Managing Bladder and Bowel Issues in Advanced Prostate Cancer
Exploring how advanced prostate cancer and its treatments impact bladder and bowel health, plus management strategies for daily life.
Advanced prostate cancer frequently brings about changes in bladder and bowel function, disrupting daily comfort and impacting quality of life. These changes can arise from the cancer itself or as side effects of medical treatments. With understanding, proactive management, and strong communication with healthcare providers, many of these challenges can be addressed effectively.
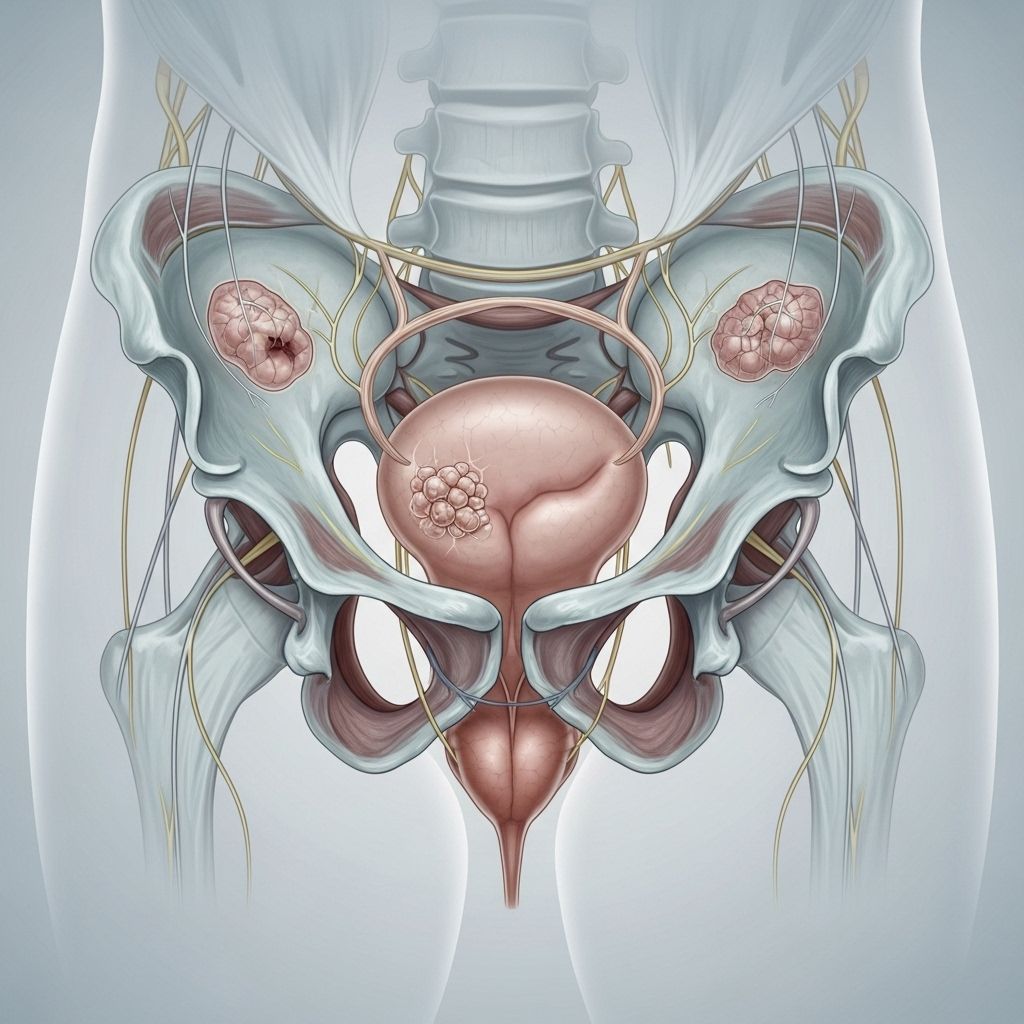
Understanding Prostate Cancer and Its Impact
The prostate gland is a crucial part of the male reproductive system. Located below the bladder and in front of the rectum, it encircles part of the urethra. As prostate cancer advances, it can extend beyond the gland to regions like lymph nodes, bones, or nearby organs, resulting in a spectrum of systemic symptoms—including disturbances of bladder and bowel function.
Types of Advanced Prostate Cancer
- Biochemical recurrence: Cancer returns as indicated by rising PSA (prostate-specific antigen) levels, but without visible metastasis.
- Castration-resistant prostate cancer (CRPC): Cancer continues to progress despite lowering testosterone levels.
- Non-metastatic castration-resistant prostate cancer (nmCRPC): Cancer does not show visible spread, but isn’t responsive to hormonal therapy.
- Metastatic prostate cancer: Cancer has spread to other parts of the body, such as bone or lymph nodes.
- Metastatic hormone-sensitive prostate cancer (mHSPC): Cancer has metastasized but can still respond to hormonal therapies.
- Metastatic castration-resistant prostate cancer (mCRPC): Cancer with distant spread that is no longer responsive to hormone therapy.
The stage and spread of prostate cancer strongly influence the likelihood and severity of bladder and bowel symptoms, as both the disease and its treatments may impact the pelvic region.
Bladder and Bowel Symptoms Caused by Cancer Itself
Bladder and bowel symptoms may develop due to the local advancement of prostate cancer, especially as the tumor grows and touches or invades adjacent organs.
Common Bladder Symptoms
- Difficulty starting urination
- Weak or interrupted urine flow
- Frequent urination, sometimes with an urgent need
- Trouble fully emptying the bladder
- Painful urination or a burning sensation
- Blood in the urine (hematuria)
Bladder symptoms are the most common urinary indicators and often arise when the expanding prostate puts pressure on or blocks the urethra, affecting urine flow. These symptoms can sometimes appear even before a prostate cancer diagnosis.
Common Bowel Symptoms
- Passing gas (flatulence)
- Diarrhea
- Constipation
- Sensation of incomplete bowel emptying
- Increased frequency or urgency to have a bowel movement
- Pain in the rectal area or abdomen
- Bowel blockage (rare)
- Rectal bleeding (rare)
Direct bowel symptoms tend to be less common because it’s rare for prostate cancer to invade the gastrointestinal (GI) tract. However, if the cancer does extend to the bowel or rectum, severe issues like pain, bleeding, and bowel obstruction may occur. Additionally, lifestyle changes, reduced physical activity, medication use, and changes in diet or hydration often associated with cancer can independently disrupt normal bowel habits and lead to constipation or diarrhea.
Bladder and Bowel Symptoms from Cancer Treatment
Treatments for advanced prostate cancer—particularly those targeted at the pelvis—can cause side effects that impact bowel and bladder health, both acutely and over the long term.
Radiation Therapy
Radiation (especially external beam radiation therapy or internal brachytherapy) is frequently aimed at the prostate and surrounding tissues. Because the rectum and bladder lie so close by, it’s common for these organs to be affected:
- Rectal pain or burning
- Diarrhea (sometimes with or without blood)
- Softer stools, and occasionally watery bowel movements
- Rectal leakage or urgency
- Bladder irritation—manifesting as increased urge and frequency
- Urinary urgency or incontinence
While most symptoms are mild and resolve weeks to months after therapy, some effects (especially from older forms of radiation) can last longer. Both the bladder and urethra are resistant to long-term radiation damage, so serious urinary leakage is rare.
Other Treatments and Their Effects
- Chemotherapy and hormonal therapy can occasionally cause diarrhea or bowel changes due to changes in metabolism or activity.
- Pain medications such as morphine and codeine are known to cause constipation. Do not discontinue prescribed medication, but inform your care team if bowel problems arise, as adjustments or additional medications might help.
- Reduced mobility, inadequate hydration, and dietary shifts due to treatment side effects may worsen or trigger new bladder or bowel problems.
How Are Symptoms Managed?
Many bladder and bowel symptoms are manageable. Early recognition and appropriate management can restore comfort and prevent complications. Treatment choices depend on the cause and severity of symptoms, and may be tailored to your specific situation.
Lifestyle and Dietary Adjustments
- Increase dietary fiber to ease constipation (e.g., fruits, vegetables, whole grains)
- Stay hydrated by drinking plenty of fluids—especially water
- Engage in regular gentle activity to stimulate bowel function
- Limit foods and drinks that irritate the bladder (like caffeine, alcohol, or spicy foods) if they exacerbate urinary symptoms
- If incontinence occurs, use absorbent pads or specialty continence products
Medical and Supportive Interventions
- Laxatives or stool softeners for constipation, tailored to individual needs
- Anti-diarrheal medications for severe diarrhea (under doctor supervision)
- Medications for bladder control, such as antimuscarinics
- Pelvic floor physical therapy to improve continence and muscle control
- If symptoms are severe or persistent, surgical interventions (rare, and only for significant blockages or structural changes)
Discussing any new or changing symptoms promptly with your doctor is critical. Many interventions are more effective if started early, and some symptoms can indicate more serious issues (e.g., metastatic spinal cord compression or bowel obstruction) that require immediate medical attention.
Communicating with Your Healthcare Team
Open, ongoing communication with your doctors, nurses, and other providers is essential in managing advanced prostate cancer symptoms:
- Track your symptoms and share detailed information about onset, frequency, severity, and any triggers that you notice.
- Maintain an open dialogue regarding any side effects or lifestyle changes, even if they feel minor or embarrassing. Healthcare teams are well versed in managing these issues.
- Ask about next steps if lifestyle or over-the-counter measures are not working.
- Seek support from counselors, dietitians, or support groups to help manage the emotional and practical aspects of symptoms.
Outlook and Quality of Life
While advanced prostate cancer is a serious condition, many bladder and bowel symptoms can improve with time, especially once effective management strategies are established. Some people find that their symptoms decrease after active treatment ends, while others continue to require ongoing adjustments and support.
Emotional challenges are common and entirely valid—struggles with incontinence, pain, or frequent trips to the bathroom can affect self-esteem, daily routines, and relationships. Open communication, both with medical providers and personal support networks, makes a meaningful difference.
Frequently Asked Questions (FAQ)
What are the most common bladder symptoms with advanced prostate cancer?
Difficulty starting urination, weak stream, increased frequency, urgency, painful urination, and sometimes blood in the urine are most frequently experienced.
Are bowel symptoms as common as bladder symptoms?
Bowel symptoms are less common, but when present may include constipation, diarrhea, discomfort, or rare cases of blockage or bleeding.
Can treatments for advanced prostate cancer cause permanent bladder or bowel problems?
Most symptoms from treatments like radiation usually resolve within weeks to months, but in rare cases (most often with older radiation methods), longer term effects may occur. Ongoing management with your healthcare provider minimizes risk.
What should I do if I experience sudden incontinence or am unable to empty my bowels?
Sudden loss of bladder or bowel control or inability to move bowels may signal a serious complication such as metastatic spinal cord compression or bowel obstruction. Promptly contact your healthcare provider or seek immediate medical attention.
How can lifestyle changes help with symptoms?
Maintaining healthy hydration, eating a balanced high-fiber diet, being as active as possible, and following medication guidance from healthcare providers can significantly improve both bladder and bowel symptoms.
Is it possible to improve quality of life despite these symptoms?
Yes. With the right mix of medical care, lifestyle adjustments, and emotional support, most people find ways to manage symptoms and maintain a meaningful quality of life.
Key Takeaways
- Advanced prostate cancer and its treatments can cause a variety of bladder and bowel problems.
- Symptoms often improve with timely management and supportive care.
- Diet, activity, and proactive symptom tracking are essential for optimal management.
- Open, honest communication with healthcare providers ensures you get the guidance and support needed to address these challenges.
References
- https://www.healthline.com/health/advanced-prostate-cancer/bladder-bowel-issues-prostate-cancer
- https://prostatecanceruk.org/prostate-information-and-support/advanced-prostate-cancer/managing-symptoms-in-advanced-prostate-cancer/
- https://www.iowauro.com/blog/10-signs-of-prostate-cancer-you-shouldnt-ignore
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8648407/
- https://www.cancerresearchuk.org/about-cancer/prostate-cancer/metastatic-cancer/symptoms
- https://www.basscancercenter.com/cancer-blog/prostate-troubles-when-to-worry-about-cancer
- https://www.mayoclinic.org/diseases-conditions/prostate-cancer/symptoms-causes/syc-20353087
- https://protons.com/treatments/prostate-cancer/signs-and-symptoms
Read full bio of Sneha Tete












