Can Diabetic Macular Edema Be Cured? Understanding DME, Treatments, and Outlook
Explore the causes, treatment options, and potential outcomes for diabetic macular edema—a common complication of diabetes that can threaten vision.
Can Diabetic Macular Edema Be Cured?
Diabetic macular edema (DME) is a complication of diabetes that threatens vision and quality of life. While considerable progress has been made in treatment, understanding whether DME can be cured depends on multiple factors, including how early it is detected and the response to therapy. In this article, we explore the underlying causes, available treatments, expectations, and advice for living with this condition.
What Is Diabetic Macular Edema?
Diabetic macular edema (DME) is a swelling of the macula—the central part of the retina responsible for sharp, straight-ahead vision—caused by fluid leaking from damaged blood vessels in the retina. DME is the most common cause of vision loss in people with diabetic retinopathy and affects millions of individuals globally, rising in number alongside diabetes cases.1
- The macula: Area responsible for central, high-resolution vision, needed for reading and recognizing faces.
- Edema: Refers to swelling caused by the accumulation of fluid.
DME arises as a consequence of chronically high blood sugar, which damages the small blood vessels supplying the retina. The result is leakage of fluid and proteins into the macula, leading to visual disturbances.
Prevalence and Impact
- Estimated to affect up to 37 million people worldwide—numbers expected to grow with rising diabetes prevalence.
- Increases risk of visual impairment or blindness, especially in working-age adults.
- May progress gradually or be detected during a routine eye exam before symptoms appear.
Symptoms of Diabetic Macular Edema
Symptoms can vary from subtle to severe, and some individuals may remain asymptomatic in the early stages. Recognizing symptoms early is important for prompt intervention.
- Blurred or wavy central vision
- Difficulty reading or seeing fine details
- Washed-out colors or colors appearing dull
- Distorted vision (straight lines may look bent)
- Dark spots or empty areas in the center of vision
- Double vision (in some cases)
Note: Symptoms may affect one or both eyes. Because the changes can be slow and subtle, regular eye exams are essential for early identification and intervention.
What Causes Diabetic Macular Edema?
DME develops due to a breakdown of the blood-retinal barrier, primarily triggered by long-term uncontrolled or poorly controlled diabetes. The process involves several stages:
- High blood sugar damages the small blood vessels of the retina, resulting in diabetic retinopathy.
- Damaged, weakened blood vessels leak fluid and protein into the macula.
- Build-up of this fluid causes the macula to swell, distorting vision.
Key triggers that increase the risk or severity of DME include:
- Poorly controlled blood glucose over time
- Longstanding diabetes (type 1 or type 2)
- High blood pressure and cholesterol
- Diabetic kidney disease
- Previous cases of diabetic retinopathy
- Smoking
In rare cases, macular edema may also be triggered or worsened by other medical conditions, certain medications, eye surgery, or local inflammation, but diabetes remains the predominant cause.
Risk Factors and Who Is at Risk?
- People with type 1 or type 2 diabetes
- Longer duration of diabetes (higher cumulative risk over time)
- Inadequate control of blood sugar, blood pressure, or cholesterol
- Diabetic retinopathy (especially proliferative types)
- Coexisting kidney disease or other vascular complications
Regular monitoring and diabetes management are crucial to reducing the risk of developing DME or halting its progression.
Diagnosing Diabetic Macular Edema
DME is not always evident without a professional eye examination. The following tests are commonly used by ophthalmologists or retina specialists:
- Comprehensive dilated eye exam: Allows for direct view of the retina and macula using slit lamp and ophthalmoscopy.
- Optical coherence tomography (OCT): Uses light waves to produce cross-sectional images of the retina, revealing fluid accumulation and thickness changes.
- Fluorescein angiography: A dye test used to visualize leaking or abnormal retinal blood vessels.
These diagnostic techniques enable early detection and precise measurement of fluid build-up, both critical for guiding treatment strategies and monitoring response.
Current Treatment Options for DME
Managing DME generally aims to reduce fluid in the macula, stop further vision loss, and in some cases, restore vision. While a permanent cure remains elusive for most, modern therapies often achieve significant and lasting improvements if treatment is started early.
Key treatment approaches include:
1. Anti-VEGF Medications
Anti-vascular endothelial growth factor (anti-VEGF) therapy has become the standard of care for center-involving DME. These injections target VEGF, a protein that promotes abnormal vessel growth and leakage in the retina.
- Delivered through regular injections (initially monthly, then as needed) into the affected eye
- Help stop leakage, reduce swelling, and stabilize or improve vision
- Brands include ranibizumab, aflibercept, bevacizumab, and faricimab (a bispecific antibody targeting both VEGF and Ang-2)
- Most patients need repeat injections—sometimes indefinitely or for several years
2. Corticosteroids
Steroids help reduce inflammation and vascular leakage. Useful for patients who do not tolerate anti-VEGF therapy or as an add-on.
- Available as eye injections or as slow-release implants
- Benefits can last months before a repeat dose is necessary
- Risks may include increased intraocular pressure (glaucoma risk) and cataract development
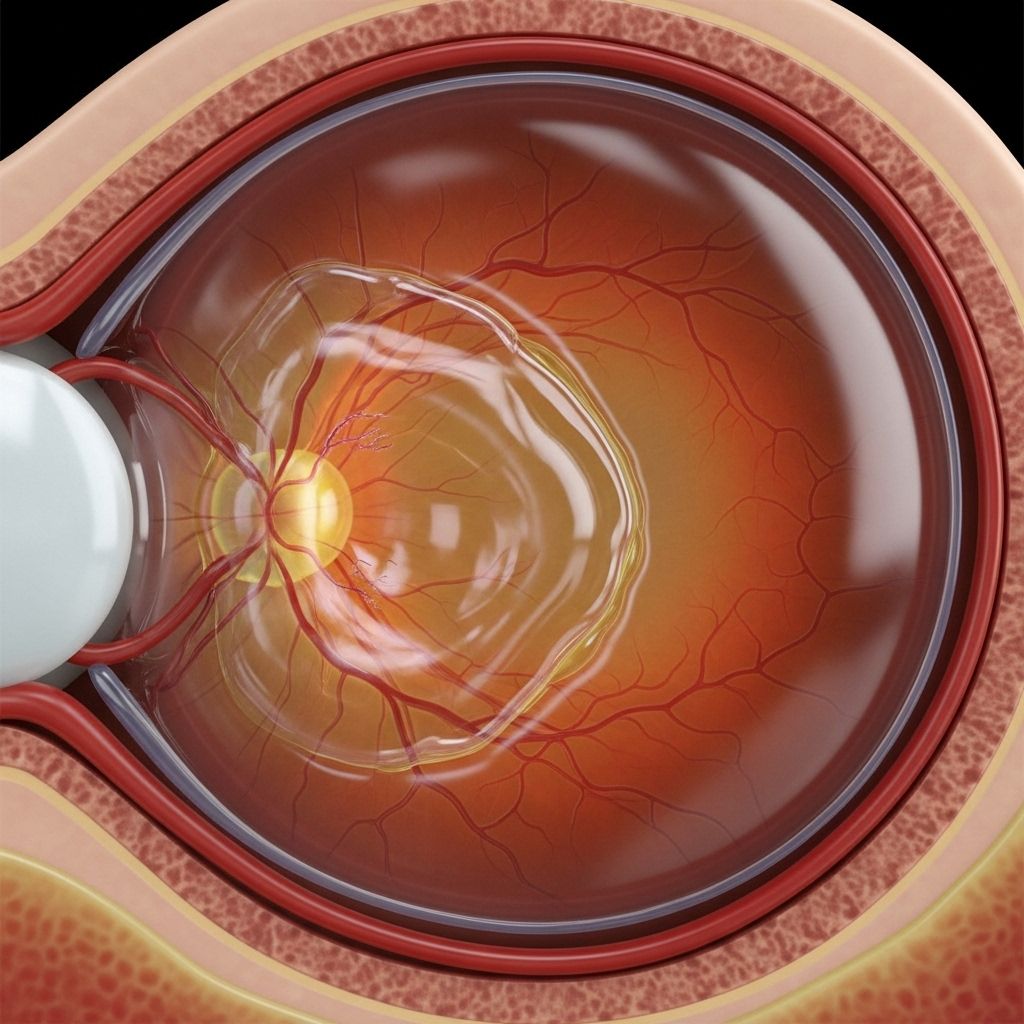
3. Laser Photocoagulation
Laser therapy uses focused light to seal off leaking blood vessels, reducing further fluid accumulation.
- Less commonly used as a first-line therapy for center-involving DME, but may be useful for specific cases (especially non-center DME)
- Procedure is typically painless and can be performed in-office
- Can prevent worsening vision loss, though may leave permanent blind spots where applied
4. Upcoming and Experimental Therapies
- Novel implantable devices delivering longer-acting medications
- Bi-specific antibodies (targeting multiple pathways at once)
- Non-invasive therapies, such as investigational eye drops (e.g., high concentration dexamethasone drops in clinical trials)2
5. Low Vision Aids and Rehabilitation
For those with persistent visual deficits, various assistive devices and vision rehabilitation programs can help maximize independence:
- Magnifying glasses, digital magnifiers, and large-print materials
- Electronic devices that assist reading or daily tasks
- Vision rehabilitation therapy to adapt to limited central vision
Can Diabetic Macular Edema Be Cured?
The ultimate question—is there a cure? The answer is nuanced:
- For most people, DME is a chronic condition—with the right treatment, swelling can be controlled and vision loss slowed or sometimes partially reversed.
- If caught early and treated aggressively, it may be possible to restore much or all of the lost vision. However, relapses can occur and ongoing monitoring is required.
- For a minority of people, the condition may become stable off treatment, but this is not the norm.
- A complete permanent cure—meaning no chance of recurrence—is rare. Ongoing follow-up is necessary to manage future risks.
Some newer medications and emerging therapies have shown promise to improve outcomes and even reverse some of the existing damage, but maintaining diabetic control remains vital to prevent recurrence.
Preventing and Managing Diabetic Macular Edema
While direct cures are not yet standard, there is much you can do to prevent DME or minimize its severity:
- Maintain optimal blood sugar control—a cornerstone of lowering risk
- Control blood pressure and cholesterol with a healthy lifestyle and, if necessary, medications
- Quit smoking to reduce vascular damage risk
- Attend regular diabetes and eye check-ups to catch problems early
- Follow your eye doctor’s advice closely on both monitoring and treatment plans
Living Well with DME
A diagnosis of DME means more than just medical management. It also requires emotional resilience and adaptation. Most people can live independently and remain active with the right supports:
- Low vision aids and assistive devices
- Connecting with a low vision specialist for tailored advice
- Participating in vision rehabilitation to learn new skills
- Seeking support groups to share strategies and experiences
Staying healthy with diabetes, maintaining close communication with your healthcare team, and getting the right eye care can result in many years of good quality life—even with DME.
Frequently Asked Questions (FAQs) about Diabetic Macular Edema
Q: Can diabetic macular edema go away on its own?
A: In most cases, DME does not resolve spontaneously and typically worsens without treatment. Medical intervention is usually required to prevent permanent vision damage.
Q: How effective are current treatments for DME?
A: Many people respond well to modern therapies—especially anti-VEGF injections—but frequent follow-up and ongoing treatment may be required. Some individuals can regain lost vision; others stabilize but may not recover full clarity.
Q: Is there a way to prevent DME if I have diabetes?
A: Yes. Effective management of blood sugar, blood pressure, and cholesterol dramatically reduces risk. Annual dilated eye exams are essential for early detection.
Q: If I have vision loss from DME, can I drive or work?
A: Many people with DME continue to drive and work, especially with early treatment and/or vision aids. Your eye doctor will advise on safety and legal standards for driving.
Q: Are there new treatments on the horizon?
A: Yes—there are promising new drugs, implantable devices, and even non-invasive therapies like special eye drops in development. Speak with your eye specialist regarding eligibility for clinical trials or new options if current therapies are not effective.
Resources and Support
- American Diabetes Association: Offers support, resources, and education for those living with diabetes.
- Prevent Blindness: Information and advocacy on diabetes-related eye health.
- Low Vision Centers: Local organizations provide rehabilitation and technology for people with vision loss.
Key Takeaways
- With prompt, ongoing, and comprehensive care, most people with DME can avoid severe, permanent vision loss.
- While a true “cure” is rare, modern therapies offer substantial hope for vision preservation and recovery.
- Prevention, regular screening, and diabetes management remain the most effective strategies.
- If vision loss occurs, low vision aids and support services can help maintain quality of life.
References
- https://www.retinaconsultantstexas.com/blog/spotlight-on-macular-edema-causes-symptoms-and-treatment-options
- https://oculis.com/our-areas-of-focus/diabetic-macular-edema/
- https://my.clevelandclinic.org/health/diseases/24733-diabetes-related-macular-edema
- https://preventblindness.org/diabetic-macular-edema-dme/
- https://www.retinany.com/services/diabetic-macular-edema
- https://www.macularsociety.org/macular-disease/macular-conditions/diabetic-macular-oedema/
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/multimedia/diabetic-macular-edema/img-20124558
- https://www.mdfoundation.com.au/about-macular-disease/diabetic-eye-disease/about-diabetic-macular-oedema/
Read full bio of Sneha Tete












