Blood Clot Treatment: Options, Risks, and Preventive Strategies
A comprehensive guide to understanding, treating, and preventing blood clots—covering therapies, risks, and the importance of ongoing care.
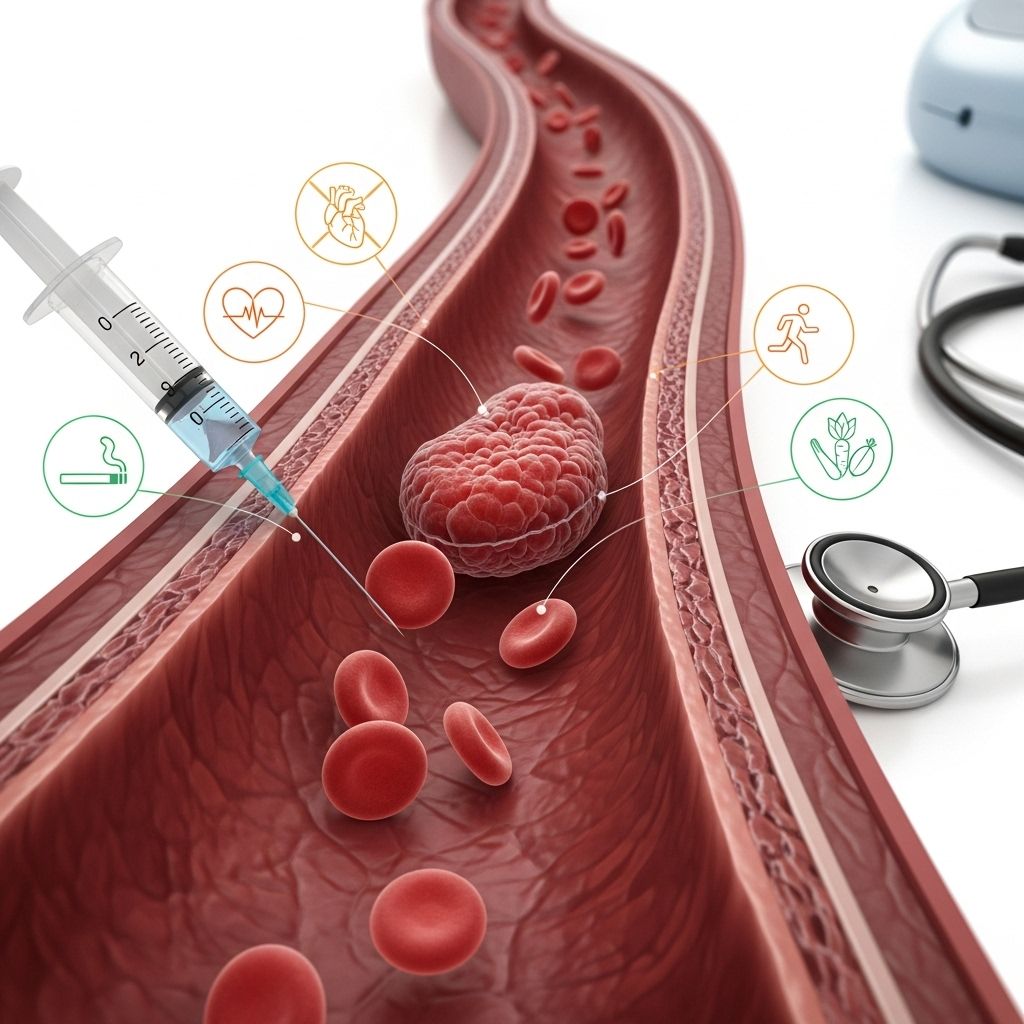
Blood clots—technically known as venous thromboembolism (VTE), encompassing both deep vein thrombosis (DVT) and pulmonary embolism (PE)—pose significant health risks and require timely and effective treatment. Management aims not only to treat acute events but also to reduce long-term complications and prevent recurrence. Understanding the causes, treatment options, and prevention strategies is critical to ensuring the best possible patient outcomes.
What Are Blood Clots?
Blood clots are semi-solid masses formed by coagulated blood components within vessels. They are vital for stopping bleeding after injury but can be dangerous when formed inside veins or arteries without injury, obstructing blood flow and causing tissue damage or death.
- Deep vein thrombosis (DVT): A clot in a deep vein, often in the leg or pelvis.
- Pulmonary embolism (PE): A clot that breaks loose and travels to the lungs, potentially life-threatening.
When Is Treatment Needed?
Treatment is required for most blood clots in deep veins or the lungs to prevent extension, recurrence, or potentially fatal complications such as PE. Some superficial or minimal distal clots may not require systemic anticoagulation; the decision is based on location, size, symptoms, and underlying risks.
Goals of Blood Clot Treatment
The primary objectives of blood clot treatment are to:
- Prevent the clot from growing larger
- Reduce the risk of the clot breaking loose and causing a PE
- Lower the chance of new clots forming
- Help the body naturally break down and remove the existing clot
- Minimize long-term complications, such as post-thrombotic syndrome
Treatment Options for Blood Clots
Treatment is tailored to the clot’s location, extent, underlying cause, and the patient’s risk factors. Fundamental approaches include:
1. Anticoagulant Medications (Blood Thinners)
Anticoagulants are medications that interrupt the clotting process, reduce the risk of clot extension, and help prevent new clots from forming. They do not actively dissolve existing clots but allow the body to break them down over time.
- Heparin (unfractionated or low molecular weight): Typically administered intravenously or by injection; acts quickly. Used in hospitals, especially for initial treatment.
- Low molecular weight heparin (LMWH): Given by subcutaneous injection. More predictable effects and often used for outpatient care.
- Direct oral anticoagulants (DOACs): Includes medications like rivaroxaban, apixaban, edoxaban, and dabigatran. These allow for oral therapy and do not require frequent blood tests.
- Vitamin K antagonists (e.g., warfarin): Oral medication, effectiveness monitored by the international normalized ratio (INR).
- Fondaparinux: A synthetic injectable medication used in specific cases.
Anticoagulation is the mainstay of blood clot therapy and may be recommended for at least three months, though duration varies with the triggering factors, risks, and presence of ongoing prothrombotic conditions.
2. Thrombolytic Therapy (Clot-Busting Drugs)
Thrombolytics are specialized medications utilized in emergencies, such as massive pulmonary embolism or severe DVT with limb-threatening symptoms, to rapidly dissolve clots. These carry significant risks, especially bleeding, and are typically reserved for critical cases.
3. Mechanical and Interventional Treatments
- Catheter-directed thrombolysis: A procedure in which clot-dissolving drugs are delivered directly to the clot via a catheter, sometimes combined with mechanical clot retrieval.
- Thrombectomy: Surgical or endovascular removal of a clot, indicated in very select, severe cases.
- Inferior vena cava (IVC) filters: Devices inserted into the vena cava (the large vein returning blood from the body to the heart) to trap clots and prevent them from reaching the lungs. Used when anticoagulation is not possible or effective; ideally retrieved when no longer needed.
4. Compression Therapy
For DVTs, especially in the legs, graded compression stockings may be recommended to help reduce swelling, promote blood flow, and lessen the risk of developing post-thrombotic syndrome (chronic leg swelling, pain, and skin changes after DVT).
Factors Affecting Treatment Choices
- Location and size of the clot (e.g., proximal vs. distal DVT, subsegmental vs. massive PE)
- Provoked vs. unprovoked clot: Was the clot triggered by a risk factor like surgery, trauma, or immobility, or did it occur spontaneously?
- Presence of ongoing risk factors: Such as cancer, inherited clotting disorders, or prolonged immobility
- Personal medical history: Including previous clots or history of major bleeding
- Risk of bleeding: Certain population groups and comorbidities make bleeding more likely, influencing the choice and duration of therapy.
Duration of Anticoagulation Therapy
The recommended duration for blood thinner therapy is based on the reason for the clot and individual risk assessment:
| Clot Type | Typical Treatment Duration | Comments |
|---|---|---|
| Provoked (e.g., surgery, trauma) | 3–6 months | If the risk factor is temporary and gone |
| Unprovoked or unknown cause | At least 3 months; may be indefinite | Assess for recurrence risk, ongoing factors |
| Ongoing risk (e.g., cancer, clotting disorder) | Long-term or lifelong | As long as risk persists |
| First episode, low bleeding risk | 3–6 months | May extend if risk factors remain |
Decisions regarding duration should be revisited periodically, especially for long-term users, to integrate new research findings, side effect monitoring, and changes in patient preference or condition.
Side Effects and Risks of Blood Clot Treatments
The most significant risk associated with anticoagulation is major bleeding. The risk depends on patient factors, medication type, and duration:
- Risk of bleeding: May include gastrointestinal bleeding, intracerebral hemorrhage, or bleeding at another site.
- Drug interactions and monitoring: Warfarin requires regular INR testing and has multiple drug/food interactions. DOACs generally need less monitoring but check for kidney and liver function.
- Allergic reactions or side effects: Rare but possible with any medication.
- Heparin-induced thrombocytopenia (HIT): A rare but serious immune reaction requiring immediate discontinuation of all heparin products.
- Skin changes and discomfort: Sometimes at injection sites or with prolonged use.
Who Manages Blood Clot Treatment?
Depending on the circumstances, a variety of health professionals may be involved in diagnosis, treatment, and follow-up:
- Primary care physicians: Assess initial symptoms and coordinate care.
- Hematologists: Specialists in blood disorders and coagulation.
- Vascular medicine or surgery specialists: Involved in more complex or severe cases, especially for interventional procedures.
- Anticoagulation clinics: Specialize in monitoring and dosing of blood thinners (particularly warfarin).
- Pharmacists and nurses: Educate, monitor, and support patients.
Blood Clot Prevention Strategies
Prevention is a cornerstone of VTE management for at-risk individuals, notably hospitalized or immobile patients. Safe and effective strategies can greatly reduce the incidence of serious blood clots.
- Medications: Low-dose anticoagulants for high-risk patients (hospitalized, after major surgery, etc.)
- Mechanical devices: Compression stockings and intermittent pneumatic compression devices to enhance blood flow in the legs.
- Early mobilization: Encouraging movement after surgery or during hospitalization significantly reduces risk.
- Hydration: Maintaining fluid balance helps prevent clotting, especially in patients unable to move freely.
- Lifestyle modification: Quitting smoking, managing weight, staying active, and controlling underlying health conditions (e.g., diabetes, hypertension) all help reduce risk.
Self-Monitoring and Ongoing Management
- Regular follow-up visits, at least yearly for long-term anticoagulant users
- Periodic lab work, especially for those on warfarin (INR) or with changes in health status
- Discussion of new research, medications, and potential dose adjustments based on life changes (e.g., surgery, travel, other illnesses)
- Open dialogue with the care team about bleeding or bruising, other side effects, and adherence challenges
Living with Blood Thinners: Safety Tips
People taking blood thinners need to be aware of how to safely incorporate this treatment into daily life:
- Carry medical identification indicating anticoagulation therapy
- Avoid high-risk activities that could lead to injury or bleeding
- Consult before starting new medications or supplements
- Report any unusual bleeding or signs of anemia (fatigue, paleness, rapid heartbeat) immediately
Frequently Asked Questions (FAQs)
Q: How long will I need to take a blood thinner for a clot?
A: The length of therapy depends on why the clot formed, its location, and your risk factors. Typical durations range from 3 months for a first, provoked clot, to indefinite therapy for recurrent or high-risk, unprovoked clots.
Q: Do blood thinners dissolve clots?
A: No, blood thinners do not dissolve existing clots but prevent further clotting and allow your body to gradually break down the clot on its own.
Q: Are there alternatives if I can’t take blood thinners?
A: Options such as IVC filters may be used in certain critical cases, but these have their risks. The need for an alternative will depend on your medical situation and will be discussed by your care team.
Q: What signs should prompt me to seek immediate medical attention?
A: Seek urgent care if you experience sudden shortness of breath, chest pain, coughing up blood, severe leg swelling or pain, fainting, or uncontrolled bleeding. These could be signs of a new clot or bleeding complication.
Q: Can I travel on blood thinners?
A: Yes, but take precautions: move your legs frequently, stay hydrated, and avoid prolonged immobility. Carry documentation about your medication during travel.
Key Takeaways
- Blood clot treatment is individualized, depending on location, cause, and ongoing risk.
- Anticoagulant medications remain the mainstay of therapy.
- Preventing blood clots, especially in high-risk settings, saves lives—prevention strategies are essential.
- Continued partnership with your health care team is critical for safe and effective management.
References
- https://pubmed.ncbi.nlm.nih.gov/26780738/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10559639/
- https://www.youtube.com/watch?v=cj-f6YPwbK8
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_Diabetes_Guide/547009/all/Anticoagulant_Use__Aspirin__Clopidogrel__Warfarin_
- https://pure.johnshopkins.edu/en/publications/vte-prophylaxis-and-treatment
- https://psnet.ahrq.gov/innovation/johns-hopkins-venous-thromboembolism-vte-collaborative-studies-and-implements-methods
Read full bio of medha deb












