Atrial Flutter: Causes, Symptoms, Diagnosis, and Treatment Options
Understand atrial flutter: from its causes to symptoms, diagnosis, risks, and current treatment strategies for optimal heart health.
Atrial Flutter: An Overview
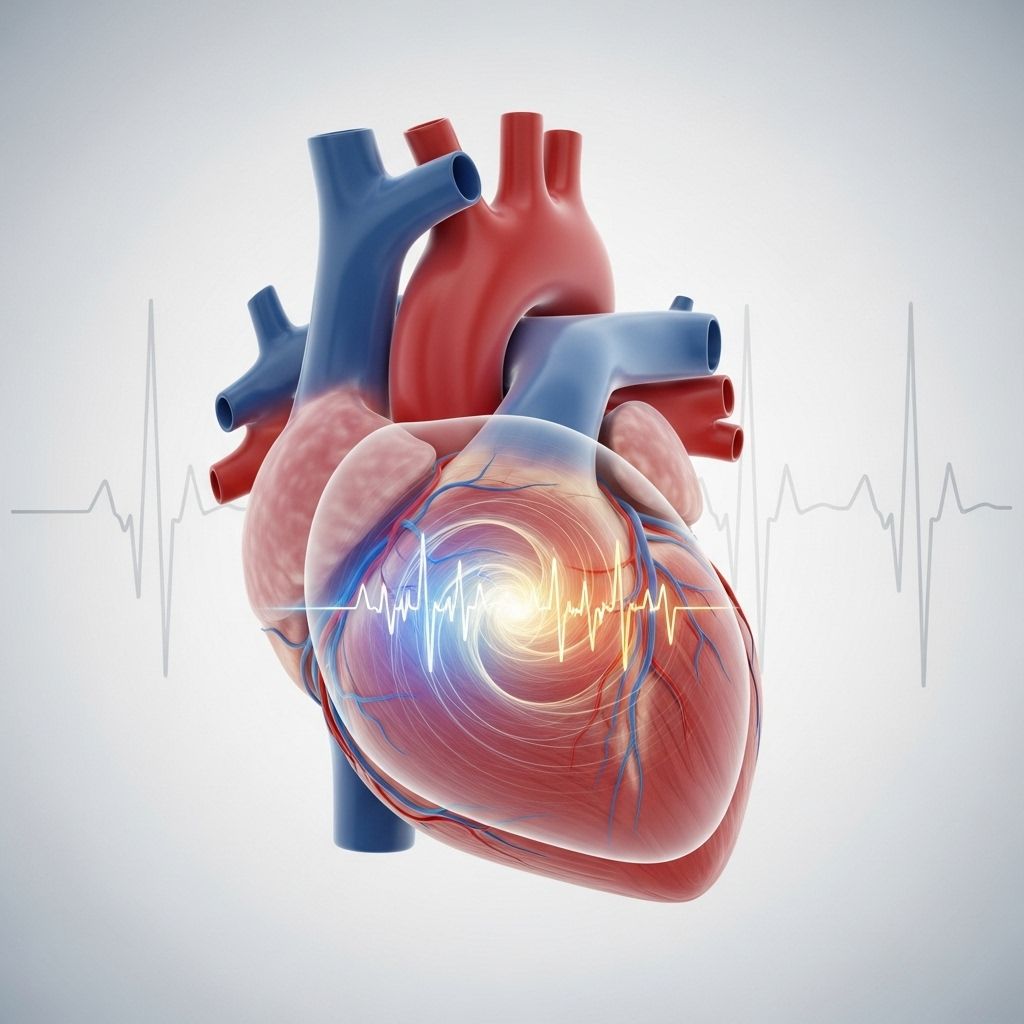
Atrial flutter is a common abnormal heart rhythm, classified as an arrhythmia. This disturbance in the normal heart rhythm causes the upper chambers of the heart—known as the atria—to beat much faster than normal, typically between 250 and 350 beats per minute. While the beats are typically coordinated, unlike in atrial fibrillation, they are excessively rapid, which can lead to serious health concerns including stroke and heart failure.
Understanding the causes, symptoms, risks, and current management options is key to maintaining heart health and preventing complications.
What is Atrial Flutter?
Atrial flutter is a type of supraventricular tachycardia—a condition where the heart’s upper chambers beat rapidly due to disorganized electrical circuits. In most cases, this rhythm originates as a large circuit in the right atrium, often traveling around the tricuspid valve. There are two main types:
- Typical atrial flutter: Originates from a circuit around the tricuspid valve in the right atrium.
- Atypical atrial flutter: Arises from circuits elsewhere in the right or left atrium.
The rapid firing disrupts the normal flow of blood through the heart, and it may occur in both people with and without prior heart disease, although scarring from prior cardiac events or surgery can increase risk.
Episodes may last seconds to hours, or become persistent, and some patients may transition between atrial flutter and atrial fibrillation.
How Atrial Flutter Differs from Other Arrhythmias
| Feature | Atrial Flutter | Atrial Fibrillation | Multifocal Atrial Tachycardia |
|---|---|---|---|
| Rhythm | Fast, regular, organized | Irregular, disorganized | Irregular, multiple P wave shapes |
| Atrial Rate | 250–350 bpm | 400–600 bpm | Variable |
| ECG Findings | Sawtooth flutter waves | No distinct P waves | P waves of varying morphology |
What Causes Atrial Flutter?
The exact cause of atrial flutter is sometimes unknown. However, risk factors and contributing conditions include:
- Prior heart surgery or damage (scarring of the atria)
- High blood pressure
- Coronary artery disease
- Heart failure
- Valve disorders (especially mitral valve disease)
- Chronic lung disease
- Hyperthyroidism (overactive thyroid)
- Alcohol use or stimulants
- Advanced age
In some cases, atrial flutter may occur without any identifiable heart problem.
Symptoms of Atrial Flutter
Symptoms vary according to how rapid the heart beats and the overall health of the patient. Some individuals may be completely asymptomatic, but common signs of atrial flutter include:
- Palpitations (feeling of fluttering or pounding in the chest)
- Rapid heartbeat
- Chest pain or discomfort
- Shortness of breath
- Lightheadedness or dizziness
- Fatigue (especially on exertion)
- Low blood pressure
- Faintness or confusion
- Sweating
- Anxiety
Episodes can sometimes be triggered by exertion or stress. The rapid heart rate associated with untreated atrial flutter—often up to 150 beats per minute—can put significant strain on the heart and is potentially dangerous. Immediate medical attention is necessary for persistent symptoms, chest pain, severe shortness of breath, or fainting.
How is Atrial Flutter Diagnosed?
Diagnosis typically starts with a healthcare provider evaluating the patient’s medical history and symptoms. The following diagnostic tools are commonly used:
- Electrocardiogram (ECG/EKG): The primary diagnostic tool; shows classic sawtooth patterns associated with atrial flutter.
- Holter Monitor: Portable device worn for 24 hours or longer to record intermittent arrhythmias.
- Event Monitor: Used for symptoms occurring less frequently; can be worn for up to 30 days.
- Echocardiogram: Ultrasound of the heart to evaluate structure, function, and look for blood clots.
- Blood tests: To rule out contributing conditions such as thyroid dysfunction.
Risks and Potential Complications
While atrial flutter itself is not always life-threatening, it can lead to serious complications if left untreated, including:
- Stroke: Blood clots can form due to slowed blood movement in the atria, increasing stroke risk.
- Heart failure: Sustained rapid heart rate may weaken the heart muscle over time.
- Cardiomyopathy: Damage to the heart muscle caused by continued rapid rate.
- Hemodynamic instability: Reduced blood pressure, fainting, or organ dysfunction due to poor cardiac output.
The decision to use anticoagulation (blood thinners) depends on individual risk factors, including previous history of stroke, heart failure, mitral valve disease, coronary artery disease, high blood pressure, and age. Patients and physicians work together to evaluate the risk and benefit of blood thinners such as warfarin or direct oral anticoagulants.
How is Atrial Flutter Treated?
Treatment aims to restore a normal heart rhythm, prevent stroke, and manage symptoms. Approaches vary based on patient history, overall health, symptom severity, and underlying causes.
Medications
- Rate control: Beta-blockers, calcium channel blockers, or digoxin can slow ventricular response.
- Rhythm control: Antiarrhythmic drugs such as dofetilide, sotalol, or amiodarone attempt to restore normal rhythm.
- Anticoagulation: Warfarin or direct oral anticoagulants (DOACs) are prescribed to reduce stroke risk when indicated.
Electrical Cardioversion
A brief, controlled electrical shock is delivered under sedation to reset the heart rhythm to normal. This is often considered if medications are ineffective or if there is no evidence of blood clot in the atria.
Catheter Ablation
- Radiofrequency catheter ablation: The most effective curative therapy for typical atrial flutter, using heat energy to destroy the abnormal circuit in the right atrium.
- Success Rate: Approximately 95% for typical atrial flutter, with very low recurrence and complication rates.
- Considered first-line for: Patients who cannot tolerate medications or have persistent symptoms despite therapy.
- Pacemaker: In rare cases, when medications and ablation fail, a pacemaker may be needed after atrioventricular nodal ablation to control heart rhythm.
Lifestyle Changes and Monitoring
- Managing underlying disorders: Controlling high blood pressure, coronary artery disease, diabetes, or thyroid dysfunction.
- Limiting stimulants: Avoid excess caffeine, alcohol, and recreational drugs.
- Regular medical checkups and monitoring for symptoms or complications.
Prognosis and Long-Term Outlook
The prognosis for patients with atrial flutter is generally very good—especially in those treated with catheter ablation, as recurrence rates are less than 5%. However, persistent atrial flutter may cause tachycardia-induced cardiomyopathy, leading to heart failure, recurrent hospitalizations, and reduced quality of life. The risk of stroke remains a priority throughout management.
With proper treatment and monitoring, many individuals lead full and active lives. However, some may experience recurrent episodes or transition to other arrhythmias, such as atrial fibrillation, which may require additional management.
Frequently Asked Questions (FAQs)
Q: Can atrial flutter convert to atrial fibrillation?
A: Yes. Many patients with atrial flutter may also develop episodes of atrial fibrillation. Both arrhythmias often share similar triggers and risk factors.
Q: Is atrial flutter dangerous?
A: Atrial flutter itself is not always immediately life-threatening, but if untreated, the rapid heart rate and increased stroke risk make it a potentially serious condition requiring medical attention.
Q: Will I need blood thinners if I have atrial flutter?
A: Many patients require blood thinners to reduce the risk of blood clots and stroke, but the need depends on individual risk factors. Your doctor will help guide this decision.
Q: What is catheter ablation, and is it safe?
A: Catheter ablation uses radiofrequency energy to destroy the abnormal electrical circuit causing atrial flutter. It is safe, with high success rates and low risk of complications, especially for right-sided atrial flutter.
Q: Can lifestyle changes help prevent episodes?
A: Yes. Managing underlying health conditions, taking medications as prescribed, and avoiding excessive stimulants (alcohol, caffeine, drugs) may reduce the risk of recurrent episodes.
Q: Should I call 911 if I have chest pain with atrial flutter?
A: Yes. If you ever experience severe chest pain, shortness of breath, fainting, or confusion along with atrial flutter, seek emergency medical care immediately.
Key Takeaways for Patients and Caregivers
- Atrial flutter is a common heart arrhythmia characterized by rapid and regular atrial beats.
- Symptoms can range from none to severe palpitations and chest pain; it may cause complications like stroke and heart failure.
- Diagnosis relies on ECG, and long-term monitoring may be needed.
- Treatment includes medications, electrical cardioversion, and curative catheter ablation.
- Prognosis is generally good after ablation, but monitoring and stroke prevention remain critical.
- Collaborate with your healthcare provider to personalize your treatment plan and understand the risks.
References
- https://www.ahajournals.org/doi/10.1161/circulationaha.105.540476
- https://www.ncbi.nlm.nih.gov/books/NBK540985/
- https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af/atrial-flutter
- https://www.healthline.com/health/atrial-flutter-vs-atrial-fibrillation
- https://www.medicalnewstoday.com/articles/afib-flutter
- https://www.healthline.com/health/video/the-atrial-fibrillation-warning-signs-you-need-to-know
- https://www.nursingcenter.com/ncblog/july-2024/atrial-arrhythmias-is-it-fibrillation-or-flutter
Read full bio of medha deb












