Burr Holes: Procedure, Uses, Risks, and Recovery
Understand how burr holes are used in neurosurgery, including their purpose, procedure, risks and what to expect during recovery.
Burr Holes in Neurosurgery: An In-Depth Overview
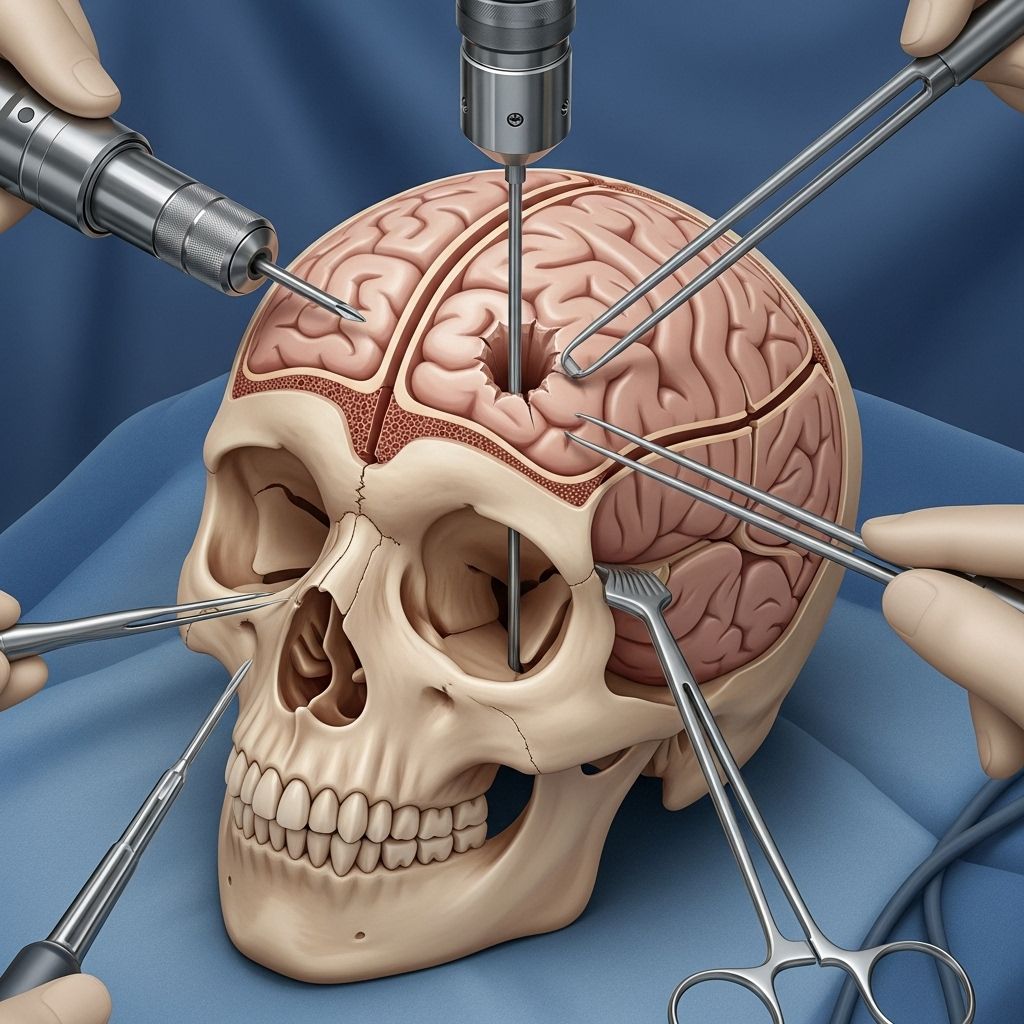
Burr holes are a fundamental procedure used in neurosurgery, involving the creation of small circular openings in the skull. This technique enables neurosurgeons to access the brain for various interventions, ranging from the treatment of acute trauma to the management of neurologic disorders like hydrocephalus. Understanding burr holes offers insight into why and how certain brain conditions are treated, the typical risks involved, and the details of post-operative recovery.
What Are Burr Holes?
A burr hole is a small, precisely drilled opening in the skull made using a specialized surgical tool called a burr. These holes allow direct access to the spaces inside the skull and can be used both diagnostically and therapeutically.
- Size: Typically 14–20 millimeters in diameter.
- Location: Most commonly placed at anatomical landmarks such as Kocher’s point, depending on the underlying need.
- Technique: Created with a surgical drill fitted with a perforator bit, sometimes extended and reconstructed using implants for specialized imaging.
Why Are Burr Holes Used?
Burr holes are used to treat several conditions related to the brain, and their indications range from lifesaving emergency procedures to routine, elective operations.
- Relieving pressure: For acute cases of intracranial bleeding or swelling.
- Draining blood or fluid: In conditions like subdural hematoma or chronic collections.
- Introducing medical devices: Placement of cerebrospinal fluid shunts or endoscopic instruments.
- Imaging access: As a window for postoperative ultrasound when standard CT and MRI imaging may not be optimal or feasible.
- Biopsy or evaluation: Collecting tissue samples or assessing intracranial pathology.
Common Conditions Treated with Burr Holes
- Hydrocephalus: A condition characterized by accumulation of cerebrospinal fluid (CSF) in the brain’s ventricles, often managed with ventriculoperitoneal (VP) shunt placement made accessible via burr holes.
- Chronic subdural hematoma: Slow bleeding between the brain surface and the dura, often relieved through drainage facilitated by burr holes.
- Brain abscess: Infection requiring direct intervention to drain the collection.
How Is a Burr Hole Procedure Performed?
The burr hole procedure combines planning, precision, and a sterile operating environment to ensure both effectiveness and safety.
- Performed under general anesthesia.
- The scalp is prepared and incised to expose the underlying bone.
- A surgical drill with a special perforator is used to make a circular hole in the skull bone.
- The dura mater (outer brain membrane) may be incised to allow further access, depending on the purpose.
- For hydrocephalus or ventricular procedures, catheters or shunts are inserted through the hole and into the ventricular system of the brain.
- Care is taken to minimize damage to surrounding tissues.
- Hemostasis is achieved via bone wax when necessary.
- The hole may be covered by the patient’s original bone fragment or with a specialized implant, particularly if postoperative imaging is needed.
- The scalp is closed with sutures or staples.
Innovations in Burr Hole Technique
- Sonolucent Burr Hole Covers: Modern burr hole procedures may include placement of a clear, sonolucent cover made of medical-grade plastic (e.g., PMMA). This allows repeated ultrasound imaging postoperatively without reopening the surgical site.
- Implant Fixation: These covers are secured with titanium plating systems for stability and longevity.
- Burr Hole Regrowth Prevention: Techniques and materials may be selected to minimize bone regrowth that might impede future imaging.
Risks of Burr Hole Procedures
Though generally considered safe, burr hole surgery—like any invasive procedure—carries some risk.
- Infection: Risks of wound infection or deeper cranial infection exist but remain low—studies show infection rates for sonolucent covers do not materially differ from standard procedures.
- Bleeding: Injury to blood vessels may occur and lead to subdural or epidural hematoma postoperatively.
- Damage to brain tissue: Precise technique mitigates but does not eliminate the potential for neural injury.
- CSF leak: Persistent cerebrospinal fluid leakage may require additional intervention.
- Burr Hole Regrowth: The bone may regrow rapidly within the first 6–12 months and stabilize afterward, potentially reducing visibility for future ultrasound imaging.
- Scarring and cosmetic changes: Minor, usually limited to the incision area.
- Rare complications: Seizures, neurologic deficits, or allergic reactions to anesthesia/implants.
Imaging and Follow-Up After Burr Hole Surgery
Imaging plays a crucial role both prior to and following burr hole procedures.
| Imaging Modality | Utility | Advantages | Limitations |
|---|---|---|---|
| CT (Computed Tomography) | Assess presence of bleeding, fluid, or device placement | Detailed, fast | Radiation exposure |
| MRI (Magnetic Resonance Imaging) | Comprehensive view of soft tissue, inflammation, abnormal growth | No radiation, high detail | Cost, longer procedure |
| Ultrasound (via burr hole) | Real-time assessment of ventricular size and anatomy through sonolucent covers | Radiation-free, portable | Requires engineered window, limited field of view |
In select patients, using a burr hole with a sonolucent implant facilitates repeated real-time ultrasound imaging for ongoing management, especially beneficial in hydrocephalus and similar disorders.
Bone Regrowth After Burr Hole Surgery
One notable physiological response after burr hole creation is bone regrowth. This regrowth can impact both function and postoperative evaluation.
- Time Frame: Greatest regrowth occurs in the first 6–12 months, typically stabilizing thereafter. Average closure may reach 25% at 6 months.
- Impact on Imaging: Significant bone regrowth can block ultrasound and reduce the utility of the window for future imaging.
- Prevention: Use of full-thickness implants and sonolucent materials can help preserve the window for imaging.
- Patient Factors: Age, sex, and skull thickness do not significantly influence regrowth rates.
Recovery After Burr Hole Surgery
Recovery varies based on the underlying reason for surgery and individual patient factors.
- Hospital stay: Most patients are monitored for 1–3 days postoperatively.
- Pain management: Mild to moderate discomfort managed with standard pain medications.
- Wound care: Clean incision and regular monitoring for signs of infection.
- Activity: Limit strenuous activity until the incision has healed and as advised by your neurosurgeon.
- Follow-up: Regular outpatient check-ups, imaging when indicated.
- Long-term considerations: In case of sonolucent covers, continued ultrasound checks may be scheduled for monitoring ventricular status in hydrocephalus or similar conditions.
Long-Term Outcomes and Patient Considerations
- Functional recovery: Most patients return to normal activities after a short convalescence.
- Cosmetic concerns: Incisions are typically small and minimally visible after healing.
- Risk of repeat procedures: Some conditions, such as chronic hematoma, may require additional intervention if symptoms recur.
- Imaging follow-up: Key for early detection of complications, especially in patients with implanted devices or covers.
Frequently Asked Questions (FAQs)
Q: What is the difference between a burr hole and a craniotomy?
A: A burr hole is a small, round opening made in the skull for minimally invasive access, while a craniotomy involves removing a larger section of skull bone to access more extensive areas of the brain. Burr holes are quicker, associated with less morbidity, and are suitable for certain diagnoses and treatments; craniotomy allows more complex procedures but carries greater risk.
Q: How soon will I recover after a burr hole procedure?
A: Most patients feel better within a few days, but full recovery depends on the underlying condition and overall health. Typical activities can resume gradually after the incision heals and your care team advises clearance.
Q: Does the burr hole close over time?
A: Bone regrowth is common, particularly within 6 to 12 months of the procedure. Most holes partly close, which may limit imaging utility if future scans are needed. Implant materials can help prevent complete closure for ongoing needs.
Q: Are there alternatives to a burr hole?
A: Alternatives depend on the exact medical problem. Other approaches might include craniotomy, stereotactic needle aspiration, or endoscopic procedures. Burr holes are frequently chosen for their speed and minimally invasive profile, especially for drainage and device placement.
Q: Is having a sonolucent burr hole cover safe?
A: Yes. Clinical studies show similar infection and revision rates to standard burr holes, with no significant increase in risk associated with sonolucent covers, and they allow ongoing ultrasound imaging of ventricular anatomy.
Conclusion: The Role and Future of Burr Holes in Neurosurgery
Burr holes remain a cornerstone of contemporary neurosurgical practice—offering safe, effective access for both emergency and planned brain interventions. With ongoing technical advancements, such as sonolucent covers, the utility of burr holes is expanding, making less invasive imaging and follow-up both practical and safe. Recognizing the indications, procedures, and outcomes associated with burr hole surgery allows patients and providers to make informed decisions about care.
References
Read full bio of Sneha Tete












