Breast Cancer: Diagnosis and Treatment Options Explained
Comprehensive guide to breast cancer diagnosis, treatment modalities, innovations, and ongoing care for optimal outcomes.
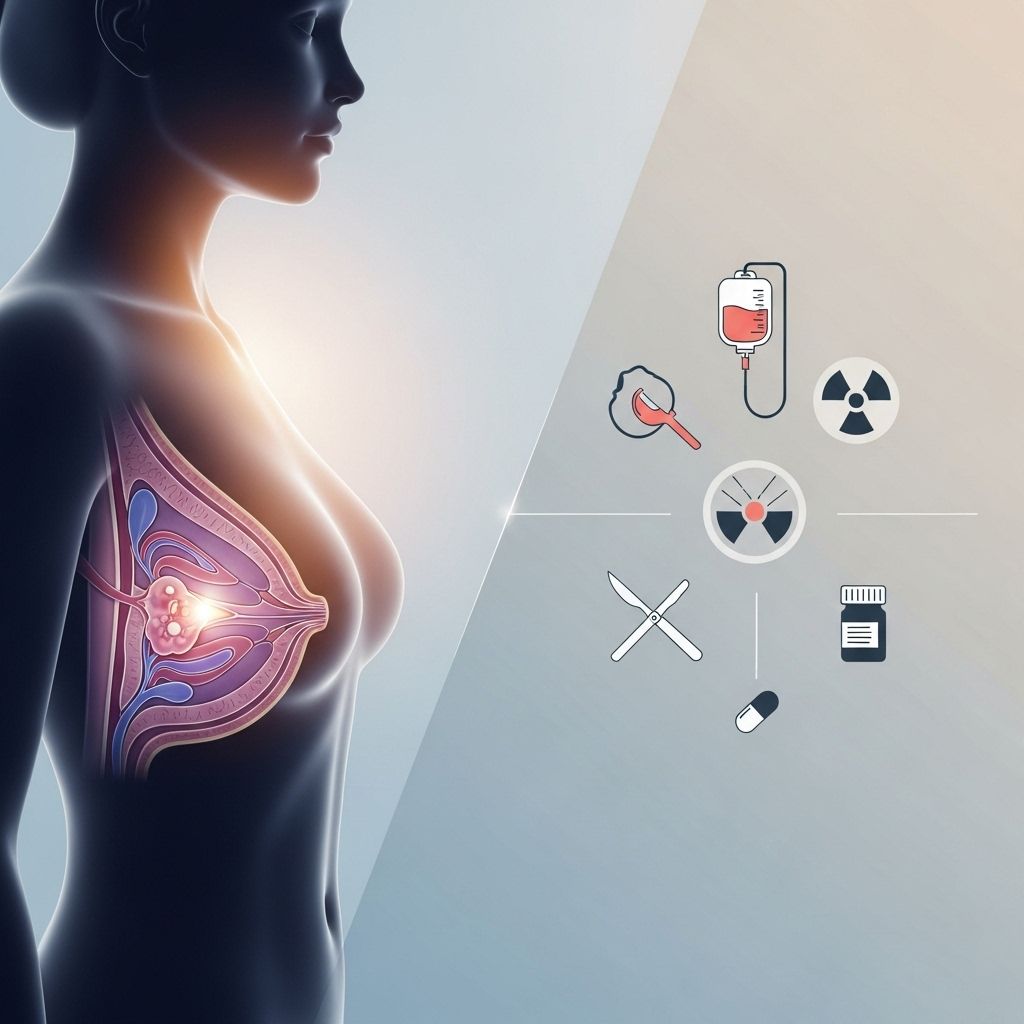
Breast Cancer Diagnosis and Treatment
Breast cancer is among the most common malignancies worldwide, affecting millions of individuals each year. Appropriate diagnosis and selection of effective therapies are crucial for improved outcomes and quality of life. This comprehensive guide explores the latest approaches to breast cancer diagnosis, treatment options, recent innovations, and the supportive therapies that play essential roles in both recovery and survivorship.
Diagnosing Breast Cancer
The path to treating breast cancer begins with an accurate diagnosis. Modern technology and specialist expertise have made it possible to detect cancer at earlier stages and tailor diagnostic approaches according to each patient’s unique risk factors and medical history.
- Breast Imaging
- Digital mammograms: Standard screening tool for detecting abnormal growths.
- 3D mammogram (tomosynthesis): Provides layered images of breast tissue for better accuracy in detection and assessment.
- Breast MRI: Used for high-risk screening, dense breast tissue, or ambiguous imaging results.
- Molecular breast imaging (MBI): Uses radioactive tracers to locate abnormalities, especially useful in dense breasts.
- Contrast-enhanced digital mammography (CEDM): Improves visibility of certain tumors with contrast agents.
- Biopsy Procedures
- Image-guided needle biopsy: Includes ultrasound, stereotactic, and MRI-guided techniques for sampling suspicious tissue accurately.
- Surgical biopsy: Reserved for cases where imaging or needle biopsy is inconclusive.
- Genetic Counseling and Testing
- Genetic evaluation for hereditary cancer risk factors (BRCA1, BRCA2, etc.) and tailored risk management plans.
- Advanced Diagnostics
- Precision medicine: Diagnostic studies of tumor genetics guide individualized therapy plans.
- Bioimpedance screening: Helps assess lymphedema risk and diagnosis.
Specialized radiologists and breast imaging experts play essential roles in accurate interpretation and early detection, which is crucial for improved clinical outcomes .
Treatment Options for Breast Cancer
Treatment strategies for breast cancer are multifaceted and highly personalized. Most management plans involve a combination of therapies, aiming to eliminate cancer cells, reduce recurrence risk, and minimize side effects while considering patient preferences and overall health.
- Surgery
- Lumpectomy: Removal of the tumor and a small margin of healthy tissue, often paired with radiation and ideal for localized cancers.
- Mastectomy: Complete removal of the affected breast. Options include skin-sparing and nipple-sparing procedures to enhance post-surgical appearance.
- Breast reconstruction: Surgical restoration performed during or after mastectomy to improve cosmetic outcomes and psychological well-being.
- All-in-one procedures: Some centers combine mastectomy and reconstruction in a single operation, enhancing convenience and recovery.
- Radiation Therapy
- Traditional radiation therapy: Targets cancer cells locally after breast-conserving surgery.
- Proton therapy: Offers precision targeting, sparing healthy heart and lung tissue—a significant advancement, especially for left-sided breast cancers.
- Accelerated partial breast irradiation: Delivers radiation over shorter periods, reducing treatment schedule from weeks to days for eligible patients.
- Chemotherapy
- Systemic treatment to destroy cancer cells or shrink tumors before (neoadjuvant) or after surgery.
- Infusion therapy: Delivered intravenously, often managed in outpatient clinics.
- Hormone Therapy
- For hormone receptor-positive breast cancer, medications block estrogen and progesterone’s effects on cancer cells, reducing recurrence risks.
- Targeted Therapy
- Drugs designed to inhibit specific molecular pathways crucial for cancer cell survival (e.g., HER2-targeted therapies).
- Clinical Trials and Research
- Patients may qualify for ongoing research studies exploring novel therapies, improving outcomes or reducing side effects.
- Supportive and Integrative Therapies
- Lymphedema management and education
- Physical therapy for recovering movement and function post-surgery or radiation
- Nutrition and dietary counseling
- Alternative therapies: Mind-body techniques, acupuncture, and symptom management strategies
- Scalp cooling cap: Used to reduce hair loss from chemotherapy
- Medication management and pharmacogenomics: Ensures optimal drug choices and dosing
Innovations in Breast Cancer Care
Recent years have seen significant innovations in both diagnosis and treatment, improving cure rates and reducing the side effects and long-term impact of therapies.
- Imaging Advances
- 3D mammography and molecular imaging for higher accuracy, particularly for high-risk or dense breast tissue individuals.
- Dynamic contrast-enhanced MRI and advanced digital imaging are improving detection and characterization of breast tumors.
- Minimally Invasive Procedures
- Sentinel lymph node biopsy: Limits lymph node removal, minimizing the risk of lymphedema and other complications.
- Neoadjuvant therapy: Shrinks tumors preoperatively, allowing for less invasive surgeries.
- Intraoperative pathology: Frozen section analysis of tissue samples during lumpectomy help avoid second surgeries.
- Precision Medicine
- Tumor genetic profiling guides personalized therapy plans, improving efficacy and minimizing unnecessary treatment.
- Clinical Trials
- Investigational drugs, therapies, and radioactive beam shaping techniques continue to expand the treatment arsenal while limiting tissue damage (like proton therapy for precise radiation).
Personalized Breast Cancer Care Plans
Every breast cancer patient is unique, and leading breast centers, such as those at Mayo Clinic, emphasize individualized care based on the specific characteristics of the cancer, patient health, preferences, and goals.
- Reviewing all available treatment options and coordinating appointments across specialties to allow timely decision-making.
- Convenient treatment scheduling that minimizes travel, such as combining lumpectomy with accelerated partial breast irradiation, or mastectomy with immediate reconstruction.
- Coordination with local physicians: Chemotherapy and other treatments can sometimes be managed close to home for convenience.
- Risk assessment and preventive care for those with strong family history or known genetic predispositions, including options for preventive surgery or additional screening.
Supportive Therapy, Recovery, and Survivorship
Beyond treating cancer, supportive care is vital to optimize recovery, manage side effects, rehabilitate physical function, and support the psychological and social needs of survivors.
- Lymphedema management to reduce fluid buildup and limb swelling
- Physical rehabilitation for regaining movement, strength, and everyday function
- Dietitian consultation for healthy eating and management of treatment-related symptoms
- Psychological and social worker support for emotional well-being
- Cancer education and survivorship programs
Survivorship care includes regular follow-up, monitoring for recurrence, side effect control, and interventions to restore quality of life.
Risk Management and Prevention
For individuals at high risk due to family history or genetic mutations (BRCA1, BRCA2, etc.), specialized clinics offer risk assessment, counseling, chemoprevention strategies and preventive surgeries:
- Prophylactic Mastectomy or Oophorectomy: Surgical risk reduction measures for those at high hereditary risk.
- High Risk Breast Clinics: Personalized assessment and tailored surveillance plans to detect disease early and minimize risk.
- Chemoprevention: Use of medications to lower cancer risk in some genetically susceptible individuals.
Table: Overview of Breast Cancer Treatment Modalities
| Treatment Modality | Description | Key Benefits | Typical Side Effects |
|---|---|---|---|
| Surgery | Removal of tumor or breast; reconstructive options | Elimination of localized cancer, cosmetic restoration | Pain, scarring, lymphedema, infection risk |
| Radiation Therapy | Use of high-energy rays to destroy cancer cells | Local recurrence prevention | Skin changes, fatigue, cardiac/lung effects |
| Chemotherapy | Drugs to kill or slow tumor cells | Treatment of local/advanced/metastatic cancer | Nausea, hair loss, fatigue, infection risk |
| Hormone Therapy | Blocks hormones that fuel cancer growth | Reduces recurrence in hormone-sensitive disease | Hot flashes, osteoporosis, mood changes |
| Targeted Therapy | Targets specific cancer cell pathways | Precision action, often fewer side effects | Heart effects, skin changes, GI symptoms |
| Supportive Therapy | Care for side effects, rehabilitation, nutrition | Improved recovery, quality of life | Rare, variable |
Frequently Asked Questions (FAQs)
Q: What is the first step after a breast cancer diagnosis?
A: Initial evaluation involves thorough imaging and biopsy, followed by discussion with an expert multidisciplinary team to determine the best individualized treatment plan.
Q: Are there alternatives to mastectomy for early-stage cancer?
A: Yes, breast-conserving surgery (lumpectomy) followed by radiation therapy is effective for many women with early-stage disease.
Q: How is treatment tailored to individual patients?
A: Diagnostic information, tumor genetics, personal preferences, and health history all guide the choice of surgery, drug therapy, radiation, and supportive care.
Q: How do innovations like proton therapy benefit patients?
A: Proton therapy allows the cancer to be targeted with minimal exposure to healthy tissue, reducing risks to the heart and lungs especially in left-sided breast cancer.
Q: What support resources are available during and after treatment?
A: Comprehensive support includes physical therapy, nutrition, psychological help, social work, lymphedema management, education, and survivorship programs.
Summary
Breast cancer care is rapidly evolving, with an increasing focus on individualized diagnosis, cutting-edge treatment options, management of side effects, and optimizing overall health and well-being. Advances in imaging, surgery, radiation, medications, and supportive therapies mean that more people than ever not only survive breast cancer, but thrive in recovery and survivorship. Multidisciplinary teams, ongoing research, and a patient-centered approach are transforming the landscape of breast cancer treatment for the better.
References
- https://www.mayoclinic.org/departments-centers/breast-clinic/sections/overview/ovc-20459469
- https://www.mayoclinic.org/diseases-conditions/breast-cancer/care-at-mayo-clinic/mac-20352479
- https://www.mayoclinichealthsystem.org/services-and-treatments/breast-cancer-care
- https://www.mayoclinic.org/diseases-conditions/breast-cancer/diagnosis-treatment/drc-20352475
- https://www.mayoclinic.org/diseases-conditions/breast-cancer/symptoms-causes/syc-20352470
- https://www.mayoclinic.org/diseases-conditions/inflammatory-breast-cancer/diagnosis-treatment/drc-20355417
- https://www.youtube.com/watch?v=mCmJQGpjGNA
- https://www.mayoclinic.org/diseases-conditions/cancer/diagnosis-treatment/drc-20370594
- https://www.mayoclinic.org/diseases-conditions/recurrent-breast-cancer/diagnosis-treatment/drc-20377141
Read full bio of medha deb












