Understanding the Brain-Gut Connection in IBS-C: How Your Mind Affects Constipation
Learn how the complex relationship between your brain and gut impacts IBS-C symptoms and constipation, and discover holistic management options.
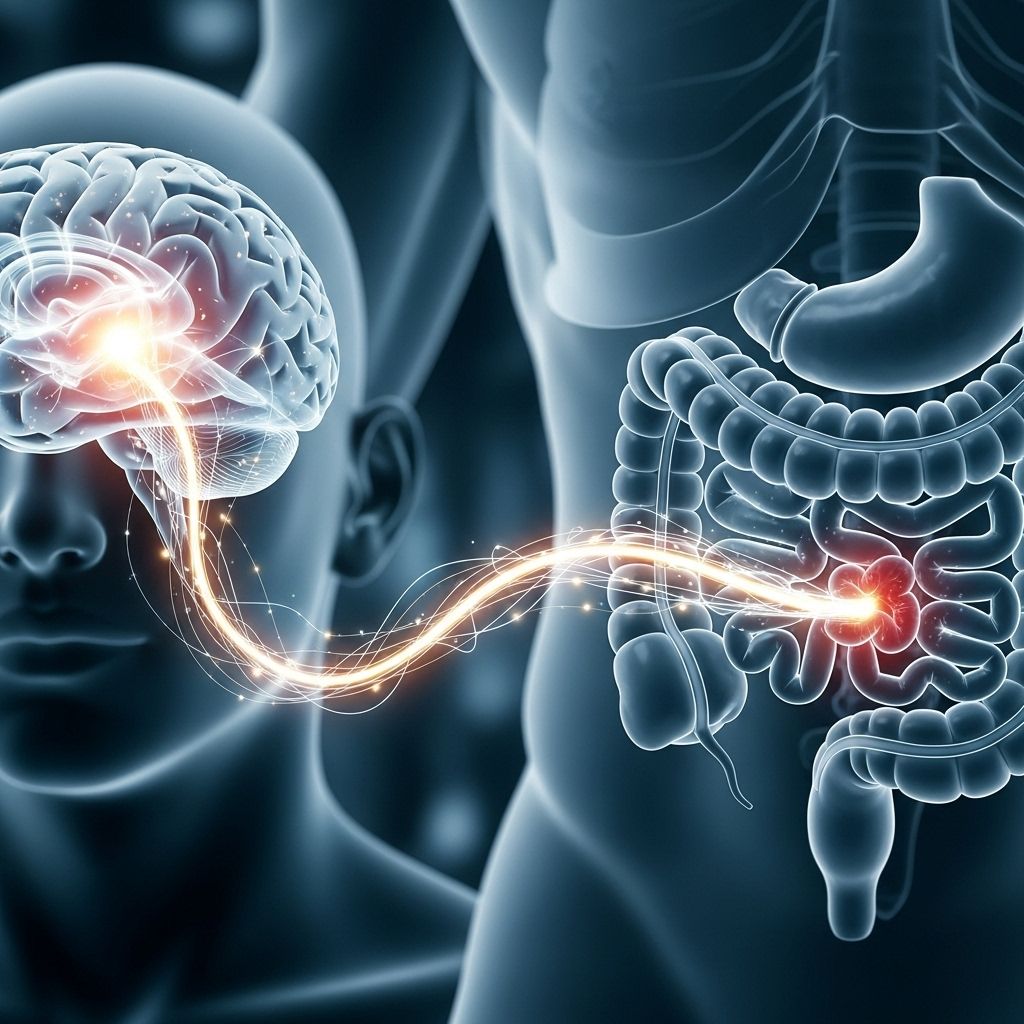
Understanding IBS-C and the Brain-Gut Connection
Irritable bowel syndrome with constipation (IBS-C) affects millions of people worldwide, yet its underlying causes are complex and often misunderstood. Modern research emphasizes that IBS-C is not just a disorder of digestion, but a condition deeply connected to how the brain and gut communicate. This interaction, known as the brain-gut axis, plays a crucial role in shaping symptoms, emotional health, and overall quality of life.
What Is IBS-C?
IBS-C is a subtype of irritable bowel syndrome characterized primarily by constipation. Key symptoms include:
- Abdominal pain or discomfort
- Bloating
- Infrequent, hard, or lumpy stools
- Feeling of incomplete evacuation
Unlike other gastrointestinal (GI) disorders, IBS-C typically does not cause visible physical damage to the digestive tract. Instead, it disrupts normal GI function, resulting in unpredictable and often debilitating symptoms.
How Does the Brain-Gut Axis Affect IBS-C?
The brain-gut axis is a dynamic communication network involving the central nervous system (brain and spinal cord), the enteric nervous system (the “second brain” within your gut), and the trillions of bacteria comprising your gut microbiome. Signals flow constantly between the gut and the brain via nerves (like the vagus nerve), hormones, and immune molecules.
This bidirectional feedback influences:
- Gut motility (how quickly food moves through the intestines)
- Perception of pain
- Digestive secretions
- Immune activity
- Mood and stress response
In people with IBS-C, this communication becomes disrupted, leading to hypersensitivity, abnormal bowel movements, and heightened responses to stress and anxiety.
How Stress, Anxiety, and Emotions Influence the Gut
Have you ever felt “butterflies in your stomach” before a big moment? This sensation highlights the power of the brain-gut connection. Stress, anxiety, and emotional states can dramatically impact gut function, sometimes triggering or worsening IBS-C symptoms.
- When we perceive threats, stress signals can alter digestive motility—slowing down or speeding up the movement of contents through the gut.
- Chronic stress and anxiety may fuel ongoing symptoms, contributing to cycles of constipation and discomfort.
Everyone has a gut-brain axis, but it’s especially sensitive in people with IBS. This sensitivity means psychological factors often play a larger role in perpetuating and intensifying symptoms than in other GI conditions.
Real-Life Impacts
- Food anxiety: Fear of eating certain foods due to unpredictable reactions
- Social avoidance: Worry about having symptoms in public
- Feeling isolated: Emotional distress from unpredictable symptoms
The uncertainty and unpredictability of IBS-C can lead to increased food restrictions and anxiety, which in turn affect digestive function, creating a negative feedback loop.
The Gut as Your Second Brain
The gut is often called the second brain because it contains over 100 million neurons—more than the spinal cord. This “enteric nervous system” can operate independently and drives digestive processes without direct input from the brain.
This system is responsible for:
- Peristalsis (waves that propel food through the intestines)
- Secretion of digestive enzymes
- Regulation of immune functions
- Sending signals to the brain indicating hunger, fullness, or the presence of pain or discomfort
Understanding the intelligence of the gut underscores why IBS-C cannot be managed by diet alone. Addressing the brain-gut axis is essential for comprehensive relief.
The Microbiome’s Role in IBS-C
Your gut microbiome—trillions of bacteria and other microorganisms—plays a pivotal role in brain-gut communication and digestive health. Healthy microbiota help regulate:
- Bowel movements
- Immune activity
- Mood chemicals (such as serotonin)
- Inflammation
When the balance of these microbes is disrupted, a state known as dysbiosis occurs. Dysbiosis is strongly linked to IBS-C, fueling symptoms like constipation, bloating, and even brain fog.
Microbiome Disruption and Its Effects
| Microbiome Function | Disruption Results |
|---|---|
| Regulate motility | Slowed transit, constipation |
| Produce mood chemicals | Lowered serotonin, increased anxiety/depression |
| Control inflammation | Chronic gut pain, bloating |
| Support immune system | Heightened immune response, discomfort |
Small Intestinal Bacterial Overgrowth (SIBO)
Some people with IBS-C also have SIBO, where excess bacteria accumulate in the small intestine, causing gas, bloating, and sometimes brain fog.
Brain Fog: Mental Effects of IBS-C
In addition to gastrointestinal symptoms, brain fog is common in IBS-C. This can involve hazy thinking, difficulty focusing, and mental fatigue. Researchers believe:
- Chronic pain or discomfort draws mental resources away from focus and clarity.
- Microbiome imbalance may send inflammatory or stress signals that affect cognition.
- Ongoing anxiety about symptoms intensifies mental cloudiness.
These effects often go overlooked, but addressing brain-gut communication can help improve both digestive and mental well-being.
Diagnosing and Managing IBS-C
Because IBS-C involves complex interactions between biology, psychology, and lifestyle, management often requires a multifaceted approach. Key steps for diagnosis and treatment include:
- Evaluation by a healthcare professional—to rule out other GI conditions and confirm IBS-C
- Symptom tracking—monitoring foods, bowel movements, symptoms, and stress levels
- Integrated management plan—tailored to address diet, mental health, microbiome, and lifestyle
Common Management Strategies
Effective IBS-C relief often requires combining approaches:
- Dietary modifications: Adjusting fiber intake, identifying trigger foods, experimenting with low-FODMAP diets
- Probiotics and prebiotics: Improving gut bacterial balance (consult a medical professional before starting supplements)
- Stress management: Mindfulness, cognitive-behavioral therapy (CBT), yoga, and relaxation techniques
- Medications: Laxatives, antispasmodics, or other drugs as prescribed
- Physical activity: Regular exercise can help stimulate intestinal motility and reduce anxiety
Individual results vary; dietary and lifestyle changes may help many, but not all. For some, treating psychological distress—often with the help of therapists or psychologists specializing in gut-brain disorders—can unlock significant improvement.
Enhancing Brain-Gut Communication
Improving the connection across the brain-gut axis can lead to symptom relief and restore gut function. Techniques include:
- Mindful eating: Eating slowly, appreciating flavors, and tuning into hunger/fullness signals
- Breathwork: Calming the nervous system via controlled breathing
- Relaxation therapies: Meditation, gentle movement, and therapy practices
- Building emotional awareness: Recognizing and responding to stress before it affects the gut
Strengthening this communication can help break negative cycles, reduce food-related anxiety, and improve overall well-being.
Frequently Asked Questions (FAQs)
Q: How does stress worsen IBS-C symptoms?
A: Stress triggers chemical and hormonal changes in the body, which disrupt normal gut motility, increase pain sensitivity, and often worsen constipation.
Q: Why can the same food bother me on some days but not others?
A: IBS-C symptoms are variable—factors like stress, sleep, and hormonal fluctuations can change how your body responds to certain foods.
Q: Can improving my mental health help my constipation?
A: Yes; mental health interventions such as therapy and stress management can decrease constipation frequency and severity in IBS-C.
Q: Are probiotics helpful for brain-gut axis problems?
A: Some probiotics can balance the gut microbiome, which may improve both gut and brain symptoms. However, effectiveness varies by individual, and consulting a professional is recommended.
Q: Is IBS-C a lifelong condition?
A: Symptoms can be chronic, but with the right approach many people experience relief by addressing both gut health and psychological factors.
Key Takeaways for Managing IBS-C
- IBS-C is a complex interplay between the brain and the gut; relief often involves more than dietary changes alone.
- Stress, anxiety, and emotional health are crucial drivers of symptoms and need focused attention.
- The gut microbiome regulates many aspects of digestive and mental health—disruptions can worsen symptoms.
- Holistic management integrates nutrition, mental health care, and lifestyle changes for the greatest chance at improvement.
Resources for Further Support
- Consult a gastroenterologist or gut-focused psychologist for persistent symptoms
- Explore evidence-based mind-gut therapies such as CBT, mindfulness, yoga
- Consider a registered dietitian to help tailor dietary approaches
If you or a loved one live with IBS-C, remember that understanding the brain-gut axis opens up new pathways for healing—going beyond food to include the mind, microbiome, and emotional wellness.
References
- https://badgut.org/information-centre/a-z-digestive-topics/brain-gut-connection-and-ibs/
- https://www.youtube.com/watch?v=JfmeXSkmfE4
- https://www.healthline.com/health/ibs-and-brain-fog
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5046167/
- https://www.healthline.com/nutrition/gut-brain-connection
- https://www.healthline.com/health/video/whats-the-scientific-link-between-your-gut-and-brain
- https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection
- https://ketteringhealth.org/ibs-the-mind-gut-connection/
Read full bio of Sneha Tete












