B-Cell Acute Lymphoblastic Leukemia: Understanding Causes, Symptoms, and Treatments
Comprehensive guide to B-cell acute lymphoblastic leukemia—covering symptoms, diagnosis, treatment, prognosis, and frequently asked questions for patients and caregivers.
B-Cell Acute Lymphoblastic Leukemia (B-Cell ALL): An In-Depth Guide
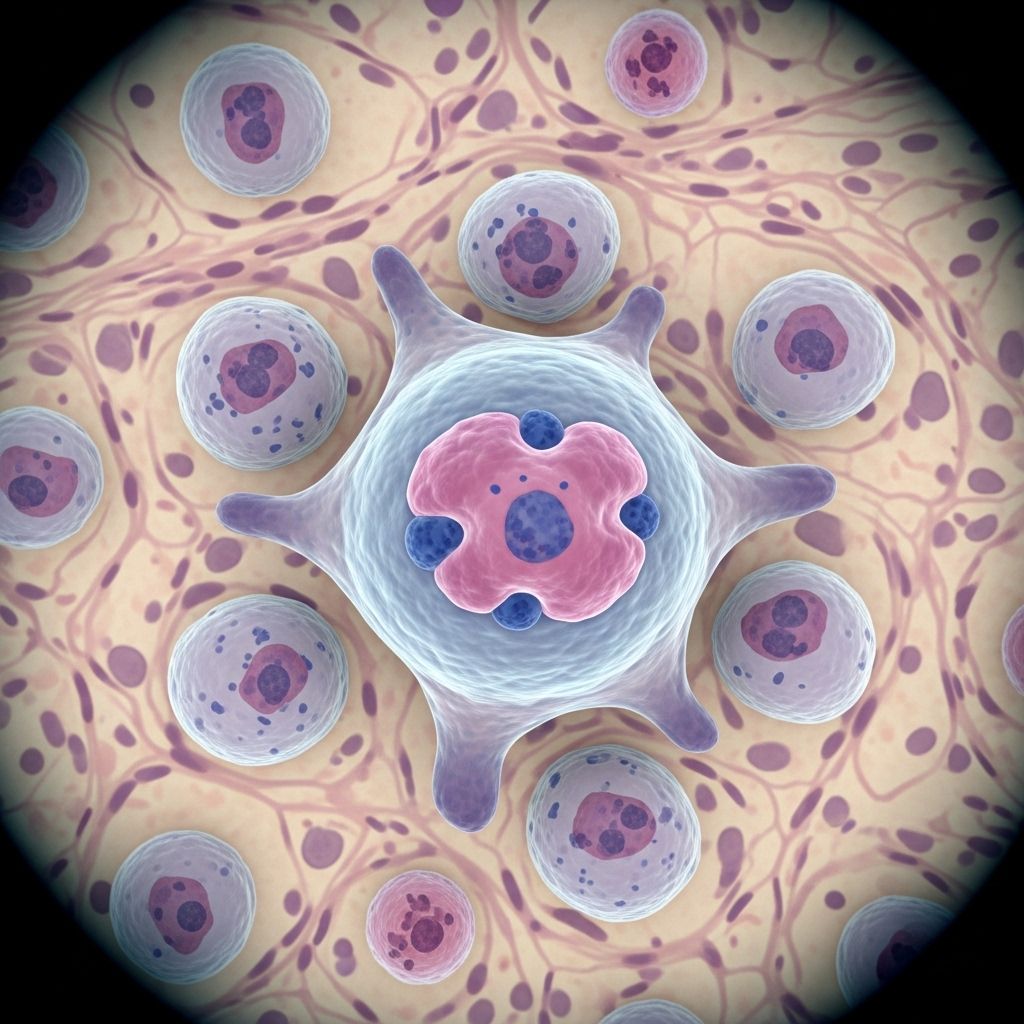
B-cell acute lymphoblastic leukemia (B-cell ALL) is a serious and rapidly progressing cancer of the blood and bone marrow that predominantly affects B lymphocytes—a type of white blood cell responsible for producing antibodies and fighting infection. Its swift onset and need for urgent treatment make it essential to understand the condition’s origins, risk factors, signs, diagnostic procedures, available therapies, and expected outcomes.
What Is B-Cell ALL?
B-cell acute lymphoblastic leukemia (ALL) begins in the bone marrow, where immature B lymphocytes (also known as B cells) multiply abnormally and crowd out normal cells. This disrupts the balance of blood components and impairs the body’s ability to fight infection, transport oxygen, and prevent bleeding. ALL is different from chronic leukemia, as it develops quickly and requires prompt medical treatment.
Acute lymphoblastic leukemia is the most common type of leukemia in children, but it can also affect adults. About 75% of adult ALL cases are of the B-cell variety. T-cell ALL accounts for the remaining 25% of cases.
How Blood Cells Are Made—and What Goes Wrong in ALL
- Bone marrow produces blood stem cells, which mature into different types of cells:
- Lymphoid stem cells → lymphocytes (B cells and T cells)
- Myeloid stem cells → red blood cells, platelets, granulocytes, and monocytes
In B-cell ALL, the bone marrow creates excessive numbers of immature B lymphocytes called blast cells. These cells multiply and accumulate in the marrow and bloodstream, outnumbering healthy blood cells and leading to symptoms like anemia, infection susceptibility, and bleeding tendencies.
Causes and Risk Factors
The exact causes of B-cell ALL remain unknown in most cases. However, several risk factors may increase susceptibility:
- Genetic mutations: Changes in the DNA of developing lymphocytes may drive leukemia.
- Family history: Those with relatives who have had leukemia may have a higher risk.
- Previous cancer treatments: Chemotherapy or radiation therapy for other cancers can increase risk later in life.
- Inherited conditions: Disorders like Down syndrome, neurofibromatosis, and certain rare genetic diseases raise leukemia risk.
- Exposure to radiation: High levels of radiation from environmental sources or medical treatment.
Most cases, especially in children, occur without identifiable causes.
Signs and Symptoms
B-cell ALL often develops in a matter of days or weeks. Symptoms result from the lack of healthy blood cells and the infiltration of abnormal cells into organs. Common signs include:
- Fatigue due to anemia (low red blood cells)
- Fever from infections (low healthy white blood cells)
- Easy bruising or bleeding (low platelets)
- Paleness of the skin
- Swollen lymph nodes
- Abdominal discomfort due to enlarged liver or spleen
- Bone pain
- Recurrent infections
- Night sweats and unexplained weight loss
- Shortness of breath
ALL can also spread beyond the bone marrow to the brain, spinal cord, testicles (in males), and other organs, potentially causing neurological symptoms (like headaches or confusion) or testicular swelling.
Types and Subgroups of ALL
Doctors classify acute lymphoblastic leukemia into types and subgroups based on features of the malignant cells.
- B-cell ALL: Most common in adults and children; further classified by the stage of B cell development affected. The most common subgroup is precursor B-cell ALL.
- T-cell ALL: More frequent in adolescent males and young adults; involves precursor T cell lymphocytes.
Determining the specific subtype of ALL is crucial for tailoring treatment and understanding prognosis.
Diagnosing B-Cell ALL
Diagnosis typically involves several steps and tests:
- Physical examination: Assessment of symptoms and signs such as swollen lymph nodes, pallor, or enlarged liver/spleen.
- Blood tests: Complete blood count reveals abnormal levels of red blood cells, white blood cells, and platelets.
- Bone marrow biopsy: A sample from the hip bone or another site is examined to identify leukemic cells.
- Flow cytometry: Laboratory technique used to classify leukemia cells by their surface markers.
- Cytogenetic analysis: Identifies chromosome changes or gene mutations associated with leukemia.
- Lumbar puncture: Cerebrospinal fluid testing to determine whether leukemia has spread to the brain or spinal cord.
- Imaging studies: CT scans and ultrasounds assess organ involvement (liver, spleen, lymph nodes).
Diagnosis may also include second opinions before finalizing a treatment plan.
Treatment Options for B-Cell ALL
Treatment for B-cell ALL aims to eradicate leukemic cells, restore normal blood counts, and prevent relapse. The journey typically unfolds in several phases:
- Induction therapy: The first stage, using strong chemotherapy drugs to prompt initial remission (elimination of abnormal cells).
- Consolidation/intensification therapy: Additional chemotherapy given to destroy residual leukemic cells.
- Maintenance therapy: Lower-dose, long-term therapy (often lasting months to years) to reduce the risk of recurrence.
- Central nervous system prophylaxis: Prevents or treats spread of leukemia to the brain or spinal cord, often using chemotherapy injected during a lumbar puncture.
- Targeted therapies: Drugs such as tyrosine kinase inhibitors or monoclonal antibodies that attack specific features of leukemia cells.
- Immunotherapy: Treatments that mobilize the immune system against leukemia cells (e.g., CAR T-cell therapy).
- Stem cell transplantation: Replacement of diseased bone marrow with healthy donor stem cells, considered for high-risk or relapsed patients.
Pediatric protocols differ from adult protocols, with children generally achieving higher cure rates. Treatment plans are highly individualized based on age, leukemia subtype, genetic mutations, prior health, and the response to initial therapy.
Side Effects of Treatment
- Fatigue
- Increased risk of infection
- Nausea and vomiting
- Hair loss
- Easy bruising
- Mouth sores
- Organ toxicity
Managing side effects is a critical part of supportive care during and after treatment.
Prognosis and Survival for B-Cell ALL
Outcomes depend on several factors, notably age at diagnosis, the presence of genetic abnormalities, initial response to therapy, and overall health. In children with B-cell ALL, survival rates exceed 90% with modern therapy. Adults often have lower survival rates due to different disease biology and more challenging treatments, but advances in targeted therapies are improving outcomes.
Some patients—especially adults—may experience relapse, necessitating further chemotherapy, targeted therapy, or stem cell transplant. Long-term monitoring remains essential even after remission.
Living With B-Cell ALL
The diagnosis and treatment of B-cell ALL impact every aspect of life—physical, emotional, and psychosocial. Patients and families should be aware of resources and strategies for support:
- Infection control: During treatment, patients must avoid contagious illnesses and sick contacts due to immunosuppression.
- Follow-up appointments: Essential for monitoring remission, managing side effects, and checking for recurrence.
- Psychological support: Counseling, support groups, and educational resources help cope with anxiety, depression, and family stress.
- Healthy lifestyle: Balanced nutrition, adequate sleep, and gentle physical activity (as tolerated) aid recovery.
- Financial and social support: Assistance programs can help with treatment costs and practical needs.
B-Cell ALL in Children vs. Adults
| Feature | Children | Adults |
|---|---|---|
| Incidence | Most common childhood leukemia | Rare, but more aggressive; poorer prognosis |
| Survival Rate | Over 90% | Lower (varies, improving with new therapies) |
| Treatment | More intensive, longer duration; generally better tolerated | May involve stem cell transplant, more toxicity |
| Relapse Risk | Lower | Higher |
Frequently Asked Questions (FAQs)
Q1: What is the difference between B-cell and T-cell ALL?
A: B-cell ALL involves immature B lymphocytes, which produce antibodies. T-cell ALL involves immature T lymphocytes, which help regulate the immune response. Treatment varies slightly in each due to biological differences.
Q2: Is B-cell ALL curable?
A: Over 90% of children are cured of B-cell ALL with current treatments. Adults have lower cure rates but newer therapies (immunotherapy, targeted drugs, stem cell transplant) are improving outcomes.
Q3: How does B-cell ALL affect daily life?
A: Fatigue, increased risk of infections, and bleeding are common. Chemotherapy and other treatments mean frequent medical visits and side effects, requiring support and lifestyle adjustments.
Q4: Can B-cell ALL return after remission?
A: Relapse is possible, especially in adults or in cases with high-risk genetic features. Close monitoring and additional therapy may be needed in such cases.
Q5: What should families and caregivers know?
A: Emotional support, infection control measures, adherence to treatment schedules, and access to reliable resources and health professionals are vital for successful management.
When to Seek Help
- Persistent fatigue, unexplained bruises, prolonged fever, or frequent infections should prompt prompt medical evaluation.
- New neurological symptoms (headaches, weakness, confusion) in someone with ALL may signify a spread to the brain—seek urgent medical care.
- Adhere closely to scheduled follow-up and treatment appointments.
Key Takeaways
- B-cell ALL is a rapid-onset cancer affecting B lymphocytes in the bone marrow.
- Early diagnosis and individualized treatment plans offer the best outcomes.
- Children have excellent prognosis; outcomes for adults are improving.
- Lifelong follow-up may be necessary due to risk of relapse or late effects of therapy.
References
- https://www.cancer.gov/types/leukemia/patient/adult-all-treatment-pdq
- https://www.ncbi.nlm.nih.gov/books/NBK459149/
- https://www.cancerresearchuk.org/about-cancer/acute-lymphoblastic-leukaemia-all/about
- https://www.webmd.com/cancer/lymphoma/b-cell-acute-lymphoblastic-leukemia-children
- https://cancer.osu.edu/for-patients-and-caregivers/learn-about-cancers-and-treatments/cancers-conditions-and-treatment/cancer-types/blood-cancers/leukemia/b-cell-acute-lymphoblastic-leukemia
- https://www.mayoclinic.org/diseases-conditions/acute-lymphocytic-leukemia/symptoms-causes/syc-20369077
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5520400/
- https://my.clevelandclinic.org/health/diseases/21564-acute-lymphocytic-leukemia
Read full bio of medha deb












