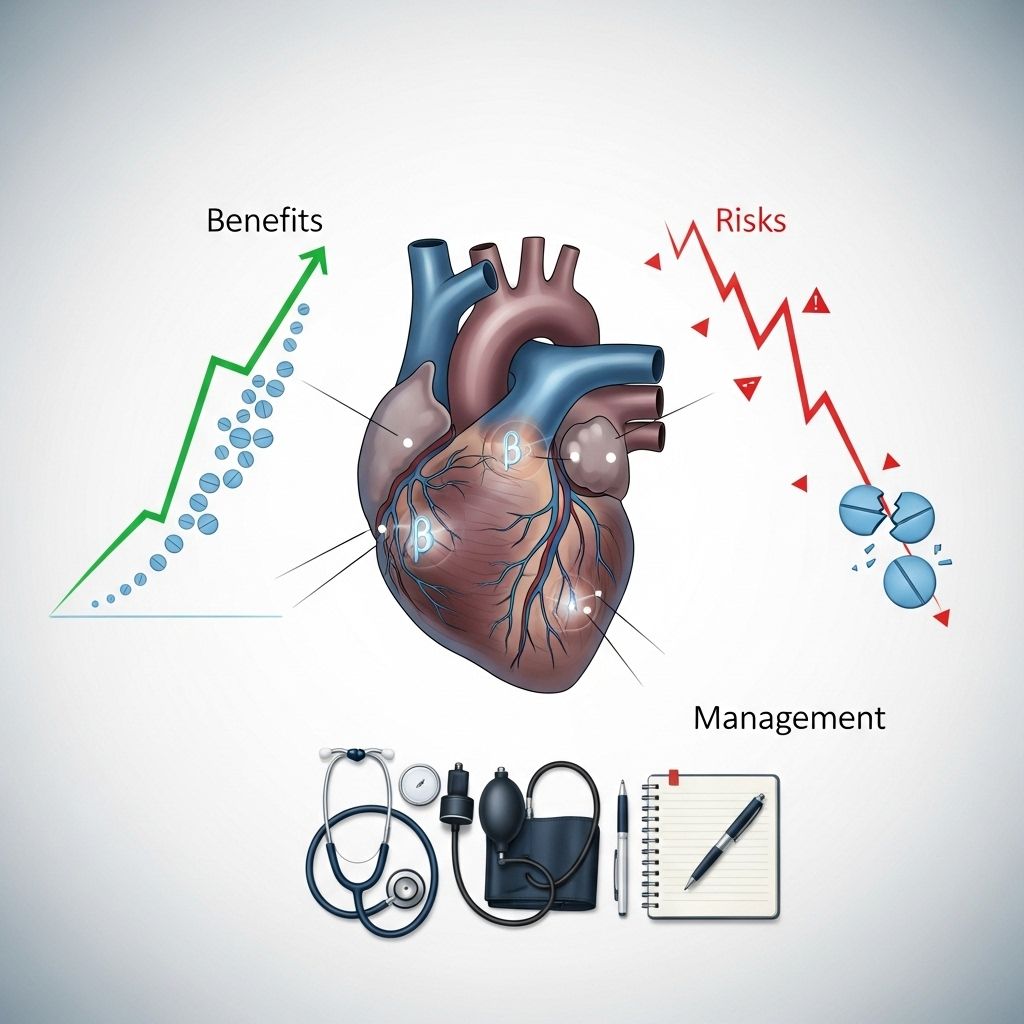
Beta-Blockers for Heart Failure: Essential Guide to Benefits, Risks, and Management
Understand how beta-blockers improve heart failure outcomes, their risks, dosing, and key management strategies for patients and caregivers.
Beta-Blockers for Heart Failure: Understanding Their Critical Role
Beta-blockers are a cornerstone in the management of heart failure, offering proven benefits in improving symptoms, reducing hospitalizations, and increasing survival rates. Once considered potentially dangerous in this population, their use is now supported by decades of research and clinical guideline recommendations.
What Are Beta-Blockers?
Beta-blockers are medications that block the effects of adrenaline (epinephrine) on the beta-adrenergic receptors of the heart and blood vessels. By doing so, they reduce heart rate, lower blood pressure, and decrease cardiac workload, making them crucial in a variety of heart conditions, including heart failure, hypertension, angina, and arrhythmias.
How Beta-Blockers Help in Heart Failure
- Improve Heart Function: Beta-blockers enhance the heart’s ability to relax and contract effectively over time, helping reverse some of the damage associated with heart failure.
- Reduce Harmful Stress Hormones: They inhibit the effects of substances like norepinephrine and epinephrine, which worsen heart failure if left unchecked.
- Lower Heart Rate: By slowing the heart rate, beta-blockers help the heart pump more efficiently with less strain.
- Decrease Hospitalizations and Mortality: Clinical trials consistently demonstrate reduced risk of death and emergency hospital admission among those on beta-blocker therapy.
Mechanism of Action
In heart failure, chronic stimulation of beta-adrenergic receptors leads to excess catecholamine release, damaging heart muscle over time. Beta-blockers block beta receptors, particularly β1 and β2, to dampen these effects. Certain agents also act on α1 or β3 receptors, contributing additional vasodilatory or protective effects.
Types of Beta-Blockers Used in Heart Failure
There are several beta-blockers, but only a few are specifically approved and recommended for heart failure with reduced ejection fraction (HFrEF):
- Bisoprolol (cardioselective)
- Carvedilol (nonselective with added alpha-blocking and vasodilation)
- Metoprolol succinate extended-release (cardioselective)
Other beta-blockers are used for hypertension, arrhythmias, and angina but do not have the same level of evidence for heart failure outcomes.
| Beta-Blocker | Receptor Selectivity | FDA Approval for Heart Failure? | Common Starting Dose | Target Dose |
|---|---|---|---|---|
| Bisoprolol | β1-selective | Yes | 1.25 mg once daily | 10 mg once daily |
| Carvedilol | Nonselective + α1-blocker | Yes | 3.125 mg twice daily | 25–50 mg twice daily |
| Metoprolol succinate ER | β1-selective | Yes | 12.5–25 mg once daily | 200 mg once daily |
Who Should Take Beta-Blockers for Heart Failure?
- All patients with HFrEF (ejection fraction <40%) should be considered for beta-blocker therapy, unless contraindicated or not tolerated.
- Initiation is recommended as soon as the diagnosis is established, even if symptoms are mild, absent, or improved by other drugs.
- Beta-blockers may not be suitable for those with severe bradycardia, low blood pressure, severe lung congestion, or certain forms of heart block.
Dosing and Administration
Beta-blockers should be started at a low dose and gradually increased every 1–2 weeks, as tolerated, to the target dose. The dose escalation (titration) process requires close monitoring for side effects and symptoms.
- Take as prescribed: Some may be taken with food, which can slow absorption but lessen side effects.
- Do not abruptly stop: Suddenly discontinuing beta-blockers can worsen heart failure.
- Monitor for changes: Watch for excessive fatigue, significant weight gain, swelling, or breathing difficulty during dose increases.
- Self-monitoring: Patients may be asked to check their pulse daily. Notify the doctor if the heart rate drops below recommended levels or blood pressure falls below 100 mmHg systolic.
Benefits of Beta-Blockers in Heart Failure
- Reduced mortality: Meta-analyses show up to a 30% reduction in death risk for heart failure patients.
- Lower hospitalization rates: Risk of emergency admissions drops by as much as 40%.
- Improved symptoms: Many experience fewer symptoms of breathlessness, fatigue, and edema.
- Enhanced left ventricular function: Restoration of healthier heart muscle function over time.
Potential Risks and Side Effects
Most side effects are temporary and mild, but patient monitoring is critical:
- Dizziness or lightheadedness, especially when standing up
- Tiredness and fatigue
- Cold hands and feet
- Headache
- Nightmares or trouble sleeping
- Heartburn, diarrhea, or constipation, gas
- Sudden weight gain: Call your doctor if you gain more than 3 pounds in one day or more than 5 pounds in one week
- Shortness of breath or wheezing
- Skin rash
- Irregular, slow, or fast heartbeat
- Swelling of feet or lower legs
- Chest pain
- Severe vomiting or diarrhea: Can cause dehydration and low blood pressure
If side effects do not resolve, or cause significant concern, communicate promptly with your healthcare provider.
Precautions and Drug Interactions
- Other medications: Beta-blockers are commonly prescribed alongside diuretics, ACE inhibitors, or digoxin. Share all medications with your healthcare provider to avoid interactions.
- Lung conditions: Severe asthma or chronic obstructive pulmonary disease (COPD) may be aggravated.
- Diabetes: Beta-blockers may mask symptoms of low blood sugar; monitor glucose closely.
- Thyroid disorders: Thyroid medications can interact, altering effectiveness.
Practical Tips for Patients on Beta-Blockers
- Follow your prescribed dosing schedule consistently.
- Monitor weight, pulse, and symptoms daily, as directed.
- Report concerning side effects or symptoms immediately.
- Attend regular follow-up appointments for medication review and heart function assessment.
- Discuss any plans for changing, skipping, or stopping medication with your healthcare provider.
Frequently Asked Questions (FAQs)
Q: What makes beta-blockers essential in heart failure treatment?
A: Beta-blockers are among the few medications proven to improve survival and reduce hospitalizations in heart failure. They are recommended by leading heart health organizations for nearly all patients with HFrEF, unless contraindicated.
Q: Which beta-blockers are approved for heart failure?
A: The three main FDA-approved agents are bisoprolol, carvedilol, and metoprolol succinate extended-release.
Q: Can I stop taking my beta-blocker if I feel better?
A: Never discontinue beta-blockers suddenly. Stopping abruptly can worsen heart failure and increase risk of serious complications. Always talk to your doctor before making any changes.
Q: What should I do if I experience side effects?
A: Report persistent, severe, or concerning side effects to your healthcare provider. Some symptoms may resolve as your body adjusts, but others may require attention or dose adjustment.
Q: Are there people who should not take beta-blockers?
A: Beta-blockers are generally safe and effective, but certain conditions—like severe lung disease, very slow heart rate (bradycardia), heart block, or very low blood pressure—may make them inappropriate. Your doctor will evaluate your specific risks and benefits.
Q: How do beta-blockers differ from other heart failure medications?
A: Unlike most drugs that lower blood pressure or fluid overload, beta-blockers directly counteract harmful stress hormones and help restore healthier heart rhythms and muscle function, providing unique benefits in reversing heart failure progression.
Key Takeaways
- Beta-blockers are recommended for nearly all patients with heart failure based on robust evidence of benefit.
- The three main agents—bisoprolol, carvedilol, and metoprolol succinate ER—are proven to reduce risk and improve outcomes.
- Start with low doses and increase slowly under medical supervision, monitoring for side effects carefully.
- Report any persistent symptoms, weight changes, or other health concerns to your healthcare provider immediately.
References & Further Reading
- American Heart Association / American College of Cardiology Guidelines: 2022 Heart Failure Management
- WebMD: Beta-Blockers for Heart Failure
- JAMA Network: β-Blocker Therapy in Heart Failure
- The Cardiology Advisor: Beta Blockers in Heart Failure Management
References
- https://www.thecardiologyadvisor.com/features/beta-blockers-in-heart-failure/
- https://jamanetwork.com/journals/jama/fullarticle/194661
- https://www.webmd.com/heart-disease/heart-failure/heart-failure-beta-blocker
- https://www.ncbi.nlm.nih.gov/books/NBK532906/
- https://www.aafp.org/pubs/afp/issues/2000/1201/p2453.html
- https://my.clevelandclinic.org/health/treatments/22318-beta-blockers
- https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/beta-blockers/art-20044522
- https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2023.1263482/full
Read full bio of medha deb












