Understanding C3G and IgAN: Medical Terminology for Kidney Disease
Get a comprehensive overview of the terminology and key concepts behind C3G and IgA nephropathy kidney diseases.
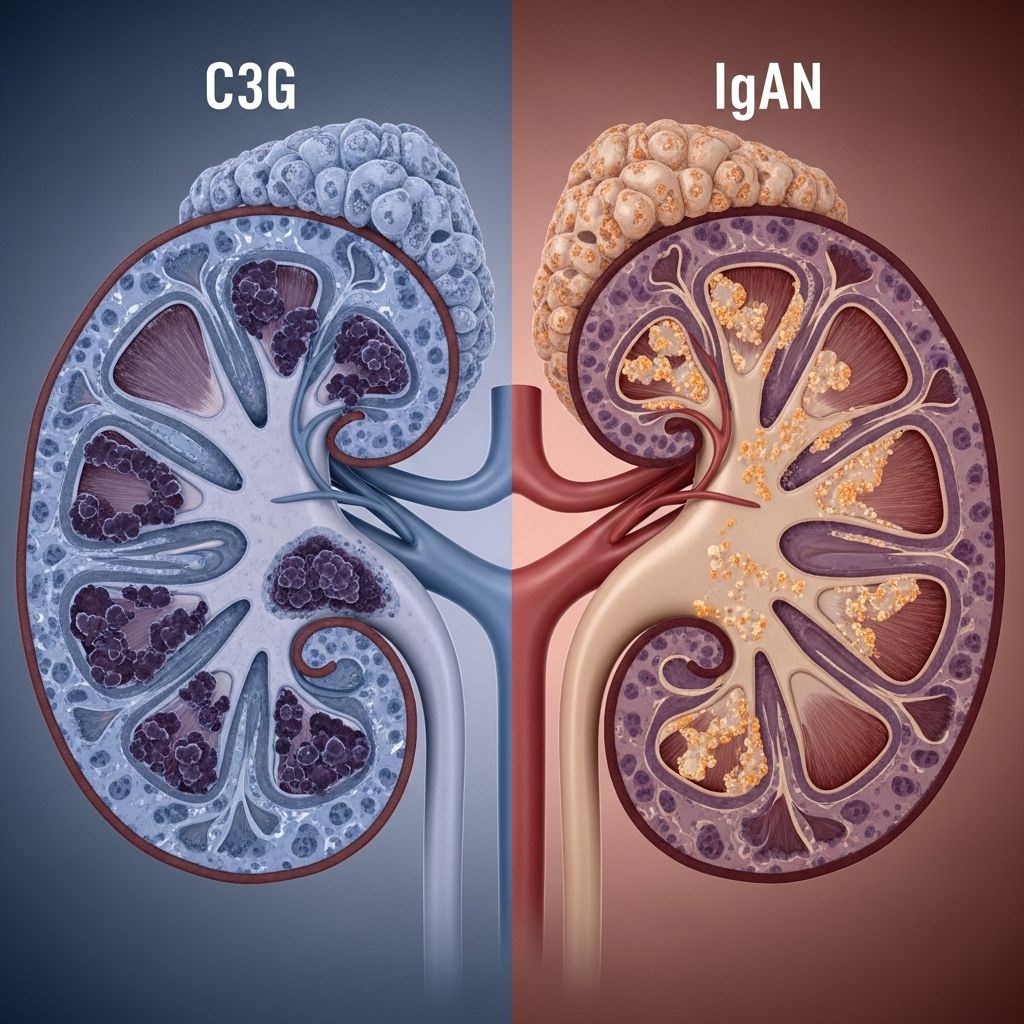
Kidney health is critical for the maintenance of your body’s internal balance, as your kidneys filter waste and excess fluids from your blood, regulate blood pressure, and ensure proper mineral balance. Two lesser-known but significant kidney conditions are C3 glomerulopathy (C3G) and IgA nephropathy (IgAN). Both are types of glomerulonephritis, a group of diseases that injure the glomeruli (the filtering units of the kidneys), and each has specific medical terminology essential for understanding diagnosis and treatment. This article explores the core terms, pathology, diagnosis, and key aspects of these complex kidney conditions.
Table of Contents
- About Glomerulonephritis
- What is C3G?
- What is IgA Nephropathy?
- Important Medical Terms in Kidney Disease
- Diagnosis Process for C3G and IgAN
- Common Laboratory and Pathology Terms
- Treatment and Management of C3G and IgAN
- Living with C3G and IgAN
- Glossary of Kidney Disease Terminology
- Frequently Asked Questions (FAQs)
About Glomerulonephritis
Glomerulonephritis refers to inflammation of the glomeruli, the tiny filters in the kidney that remove waste and excess fluid. There are several subtypes of glomerulonephritis, including C3G and IgAN, each with distinct features:
- C3G (C3 glomerulopathy): Characterized by abnormal deposits of complement protein C3 in the glomeruli, resulting from malfunction in the complement pathway, part of the immune system.
- IgA Nephropathy (IgAN): Marked by the buildup of the IgA antibody in the kidneys, leading to inflammation and damage.
Both conditions can lead to chronic kidney disease (CKD), a progressive loss of kidney function.
What is C3G?
C3 glomerulopathy (C3G) is a rare kidney disorder characterized by predominant C3 complement protein deposits in the kidney, often resulting in proteinuria (protein in urine), hematuria (blood in urine), and long-term loss of kidney function.
- Related to genetic or acquired problems in the complement system, a part of the immune system.
- Two main subtypes:
- Dense Deposit Disease (DDD): Named for the dense ribbon-like deposits seen on electron microscopy.
- C3 glomerulonephritis (C3GN): Shows C3-dominant staining on immunofluorescence, but with less ultra-structural density than DDD.
- C3G may present in childhood or adulthood, with variable disease severity.
C3G is diagnosed via kidney biopsy with special staining and microscopy techniques.
What is IgA Nephropathy?
IgA Nephropathy (IgAN), also known as Berger’s disease, is the most common glomerulonephritis worldwide. It occurs when IgA, an antibody, builds up in the glomeruli, causing inflammation.
- Often discovered following visible blood in the urine (hematuria), typically after an upper respiratory tract infection.
- Disease progression is slow and variable; some maintain normal kidney function, while others may develop CKD over time.
- Diagnosis is confirmed by kidney biopsy and immunofluorescence showing IgA-dominant deposits.
The cause of abnormal IgA accumulation is not fully understood, but genetic, environmental, and immune factors are all implicated.
Important Medical Terms in Kidney Disease
Understanding kidney disease involves numerous specialized terms. Here are some key terms essential for C3G, IgAN, and glomerular diseases in general:
| Term | Definition |
|---|---|
| Proteinuria | Excess protein in the urine, an indicator of kidney filtration problems. |
| Hematuria | Blood in the urine, ranging from microscopic (not visible) to gross (visible). |
| eGFR | Estimated glomerular filtration rate, a measure of kidney function. |
| Creatinine | Waste product measured in blood to assess kidney function. |
| Complement System | Part of the immune system involved in inflammation and defense against infections; abnormalities can contribute to C3G. |
| Immunofluorescence | Microscopy technique used to detect immune deposits in kidney tissue. |
| Electron Microscopy | Advanced microscopy used to identify ultrastructural features of kidney disease. |
| Biopsy | The removal of a small kidney sample for detailed pathological examination. |
| Nephrotic Syndrome | Clinical syndrome involving high levels of proteinuria, low blood albumin, high cholesterol, and swelling. |
| Nephritic Syndrome | Kidney syndrome involving hematuria, hypertension, mild proteinuria, and reduced kidney function. |
Diagnosis Process for C3G and IgAN
Diagnosing these disorders is a multi-step process that incorporates clinical findings, laboratory data, and specialized pathology evaluation. Steps include:
- Clinical presentation: Symptoms (e.g., swelling, blood in urine) are evaluated. A patient may experience edema (swelling), hypertension (high blood pressure), or fatigue. Some patients are asymptomatic and are only diagnosed via abnormal urine tests.
- Urinalysis: Lab testing of urine to check for protein, blood, and other abnormalities.
- Blood tests: eGFR, creatinine, and testing for complement proteins (C3, C4) and autoantibodies.
- Kidney biopsy: A sample is taken to be analyzed by light microscopy, immunofluorescence, and electron microscopy. This reveals the characteristic deposits and inflammation patterns.
- Genetic and immunological testing: Sometimes performed to identify inherited or autoimmune causes, especially in cases of C3G.
Combined, these results provide the basis for a diagnosis and help in planning treatment.
Common Laboratory and Pathology Terms
- Immunostaining: The use of antibodies to stain specific proteins in tissue samples, helping identify immune deposits (e.g., C3, IgA, IgG).
- Mesangial proliferation: An increase in the number of mesangial cells in the glomerulus, often seen in IgAN.
- Cellular crescents: Layers of cells forming outside the glomerulus, indicating severe injury.
- Sclerosis: Hardening (scarring) of the glomeruli, which may indicate chronic damage.
- Podocyte injury: Damage to specialized cells (podocytes) that help filter blood through the glomerulus.
Treatment and Management of C3G and IgAN
Treatment strategies for these kidney diseases are tailored to the underlying cause, disease progression, and severity. Common goals include reducing proteinuria, controlling blood pressure, and managing immune system activity.
General Treatment Principles
- Blood pressure control: Typically using angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs).
- Immunosuppression: Medications such as corticosteroids and other immunosuppressive agents are sometimes considered.
- Dietary changes: Sodium and protein restriction may be recommended to reduce strain on the kidneys.
- Diuretics: Used to manage swelling and high blood pressure.
- Statins: Prescribed to help lower cholesterol if indicated.
- Treatment of underlying infections: If an underlying cause is identified (e.g., a specific infection), targeted therapies may be used.
Advanced Therapies
- Plasma exchange: Sometimes used in rapidly progressive forms or when autoantibodies play a major role.
- Targeted complement inhibitors: Research and clinical trials are ongoing for medications that directly target the complement pathway in C3G.
Management of End-Stage Renal Disease (ESRD)
- Dialysis: Used when kidney function falls below critical levels. Can be hemodialysis or peritoneal dialysis.
- Kidney transplantation: The preferred solution for suitable candidates with ESRD. Disease recurrence can occur and must be monitored.
Living with C3G and IgAN
Chronic kidney diseases such as C3G and IgAN require ongoing care and vigilance. The following tips can help improve quality of life and outcomes:
- Have regular check-ups to monitor kidney function and urine tests.
- Take prescribed medications on schedule and follow up with your healthcare provider about any side effects.
- Manage blood pressure and cholesterol as advised.
- Adopt a kidney-friendly diet as recommended by your doctor or dietitian.
- Stay physically active within your capability.
- Communicate any new or worsening symptoms promptly to your healthcare provider.
Education, support from healthcare teams, and patient advocacy organizations can provide additional information and encouragement.
Glossary of Kidney Disease Terminology
- Antibody: Protein used by the immune system to identify and neutralize foreign objects.
- Autoimmune disease: A disease in which the immune system attacks healthy parts of the body.
- Biopsy: Removal and examination of tissue sample from the body.
- Chronic kidney disease (CKD): Progressive decline in kidney function over time.
- Immunosuppressant: Medication that weakens the immune system.
- Nephron: The basic structural and functional unit of the kidney.
- Remission: Disappearance of signs and symptoms of disease.
- Relapse: A return of disease activity after improvement.
Frequently Asked Questions (FAQs)
What is the difference between C3G and IgA nephropathy?
C3G is characterized by C3 protein deposits from complement pathway dysfunction, while IgA nephropathy involves IgA antibody deposition. Each has distinct causes and disease mechanisms.
What are the early warning signs of glomerular kidney disease?
Early signs include swelling (edema), blood in the urine (hematuria), and high blood pressure. Sometimes there are no noticeable symptoms at all.
Can C3G or IgAN be cured?
There is currently no definitive cure for either condition. Treatments aim to slow progression, control symptoms, and preserve kidney function. Kidney transplantation may be considered at advanced stages.
What are the main diagnostic tests for these diseases?
Tests include urine and blood tests, kidney biopsy with immunofluorescence and electron microscopy, and genetic or antibody studies as needed.
Are these conditions inherited?
Some cases, especially C3G, may have genetic factors involved, but not all cases are inherited. Family history can sometimes increase risk.
How often do I need follow-up visits for C3G or IgAN?
Follow-up schedules vary; typically every 3–6 months, or more often if the disease is active or progressing.
Key Takeaway
C3G and IgA nephropathy are complex but increasingly well-understood forms of glomerular kidney disease. Knowing the terminology, disease mechanisms, and diagnostic process is vital for anyone affected. Work closely with your healthcare team and seek trusted sources for the latest information and support.
References
- https://www.medicalnewstoday.com/articles/172179
- https://www.medicalnewstoday.com/articles/327300
- https://www.healthline.com/health/kidney-disease
- https://www.healthline.com/health/chronic-kidney-disease
- https://www.healthline.com/health/video/kidney-failure
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7417004/
- https://www.healthline.com/health/video/foods-to-avoid-with-kidney-disease
- https://medlineplus.gov/chronickidneydisease.html
- https://www.youtube.com/watch?v=XUnRopZmYJs
Read full bio of Sneha Tete












