical guidance. There is no supplement proven to reverse diabetic neuropathy.
Will future research offer a cure for diabetic neuropathy?
Ongoing research continues in gene therapy, stem cell treatments, and nerve growth factors. These may improve outcomes in the future but are not yet established therapies.
When to Seek Help
- Sudden pain, weakness, or numbness that worsens quickly
- Non-healing wounds, infection, or ulcers, especially on the feet or legs
- Severe symptoms interfering with daily life, mobility, or independence
Early consultation with your healthcare provider increases the chance of controlling neuropathy and preventing further complications.
Takeaway
Although diabetic neuropathy cannot currently be reversed, timely action can greatly improve symptoms, halt progression, and enhance quality of life. Stay engaged with your healthcare team, commit to self-care strategies, and watch for updates in medical research as new treatments emerge.
References
- https://www.johnstonmd.com/blog/diabetic-neuropathy-can-it-be-reversed
- https://www.capitalfeet.com/post/can-diabetic-neuropathy-be-reversed
- https://www.healthline.com/health/diabetes/can-diabetic-neuropathy-be-reversed
- https://www.medicalnewstoday.com/articles/317923
- https://pmc.ncbi.nlm.nih.gov/articles/PMC209306/
- https://my.clevelandclinic.org/health/diseases/21621-diabetic-neuropathy
- https://www.mayoclinic.org/diseases-conditions/diabetic-neuropathy/diagnosis-treatment/drc-20371587
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9643187/
- https://my.clevelandclinic.org/health/diseases/14737-peripheral-neuropathy
- https://www.nature.com/articles/s41392-025-02175-1
Read full bio of medha deb












