Bladder Infection vs. UTI: Differences, Symptoms, and Treatment
Explore the differences, symptoms, causes, and treatments between bladder infections and UTIs to understand diagnosis and prevention.
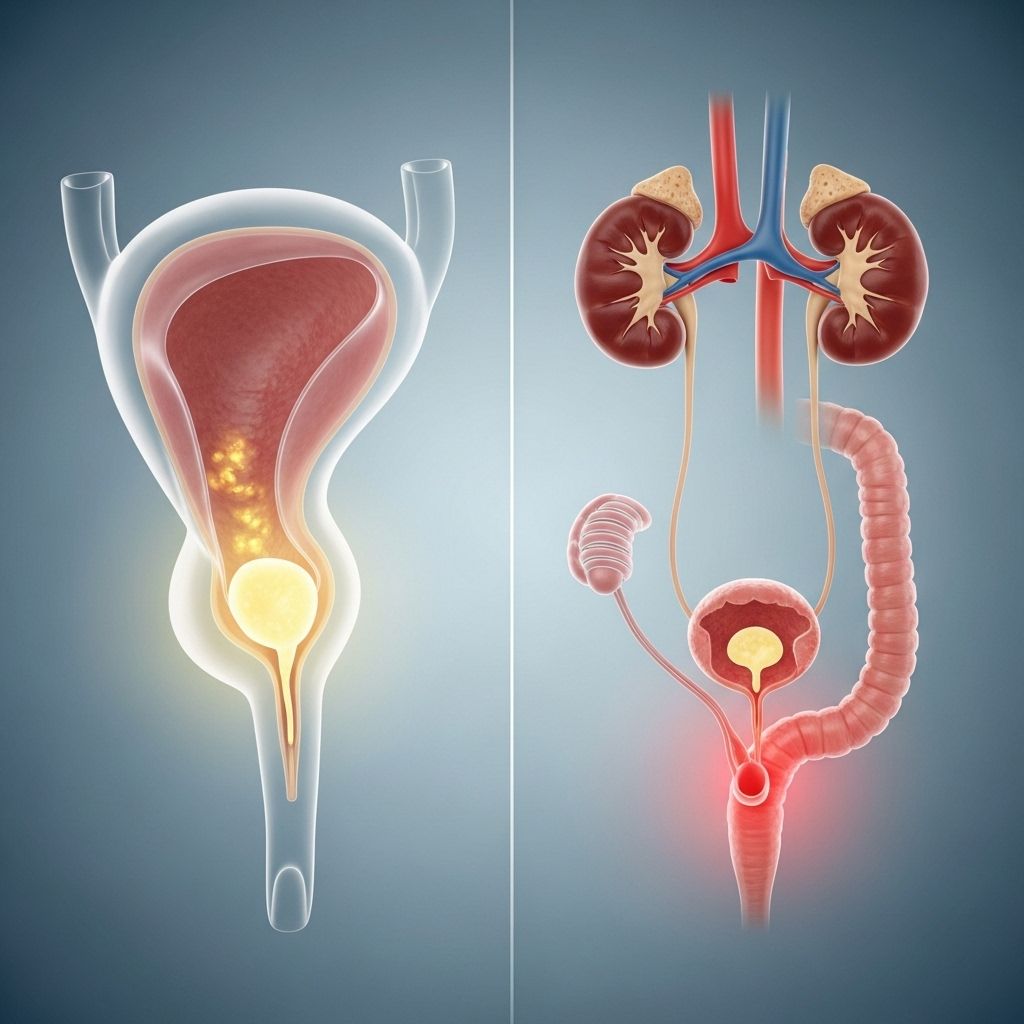
Bladder infections and urinary tract infections (UTIs) are two related yet distinct medical conditions that frequently affect people of all ages, especially women. Understanding the difference between a bladder infection—which is a specific type of UTI—and other forms of UTIs is crucial for proper diagnosis, treatment, and prevention. This comprehensive guide reviews their symptoms, causes, risk factors, complications, and best practices for management and care.
What Is a UTI?
Urinary tract infections (UTIs) are infections that can affect any part of the urinary system, including the kidneys, ureters, bladder, and urethra. Most commonly, UTIs involve the lower urinary tract—the bladder and urethra. However, an infection can progress to the upper urinary tract, affecting the kidneys, and potentially causing more severe health problems.
- The most common cause of UTIs is the bacterium Escherichia coli (E. coli), which typically enters the urinary tract through the urethra.
- UTIs are much more common in women than men due to anatomical differences.
- UTIs can be classified as lower UTIs (involving the bladder and urethra) and upper UTIs (involving the kidneys and ureters).
Bladder Infection vs. UTI: Key Differences
A bladder infection (often called cystitis) is the most common type of UTI, but not all UTIs are bladder infections. UTIs can also refer to infections of the kidneys (pyelonephritis) or urethra (urethritis).
| Feature | Bladder Infection (Cystitis) | UTI (General) |
|---|---|---|
| Definition | Infection limited to the bladder | Infection in any part of urinary tract |
| Symptoms | Burning during urination, frequent urge, pelvic pain | Symptoms depend on location; can include burning, pain, fever, back pain |
| Area affected | Bladder | Bladder, urethra, ureters, or kidneys |
| Severity | Generally less severe, but can worsen | Ranges from mild to severe (kidney infections can be serious) |
Symptoms of Bladder Infections and UTIs
Symptoms of UTIs and bladder infections can overlap, making self-diagnosis challenging. Still, certain signs can help distinguish between them:
- Frequent urge to urinate, even when little urine is produced
- Burning or pain during urination
- Cloudy or foul-smelling urine
- Lower abdominal or pelvic pain
Additional symptoms that may suggest a more severe (upper tract) UTI include:
- High fever with chills
- Flank or back pain (near the kidneys)
- Nausea or vomiting
- Fatigue and malaise
Bladder infection symptoms tend to be localized, while more systemic symptoms (fever, nausea) may indicate the infection has reached the kidneys.
Causes and Risk Factors
How Do UTIs and Bladder Infections Develop?
The vast majority of lower UTIs, including bladder infections, begin when bacteria from the digestive tract enter the urinary tract, typically through the urethra. They travel upwards, sometimes reaching the bladder or—in worse cases—the kidneys.
Main causes of bladder infections and UTIs:
- Escherichia coli (E. coli) is the bacterium responsible for most infections.
- Anatomical factors in females, such as a shorter urethra, allow easier bacterial access to the bladder.
- Using urinary catheters or having a suppressed immune system increases risk.
- Sexual activity can introduce bacteria into the urinary tract.
- Menopausal changes and certain birth control methods (like diaphragms) may also increase susceptibility.
Major Risk Factors
- Female sex: Women are more likely to develop UTIs due to shorter urethras and proximity to the anus.
- Sexual activity: Can transport bacteria into the urinary tract.
- Urinary tract abnormalities: Structural or functional problems can impede urine flow, leading to infection.
- Suppressed immunity: Chronic illnesses such as diabetes impair defenses.
- Catheter use: Increases exposure to bacteria.
- Menopause: Declining estrogen may disrupt normal bacterial balance in the urinary tract.
Diagnosis of Bladder Infections and UTIs
Diagnosis typically begins with a review of symptoms and a physical examination. Laboratory testing is often used to confirm infection and identify the causative organism.
- Urine analysis (urinalysis): Tests for white blood cells, red blood cells, and bacteria.
- Urine culture: Identifies the specific bacteria causing the infection.
- For recurrent or severe infections, imaging tests like ultrasound, CT scans, or cystoscopy may be recommended.
Prenatal screening for bacteria in the urine is routine, as UTIs during pregnancy can affect mother and baby.
Treatment
Most bladder infections and lower urinary tract infections are treated with oral antibiotics. Treatment regimens and choice of medication depend on the type of bacteria, severity of infection, and patient characteristics (like pregnancy or allergies).
Overview of Treatment Approaches
- Short courses of antibiotics (37 days): Typical for uncomplicated cases in otherwise healthy people
- Longer courses: For complicated or recurrent infections, or for upper tract involvement
- Increased fluid intake: Helps flush bacteria from the urinary tract
- Pain relief: Over-the-counter medications like acetaminophen or ibuprofen can be used
- Hospitalization: In severe cases, especially if the infection has spread to the kidneys, IV antibiotics may be necessary
Prompt treatment greatly reduces the risk of serious complications. Untreated infections may progress to the kidneys and possibly cause sepsis (spread of bacteria into the bloodstream), which is a life-threatening emergency.
Complications
While lower UTIs and bladder infections are usually minor if promptly treated, complications can arise if these infections are ignored or inadequately treated.
- Pyelonephritis: Kidney infection, which can present with fever, flank pain, chills, and vomiting
- Recurring infections: Multiple UTIs may signal underlying issues
- Sepsis: Particularly dangerous in the elderly, infants, and immune-compromised individuals
- Complications in pregnancy: Untreated UTIs can affect fetal health and may lead to low birth weight or premature birth
Prevention Tips
Several steps can reduce the risk of developing bladder infections and UTIs:
- Hydration: Drink plenty of water to dilute urine and flush out bacteria
- Urinate promptly: Don’t delay urination when you feel the urge
- Wipe front to back: After using the toilet, always wipe from front to back to prevent bacterial spread
- Urinate after sex: Helps remove bacteria that might have entered the urethra during intercourse
- Avoid irritating feminine products: Douches, deodorant sprays, and powders can disrupt the natural balance of bacteria
- Wear breathable underwear: Cotton allows for air flow and reduces moisture that could facilitate bacterial growth
For people with recurring infections, a healthcare provider may recommend preventive antibiotics or additional testing for anatomical issues.
When to Seek Medical Attention
If you experience symptoms of a bladder infection or UTI, it’s important to consult a healthcare provider—especially if:
- You have symptoms that persist beyond a day or worsen rapidly
- You have a fever, chills, nausea, or back pain (possible kidney involvement)
- You are pregnant or have underlying health conditions (like diabetes)
- You have blood in your urine
- You experience recurrent infections
Early intervention can prevent progression and minimize complications.
Bladder Infection vs. Other Genitourinary Infections
Bladder infections and UTIs are sometimes confused with other conditions, such as vaginal yeast infections (thrush) or sexually transmitted infections (STIs). However, there are key differences:
- Thrush is a fungal infection, typically causing vaginal itching, discharge, and discomfort. It is not caused by bacteria and requires antifungal therapy, not antibiotics.
- STIs may have overlapping symptoms but usually also cause discharge, sores, or pelvic discomfort, and are transmitted sexually.
- UTIs typically cause urinary symptoms without significant vaginal irritation.
Proper diagnosis is essential so that you receive the most effective treatment.
Frequently Asked Questions (FAQs)
How can you tell the difference between a UTI and a bladder infection?
The main way to distinguish is by the location of symptoms: Bladder infections (cystitis) are a type of UTI that specifically involve the bladder, causing symptoms like burning during urination, strong urge to urinate, pelvic discomfort, and cloudy urine. UTIs can affect other parts too—if symptoms include back pain, fever, or vomiting, the infection may have spread to the kidneys.
Can you have a UTI without burning or pain when urinating?
Yes. Some people, particularly older adults and pregnant individuals, may not have classic symptoms like burning. Sometimes, the only sign is cloudy urine or a strong, persistent urge to urinate.
How are bladder infections and UTIs diagnosed?
Diagnosis generally relies on symptoms, urinalysis (to detect infection markers), and urine culture (to identify the bacteria). More severe or recurrent cases may require imaging or additional tests.
Are bladder infections dangerous?
Most bladder infections are not dangerous if treated promptly. However, left untreated, they can progress to kidney infections, which are more serious and may lead to complications like sepsis.
How do you prevent bladder infections and UTIs?
Maintain good hydration, urinate regularly, wipe front to back, and urinate after intercourse. Avoid unnecessary irritants and seek care for any recurrent or severe symptoms.
Key Takeaways
- Bladder infections are a common type of UTI but not all UTIs are bladder infections.
- Bladder infections usually cause localized urinary symptoms; more severe infections can involve kidneys and produce systemic symptoms.
- Prompt medical attention and treatment with antibiotics are vital for preventing complications.
- Prevention relies on good urinary habits, hygiene, and—as needed—medical care for those at higher risk.
If you suspect a UTI or bladder infection, consult your healthcare provider to confirm the diagnosis and start appropriate treatment.
References
- https://www.dispatchhealth.com/blog/uti-vs-bladder-infection-whats-the-difference/
- https://www.healthline.com/health/upper-uti-vs-lower-uti
- https://www.medicalnewstoday.com/articles/bladder-infection-vs-uti
- https://e-surgery.com/do-i-have-thrush-or-uti-how-to-tell-the-difference/
- https://tena.com.au/blogs/living-with-incontinence/bladder-infection
- https://www.txalz.org/blog/when-infection-mimics-progression-utis-in-alzheimers/
- https://www.medicalnewstoday.com/articles/189953
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5522788/
Read full bio of medha deb












