Breast Pain: 10 Reasons Your Breasts May Hurt
Understanding the common and uncommon causes of breast discomfort

Breast pain, medically known as mastalgia, is an incredibly common concern that affects women of all ages. While breast discomfort can be alarming, it’s important to understand that pain in the breasts is rarely a sign of breast cancer. Most cases of breast pain are related to hormonal fluctuations, lifestyle factors, or benign conditions that can be effectively managed. Understanding the various causes of breast pain can help you identify what might be triggering your discomfort and when it’s time to consult with a healthcare provider.
Breast pain manifests in different ways for different women. Some experience a dull, persistent ache, while others deal with sharp, shooting sensations. The discomfort may be cyclical, appearing and disappearing with your menstrual cycle, or it may be constant and unrelated to hormonal patterns. The pain might affect one breast or both, and it can range from mild irritation to severe discomfort that interferes with daily activities. By exploring the ten most common reasons for breast pain, you’ll be better equipped to understand your body and make informed decisions about your health.
Hormonal Fluctuations During Menstrual Cycle
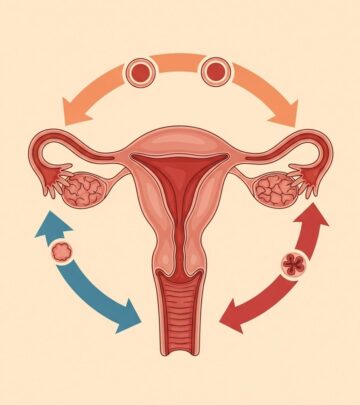
The most prevalent cause of breast pain is the natural hormonal changes that occur throughout your menstrual cycle. Hormone changes during your period are responsible for the majority of breast pain complaints among women of reproductive age. As estrogen and progesterone levels fluctuate during different phases of your cycle, your breast tissue responds to these hormonal shifts, often resulting in tenderness, swelling, and discomfort.
This type of cyclical breast pain typically begins a week or two before menstruation and usually subsides once your period starts. The discomfort is often bilateral, affecting both breasts, and may extend to the underarm area. Women describe this pain as a heavy, dull ache accompanied by breast fullness and swelling. The intensity can vary from cycle to cycle, with some months being more uncomfortable than others. Imbalances in estrogen and progesterone effects in the breast have been implicated in this type of mastalgia, and understanding this connection can help women better manage their symptoms.
Water Retention and Breast Swelling
Water retention is another common culprit behind breast pain, particularly in the days leading up to menstruation. When your body retains excess fluid, your breasts can become swollen, heavy, and tender to the touch. This fluid accumulation causes the breast tissue to stretch, leading to discomfort that can range from mild to quite significant.
The relationship between water retention and breast pain is closely tied to hormonal fluctuations, particularly changes in progesterone levels. As your body prepares for menstruation, progesterone causes your body to hold onto more water, which accumulates in various tissues, including your breasts. Women who are particularly sensitive to these hormonal changes may experience more pronounced swelling and pain. Reducing salt intake and staying well-hydrated can sometimes help minimize water retention and the associated breast discomfort.
Breast Injury and Trauma
Physical injury to the breast can result in immediate or delayed pain that may persist for days or even weeks. Injuries can occur from various sources, including sports activities, accidents, falls, or even vigorous exercise without proper breast support. The breast tissue, which contains delicate structures including milk ducts, fatty tissue, and connective tissue, can be easily bruised or damaged.
Following an injury, you might notice localized pain, bruising, swelling, or tenderness in the affected area. The pain may be sharp initially and then transition to a dull ache as healing progresses. Even minor trauma that doesn’t seem significant at the time can cause lingering discomfort. In some cases, injury to the breast can lead to the formation of scar tissue or fat necrosis, which may create a palpable lump and ongoing pain. If you’ve experienced breast trauma and the pain doesn’t improve within a reasonable timeframe, consulting with a healthcare provider is recommended.
Pregnancy-Related Breast Changes
Pregnancy brings dramatic hormonal changes that significantly affect breast tissue, particularly during the first trimester. Many women report that breast tenderness and pain are among the earliest signs of pregnancy, sometimes occurring even before a missed period. The surge in hormones, particularly estrogen and progesterone, causes the breasts to prepare for milk production, resulting in substantial changes to breast tissue.
During pregnancy, breasts typically become larger, heavier, and more sensitive. The milk ducts expand, blood flow increases, and fatty tissue accumulates, all contributing to discomfort. Women often describe this pain as a constant soreness or tenderness, particularly when touching or applying pressure to the breasts. The nipples may also become extremely sensitive. While this discomfort can be challenging, it’s a normal part of pregnancy and usually indicates that your body is preparing properly for breastfeeding. Wearing a well-fitted, supportive bra and using warm or cold compresses can provide relief during this time.
Breastfeeding Challenges
Nursing mothers frequently experience various types of breast pain related to the breastfeeding process. While breastfeeding is natural, it doesn’t always come easily, and several complications can cause significant discomfort. Common breastfeeding-related causes of breast pain include engorgement, blocked milk ducts, improper latch, and infections such as mastitis.
Engorgement occurs when breasts become overly full of milk, causing them to feel hard, swollen, and painful. Blocked milk ducts create localized areas of tenderness and may appear as firm, painful lumps within the breast. An infection in the breast, known as mastitis, produces intense pain along with redness, warmth, and sometimes fever. Additionally, if a baby doesn’t latch properly, it can cause nipple trauma and breast pain that extends beyond the immediate nursing session. Working with a lactation consultant can help address many of these issues and make breastfeeding more comfortable.
Medication Side Effects
Numerous medications can cause breast pain as a side effect, particularly those that affect hormone levels in the body. Some medicines, including hormone therapies such as birth control pills, hormone replacement therapy, and fertility treatments, commonly list breast tenderness as a potential adverse effect. The synthetic hormones in these medications can stimulate breast tissue in ways similar to natural hormonal fluctuations, leading to pain and discomfort.
Beyond hormonal medications, certain antidepressants, blood pressure medications, and some antibiotics have also been associated with breast pain. Additionally, medications like digoxin (used for heart conditions), methyldopa (for high blood pressure), and spironolactone (a diuretic) can affect breast tissue and cause discomfort. If you suspect your medication is causing breast pain, don’t stop taking it without consulting your healthcare provider. They may be able to adjust your dosage or switch you to an alternative medication that doesn’t produce this side effect.
Breast Cancer Considerations
While breast cancer rarely causes pain as its primary symptom, it’s important to acknowledge that it can happen in some cases. Most breast cancers are discovered through the detection of a painless lump, changes in breast appearance, or abnormal mammogram results rather than through pain. However, inflammatory breast cancer, a rare and aggressive form of the disease, can present with pain, redness, swelling, and warmth in the affected breast.
It’s crucial to understand that the vast majority of breast pain is not related to cancer. However, if you experience persistent breast pain accompanied by other concerning symptoms such as a palpable lump, skin changes, nipple discharge, or changes in breast shape or size, you should seek medical evaluation promptly. Regular breast self-examinations, clinical breast exams, and mammograms according to recommended guidelines are essential for early cancer detection, regardless of whether you’re experiencing pain.
Post-Surgical Breast Pain
Surgery from a biopsy, breast reduction, or a mastectomy can result in both acute and chronic breast pain. Any surgical procedure involving the breast creates trauma to the tissue, which requires time to heal. Immediately following surgery, pain is expected and typically managed with prescribed pain medications. However, some women experience ongoing discomfort that persists well beyond the initial healing period.
Post-surgical pain can result from nerve damage during the procedure, scar tissue formation, or complications during healing. Myofascial pain syndrome is one potential cause of chronic pain in breast cancer survivors who have undergone surgery, particularly when axillary lymph node dissection is involved. This condition involves trigger points in muscle tissue that cause referred pain and can significantly impact quality of life. Studies have shown that a substantial percentage of women develop this syndrome following breast cancer surgery, highlighting the importance of proper post-operative care and pain management strategies.
Inadequate Breast Support
An unsupportive bra or wearing the wrong bra size is a surprisingly common yet often overlooked cause of breast pain. Many women wear bras that don’t fit properly, either because they’ve never been professionally fitted or because their breast size has changed due to weight fluctuations, pregnancy, or aging. Breasts, which have no muscle tissue of their own, rely on ligaments called Cooper’s ligaments for support. Without adequate external support from a well-fitted bra, these ligaments can become strained, leading to discomfort.
Women with larger breasts are particularly susceptible to pain from inadequate support, as the weight of the breast tissue pulls on the chest wall, shoulders, and back. During physical activity, breasts can move significantly without proper support, causing pain and potential tissue damage. Wearing a bra that offers good support, particularly during exercise, can make a substantial difference in comfort levels. Getting professionally fitted for a bra and replacing worn-out bras regularly are simple steps that can prevent or alleviate breast pain related to inadequate support.
Musculoskeletal and Chest Wall Pain
Not all pain perceived as breast pain actually originates in the breast tissue itself. Musculoskeletal conditions affecting the chest wall, ribs, or muscles beneath the breasts can create sensations that feel like breast pain. Costochondritis, an inflammation of the cartilage connecting the ribs to the breastbone, is a common cause of chest wall pain that women may mistake for breast pain. Similarly, muscle strain in the pectoral muscles from exercise or poor posture can produce discomfort that seems to come from the breast.
Myofascial pain syndrome, characterized by trigger points in muscle tissue that refer pain to other areas, can also manifest as breast pain. This regional pain syndrome affects palpable taut bands of skeletal muscle and can cause distant motor and autonomic effects. Activities that strain the chest muscles, such as heavy lifting, rowing, or even prolonged computer work with poor ergonomics, can trigger this type of pain. Distinguishing between true breast pain and musculoskeletal pain is important because the treatment approaches differ significantly.
When to Seek Medical Attention
While most breast pain is benign and resolves on its own, certain circumstances warrant medical evaluation. If you have breast pain that lasts a long time or keeps coming back, you should talk to your doctor. Additionally, seek medical attention if your breast pain is accompanied by a lump or thickening in the breast, changes in breast skin texture or appearance, nipple discharge (especially if bloody), redness or warmth suggesting infection, or pain that significantly interferes with daily activities.
Your doctor will examine you, ask you to describe your pain, and determine the location of the pain. During the exam, your doctor will check to see if you have lumps in your breasts. Depending on your age and symptoms, your doctor may recommend additional testing. If you’re younger than 30 and don’t have a breast lump, your doctor might decide you don’t need any tests. However, if you’re older than 30, even without a palpable lump, your doctor may want you to get additional tests, especially if you are experiencing persistent pain.
Diagnostic Procedures for Breast Pain
When breast pain requires investigation, several diagnostic tools can help identify the underlying cause. A mammogram is a special X-ray of the breasts that can detect abnormalities in breast tissue, including masses, calcifications, or architectural distortions. While mammograms are primarily screening tools for breast cancer, they can also identify other conditions that might be causing pain.
A breast ultrasound is a painless test that uses sound waves to create images of breast tissue. This imaging modality is particularly useful for evaluating palpable lumps, assessing dense breast tissue (common in younger women), and distinguishing between solid masses and fluid-filled cysts. If imaging reveals a suspicious area, a breast biopsy may be necessary. During this procedure, tissue is surgically removed from your breast and examined under a microscope. The area being sampled is numbed to eliminate pain, and the procedure is typically performed on an outpatient basis.
Treatment and Management Strategies
There are different treatments for breast pain, depending on what is causing it. For cyclical breast pain related to hormonal fluctuations, lifestyle modifications may provide relief. While there’s no definitive scientific evidence that lifestyle changes are universally effective, some women feel better when changing bra styles and cutting back on salt and caffeine. Reducing alcohol intake, maintaining a healthy weight, and getting regular exercise may also help, as alcohol intake, inactivity, and obesity have been associated with increased breast cancer risk and potentially more pronounced breast symptoms.
Wearing a bra that offers good support is one of the simplest yet most effective interventions for breast pain. Applying ice or heat to the painful breast can provide temporary relief, with cold helping to reduce inflammation and heat promoting relaxation of tense tissue. Taking an over-the-counter pain medicine such as ibuprofen or acetaminophen can help manage discomfort. For more severe pain, your doctor may prescribe stronger pain medication or consider hormonal treatments. Research has shown that medroxyprogesterone acetate effectively suppresses cyclic mastalgia in reproductive-age women, though its use requires careful consideration of potential side effects and individual patient factors.
Living with Breast Pain
Most of the time, breast pain goes away on its own after a few months, particularly when it’s related to hormonal fluctuations or temporary conditions. However, understanding your pain patterns and triggers can help you manage symptoms more effectively. Keeping a pain diary that tracks when pain occurs, its intensity, and any associated factors (such as menstrual cycle phase, activities, or dietary choices) can provide valuable insights for both you and your healthcare provider.
For chronic or recurrent breast pain, developing a comprehensive management strategy is important. This might include a combination of appropriate supportive garments, pain relief measures, stress management techniques, and regular follow-up with your healthcare provider. If you are experiencing long-term pain that isn’t going away, don’t hesitate to seek medical evaluation. Persistent breast pain can significantly impact quality of life, and you deserve appropriate assessment and treatment to address your symptoms effectively.
Frequently Asked Questions
Q: Is breast pain a common symptom of breast cancer?
A: No, breast pain rarely indicates breast cancer. Most breast cancers present as painless lumps or are detected through screening mammograms. However, if pain is accompanied by other concerning symptoms like lumps, skin changes, or nipple discharge, medical evaluation is warranted.
Q: Can birth control pills cause breast pain?
A: Yes, birth control products can cause breast pain as a side effect. The synthetic hormones in contraceptives can stimulate breast tissue similarly to natural hormonal fluctuations, leading to tenderness and discomfort, especially when first starting the medication.
Q: How long does breast pain typically last?
A: The duration of breast pain varies depending on the cause. Cyclical pain related to menstruation typically lasts one to two weeks before your period and resolves once menstruation begins. Non-cyclical pain may persist longer but often resolves within a few months without treatment.
Q: Should I avoid caffeine if I have breast pain?
A: While scientific evidence is limited, some women report improvement in breast pain symptoms when they reduce or eliminate caffeine consumption. If you suspect caffeine might be contributing to your discomfort, consider reducing your intake to see if symptoms improve.
Q: Does being overweight increase the risk of breast pain?
A: Obesity can contribute to breast pain in several ways. Excess weight can increase hormonal fluctuations, place additional strain on breast ligaments, and make finding properly supportive bras more challenging. Maintaining a healthy weight through diet and exercise may help reduce breast pain symptoms.
Q: When should I see a doctor about breast pain?
A: Seek medical attention if your breast pain persists for more than a few weeks, is severe enough to interfere with daily activities, is accompanied by a lump or skin changes, or if you notice nipple discharge. Women over 30 with new onset breast pain should also consult their healthcare provider.
Q: Can stress cause breast pain?
A: While stress doesn’t directly cause breast pain, it can exacerbate existing discomfort and may influence hormonal balance. Stress can also increase muscle tension in the chest wall, which might be perceived as breast pain. Managing stress through relaxation techniques may help reduce overall discomfort.
References
- https://familydoctor.org/condition/breast-pain-in-women/
- https://pure.johnshopkins.edu/en/publications/influence-of-parenteral-progesterones-on-the-prevalence-and-sever-4
- https://pure.johnshopkins.edu/en/publications/incidence-of-myofascial-pain-syndrome-in-breast-cancer-surgery-a-
- https://www.jhah.com/en/news-events/news-articles/fight-against-breast-cancer/
- https://publichealth.jhu.edu/2016/women-may-be-able-to-reduce-breast-cancer-risk-predicted-by-their-genes
Read full bio of medha deb