Benign Prostatic Hyperplasia (BPH): Symptoms, Causes, and Treatments
Understanding BPH is essential for managing urinary symptoms and improving quality of life as men age.
Overview
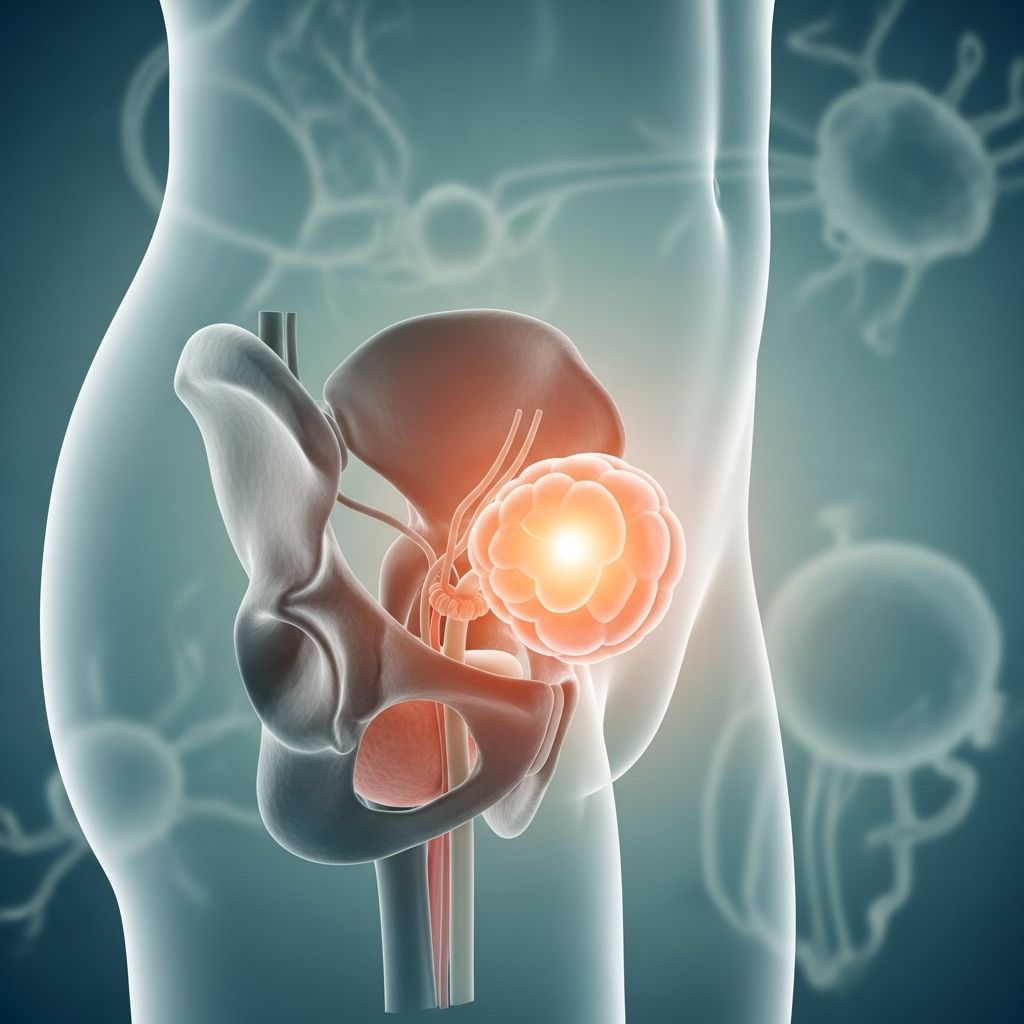
Benign prostatic hyperplasia (BPH), also known as an enlarged prostate, is a common health issue that primarily affects men as they age. The prostate, a small gland located just below the bladder, plays a vital role in male reproductive health by helping to produce semen. As men grow older, the prostate often increases in size.
This enlargement can lead to blockage of urine flow from the bladder, causing bothersome urinary symptoms and, if untreated, potentially leading to problems affecting the bladder, urinary tract, or kidneys. Fortunately, a range of treatments—including medications, lifestyle modifications, and surgical procedures—are available to help manage BPH and improve quality of life.
Symptoms
The symptoms of BPH often develop slowly and may vary in severity. Not every man experiences all symptoms, and the size of the prostate does not always match the level of discomfort.
- Frequent or urgent need to urinate
- Increased frequency of urination at night (nocturia)
- Difficulty starting urination
- Weak urine stream or a stream that stops and starts
- Dribbling at the end of urination
- Incomplete emptying of the bladder
Sometimes, less common symptoms may occur, such as:
- Urinary tract infections
- Inability to urinate (urinary retention)
- Blood in the urine (hematuria)
How Symptoms Can Impact Daily Life
Many men find BPH symptoms—especially urgency, frequency, and nocturia—disruptive. Some may find sleep interrupted, while others plan trips around restroom availability. Persistent symptoms can significantly affect daily routines, comfort, and psychological wellbeing.
When to See a Doctor
It’s important to consult a healthcare provider if you experience urinary symptoms that:
- Are uncomfortable or bothersome
- Interfere with daily activities
- Cause anxiety about urinary health
Immediate medical attention is warranted if you:
- Cannot urinate at all
- Notice blood in your urine
- Develop pain or discomfort in the lower abdomen or urinary tract
Causes
BPH is not cancerous and its development is attributed to multiple factors, most of which are believed to be age-related and influenced by hormonal changes.
- Hormonal changes with age: The exact mechanism is unclear, but hormonal shifts, particularly in testosterone and estrogen levels, are suspected contributors.
- Cellular changes: As men get older, the balance of cell growth and cell death changes, resulting in increased prostate tissue.
Other causes, such as chronic inflammation and familial tendencies, may also play a role, but are less clearly defined.
Risk Factors
Certain factors increase the likelihood of developing BPH, including:
- Advancing age (especially after age 40, risk increases significantly)
- Family history of prostate problems
- Medical conditions such as diabetes and heart disease
- Obesity and sedentary lifestyle
- Lack of physical activity
- Ethnic background: Some populations have higher rates of BPH
Complications
If left untreated, BPH can give rise to several complications. Although most men with BPH do not experience severe complications, the risk increases as symptoms progress.
- Sudden inability to urinate (acute urinary retention)
- Urinary tract infections (UTIs): Inability to empty the bladder fully can contribute to infections.
- Bladder stones: These can form due to incomplete emptying of the bladder.
- Bladder damage: Chronic retention can weaken and stretch bladder muscles.
- Kidney damage: Pressure from a full bladder can affect kidney function.
Serious complications are uncommon with appropriate treatment. Nonetheless, procrastinating medical evaluation may heighten risks.
Prevention
There is no proven way to prevent BPH, but some strategies may help reduce risk and ease symptoms:
- Maintaining a healthy weight
- Staying physically active
- Adopting a balanced diet
- Managing underlying chronic illnesses
Regular check-ups with your healthcare provider can help in early detection and timely management.
Lifestyle Modifications for Symptom Relief
Initial management of BPH symptoms often includes lifestyle and behavioral changes, which can reduce symptom severity and improve quality of life:
- Reducing intake of fluids—especially before bedtime
- Limiting beverages with caffeine and alcohol, which can increase urine production
- Practicing double voiding—urinating, then waiting a few moments and trying again
- Avoiding medications that can worsen symptoms, such as some antihistamines or decongestants (under physician guidance)
- Regular physical activity to maintain bladder function
Treatment Options
Treatment is tailored to each individual’s symptoms, prostate size, age, overall health, and personal preferences. The main categories of treatment include:
1. Medications
- Alpha blockers: Relax prostate and bladder neck muscles to improve urine flow
- 5-alpha reductase inhibitors: Shrink the prostate by affecting hormone levels
- Combination therapies: Use both medications above for greater effectiveness
2. Minimally Invasive or Surgical Procedures
These interventions are considered when medications and lifestyle changes are not effective:
- Transurethral resection of the prostate (TURP): Surgical removal of prostate tissue via the urethra
- Laser therapy: Use of focused light to cut or shrink prostate tissue
- Prostatic urethral lift (PUL): Mechanical lifting of the prostate to relieve pressure on the urethra
- Water vapor or Aquablation therapies: Newer treatments leveraging water to ablate tissue with lower risk of sexual side effects
- Simple prostatectomy: Reserved for very large prostates
Newer Treatment Developments
Innovations such as Aquablation use high-pressure water to remove excess prostate tissue, offering benefits like decreased risk of incontinence and sexual side effects compared to other procedures. These are particularly valuable for larger prostates and patients with higher surgical risks.
Table: Comparison of Common BPH Treatments
| Treatment | How It Works | Main Benefits | Main Risks/Side Effects |
|---|---|---|---|
| Alpha blockers | Relax muscles in prostate/bladder neck | Quick symptom relief | Dizziness, fatigue |
| 5-alpha reductase inhibitors | Shrink prostate by altering hormones | Long-term size reduction | Reduced libido, erectile dysfunction |
| TURP | Removes obstructive tissue through urethra | Effective for moderate to severe symptoms | Bleeding, retrograde ejaculation |
| Laser therapy | Uses light to cut or remove tissue | Less bleeding, faster recovery | Temporary irritation |
| Prostatic urethral lift (PUL) | Lifts and holds enlarged prostate tissue | Minimally invasive, preserves sexual function | Mild discomfort, irritation |
| Aquablation | Waterjet ablation of tissue | Fewer sexual side effects, precise | Short-term catheter, rare complications |
Healthcare Costs and Considerations
BPH is not only a clinical challenge but also has economic impacts. Annual individual healthcare costs for BPH treatments can exceed $1,500, with national costs reaching billions. The choice of procedure can have significant implications for cost, recovery, and long-term outcomes. Discuss with your healthcare provider about the most cost-effective and beneficial option for your condition.
Frequently Asked Questions (FAQ)
Q: Is BPH the same as prostate cancer?
A: No, BPH is a non-cancerous enlargement of the prostate and does not increase the risk for prostate cancer. However, both conditions may coexist and require different management approaches.
Q: Can BPH be cured?
A: BPH is a chronic condition, but symptoms can be managed successfully with lifestyle changes, medication, or procedures. Most men find significant relief with appropriate treatment.
Q: Are there any natural remedies for BPH?
A: Some supplements are marketed for prostate health, but scientific evidence supporting their effectiveness is limited. Always consult your physician before trying herbal or non-prescription remedies.
Q: What lifestyle changes help reduce BPH symptoms?
A: Reducing caffeine/alcohol, limiting evening fluids, regular exercise, and practicing double voiding can ease symptoms. Avoid bladder irritants and consult your doctor for medications that may exacerbate issues.
Q: What if I suddenly can’t urinate?
A: Acute urinary retention is a medical emergency. Seek immediate care if you are unable to pass urine, as it may require prompt intervention to prevent complications.
Key Takeaways
- BPH is common as men age, and can significantly impact quality of life.
- A range of treatments, from lifestyle changes to advanced minimally invasive therapies, are available and highly effective.
- Prompt recognition and management can prevent complications such as urinary retention and infection.
- Discuss treatment options, risks, and benefits with your healthcare provider to make informed decisions tailored to your specific needs.
References
- Original content based on Mayo Clinic and related professional resources on BPH.
References
- https://www.mayoclinic.org/medical-professionals/urology/news/new-bph-treatment-ablates-the-prostatic-tissue-without-heat/mac-20573532
- https://www.mayoclinic.org/medical-professionals/urology/news/healthcare-costs-associated-with-benign-prostatic-hyperplasia/mac-20560056
- https://www.mayoclinic.org/diseases-conditions/benign-prostatic-hyperplasia/symptoms-causes/syc-20370087
- https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-can-lifestyle-changes-help-with-enlarged-prostate/
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/treatment-for-enlarged-prostate
Read full bio of Sneha Tete












