Can Diabetes Cause Blindness? Understanding Risks and Prevention
Discover how diabetes affects your eyesight, the mechanisms behind diabetic blindness, key warning signs, prevention, and treatment strategies.
Can Diabetes Cause Blindness?
Diabetes is a chronic condition that impacts millions of people worldwide and carries the risk of severe complications. Chief among those complications is the potential to cause permanent vision loss or blindness. But how exactly does diabetes affect eye health, who is at risk, how can you spot symptoms early, and what are your options for treatment and prevention? This article provides an in-depth look at how diabetes can lead to blindness and how you can protect your vision.
How Diabetes Can Cause Blindness
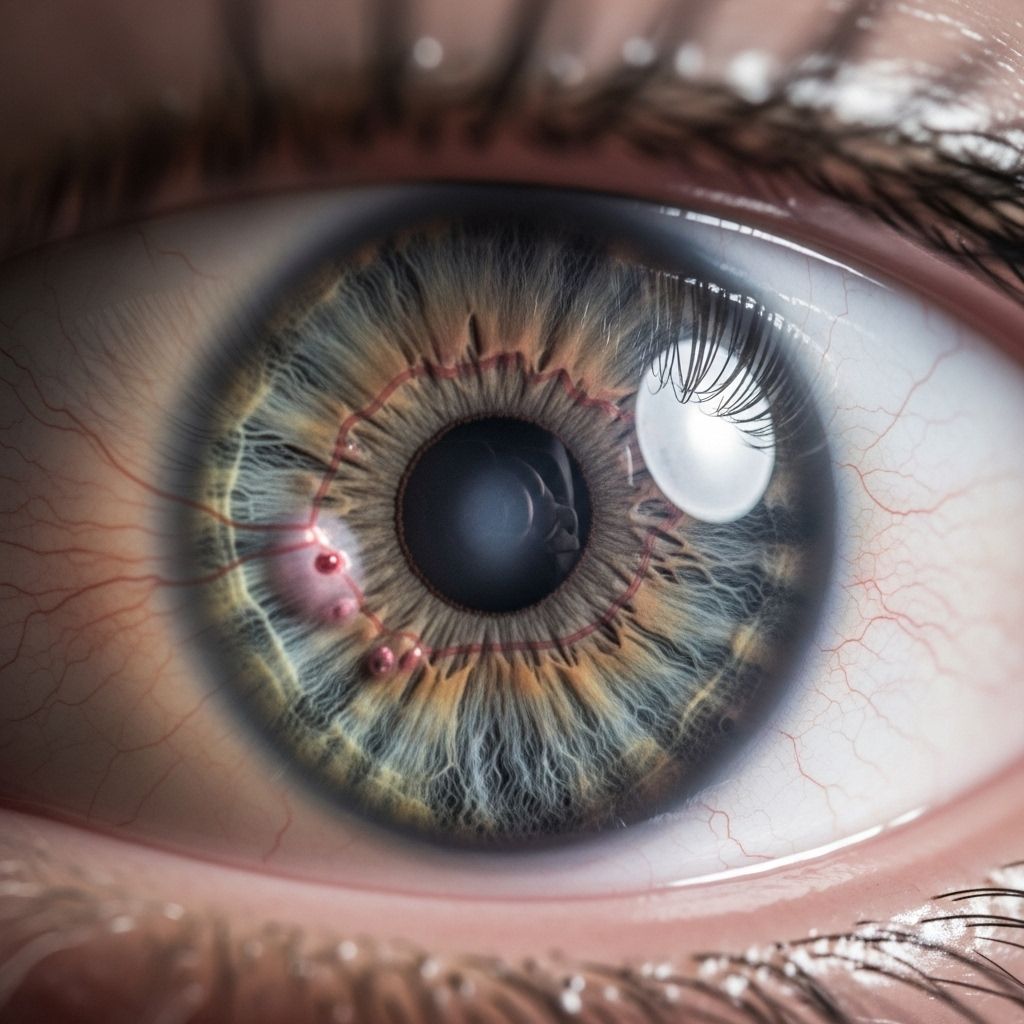
Diabetes primarily threatens vision through its impact on the blood vessels within the eye, especially the retina. Elevated blood glucose levels over time damage small blood vessels, leading to a condition called diabetic retinopathy. Without timely intervention, diabetic retinopathy can progress to irreversible blindness.
- What is the retina? It is a light-sensitive layer at the back of your eye that is crucial for vision.
- How does diabetes harm the retina? Prolonged high blood sugar damages the tiny blood vessels supplying the retina, leading to leakage, swelling, or new abnormal vessel growth, all of which impair vision.
- The most serious forms of vision loss from diabetes include diabetic retinopathy, but diabetes also increases the risk for cataracts and glaucoma.
Understanding Diabetic Retinopathy
Diabetic retinopathy is the leading cause of vision impairment in adults with diabetes. It is estimated that about one-third of people living with diabetes have some degree of retinopathy, and one in ten may eventually develop vision-threatening disease.
Stages of Diabetic Retinopathy
| Stage | Description | Potential Vision Impact |
|---|---|---|
| Non-Proliferative DR (NPDR) | Early stage. Blood vessels in the retina weaken, bulge (microaneurysms), and may leak fluid causing swelling (edema), especially in the macula. | May cause blurred vision if edema develops, but often has no symptoms initially. |
| Proliferative DR (PDR) | Advanced stage. Poorly nourished retina causes new, fragile blood vessels to grow. These vessels are prone to bleeding, leading to scarring or retinal detachment. | Dark spots, severe vision loss, or even total blindness if untreated. |
Other Diabetes-Related Eye Diseases
- Diabetic Macular Edema (DME): Swelling of the macula due to fluid leakage, leading to vision distortion and is a major cause of blindness in diabetes.
- Cataracts: Diabetes increases the risk of developing cataracts (clouding of the eye’s lens) and getting them at a younger age.
- Open-Angle Glaucoma: Diabetes nearly doubles the risk for this slow-progressing eye disease that damages the optic nerve.
Who Is at Risk?
Anyone with type 1, type 2, or gestational diabetes is at risk for diabetic retinopathy and other diabetic eye diseases. Important risk factors include:
- Duration of diabetes – the longer you have diabetes, the higher your risk.
- Consistently high blood sugar levels.
- High blood pressure or high cholesterol.
- Pregnancy (in people with pre-existing or gestational diabetes).
- Smoking.
- Belonging to certain ethnic/racial groups, including African American, Hispanic/Latino, or Native American ancestry.
Symptoms and Warning Signs
Early diabetic retinopathy often develops without noticeable symptoms. Regular screening is thus critical. As the disease progresses, symptoms may include:
- Blurry or fluctuating vision.
- Spots or dark shapes (floaters) in your field of view.
- Difficulty seeing at night or in low light.
- Colors appearing faded or washed out.
- Dark or empty spots in the center of your vision.
- Sudden vision loss (seek urgent care).
Many cases are not identified until significant damage has occurred, making regular eye exams essential for all people with diabetes, even when vision is normal.
How Is Diabetic Eye Disease Diagnosed?
Diagnosis relies on comprehensive, dilated eye exams performed by an optometrist or ophthalmologist:
- Your doctor will use eye drops to dilate (widen) your pupils and examine the retina for any signs of leakage, swelling, or abnormal vessels.
- Other tests, such as optical coherence tomography (OCT) or fluorescein angiography, may be used for detailed retinal imaging and assessing blood vessel function.
- Early and regular screening are crucial: Type 2 diabetes patients should get an exam at diagnosis; type 1 diabetes, within five years of initial diagnosis. Pregnant women with diabetes need an eye exam early in pregnancy.
How Quickly Can Diabetes Cause Blindness?
Vision loss due to diabetes generally unfolds over years, not days or weeks. The speed at which blindness might develop depends on how well diabetes is controlled and whether early eye changes are detected and treated:
- Without treatment or good blood sugar control, retinopathy can progress from early stages to severe vision loss within a decade.
- Some aggressive forms (especially with poor control or additional risk factors) can cause significant vision impairment more rapidly.
- Most major causes of blindness from diabetes are preventable or treatable with regular eye exams and prompt intervention.
Treatment Options for Diabetic Eye Disease
Multiple treatments can effectively manage diabetic eye complications and help prevent progression to blindness. Options include:
- Laser Therapy (Photocoagulation): Targets leaking vessels, slows or stops bleeding, and helps prevent vision loss.
- Medication Injections: Drugs like VEGF inhibitors or corticosteroids are injected into the eye to reduce swelling and block abnormal blood vessel growth.
- Vitrectomy Surgery: Surgically removes blood-filled or scarred gel from the eye, especially in advanced cases.
- Cataract or Glaucoma Surgeries: Address other diabetes-related eye complications when necessary.
Early treatment at the first signs of disease is essential for the best outcomes.
Prevention: Protecting Your Sight When You Have Diabetes
- Control Blood Sugar: The lower and more stable your A1c (average blood sugar), the lower your risk of retinopathy and other complications.
- Manage Blood Pressure and Cholesterol: High blood pressure and cholesterol further damage blood vessels in the eye.
- Regular Comprehensive Eye Exams: Annual dilated eye exams (or more often if recommended) for all people with diabetes.
- Quit Smoking: Smoking compounds blood vessel damage and increases risk.
- Follow Your Diabetes Care Team’s Advice: Take medication as prescribed, maintain a balanced diet, exercise, and attend regular check-ups.
Adhering to preventive care significantly reduces the likelihood of irreversible vision loss.
Frequently Asked Questions (FAQs)
Can everyone with diabetes go blind?
Not everyone with diabetes will go blind. With proper management and regular eye exams, most cases of blindness due to diabetic retinopathy are preventable.
What are the first warning signs of diabetic eye disease?
Early diabetic retinopathy may show no symptoms. Warning signs as the disease advances include blurred or fluctuating vision, spots, and dark areas in your sight. Regular screening is vital for early detection.
How often should I get my eyes checked if I have diabetes?
At least once a year, but more frequently if your doctor recommends. If you notice sudden vision changes, contact your eye doctor immediately.
Can lost vision from diabetic retinopathy be restored?
Treatment can stabilize or even improve vision in some cases, especially if started early. However, advanced disease with severe damage may lead to permanent vision loss.
Does good blood sugar control eliminate all risk?
Good control dramatically reduces your risk and slows disease progression, but it does not eliminate risk entirely. Annual eye exams are still needed.
Summary Table: Key Facts About Diabetes and Blindness
| Fact | Details |
|---|---|
| Most common eye disease in diabetes | Diabetic retinopathy |
| Prevention | Blood sugar, blood pressure control, annual eye exams |
| Major treatable symptoms | Blurred vision, floaters, sudden vision changes |
| Treatments | Laser therapy, injections, surgery |
| Vision loss risk | Rises with longer diabetes duration and poor disease control |
Takeaway
Diabetes significantly increases the risk of vision loss and blindness, but most severe outcomes can be prevented with early detection, regular comprehensive eye exams, and consistent management of blood glucose, blood pressure, and cholesterol. Alert your eye care professional to any vision changes, and follow up on recommended screenings. Taking these steps empowers you to protect your eyesight and quality of life.
References
- https://www.orbis.org/en/avoidable-blindness/diabetic-retinopathy
- https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-vision-loss.html
- https://www.upmc.com/services/eye/conditions/diabetic-retinopathy
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://www.nhs.uk/conditions/diabetic-retinopathy/
- https://medlineplus.gov/diabeticeyeproblems.html
- https://www.nm.org/healthbeat/healthy-tips/diabetes-and-blindness
Read full bio of Sneha Tete












