Atrial Fibrillation Symptoms at Night: What You Need to Know
Understand how atrial fibrillation can present uniquely at night, why symptoms may be more noticeable, and how to manage AFib for better sleep and heart health.
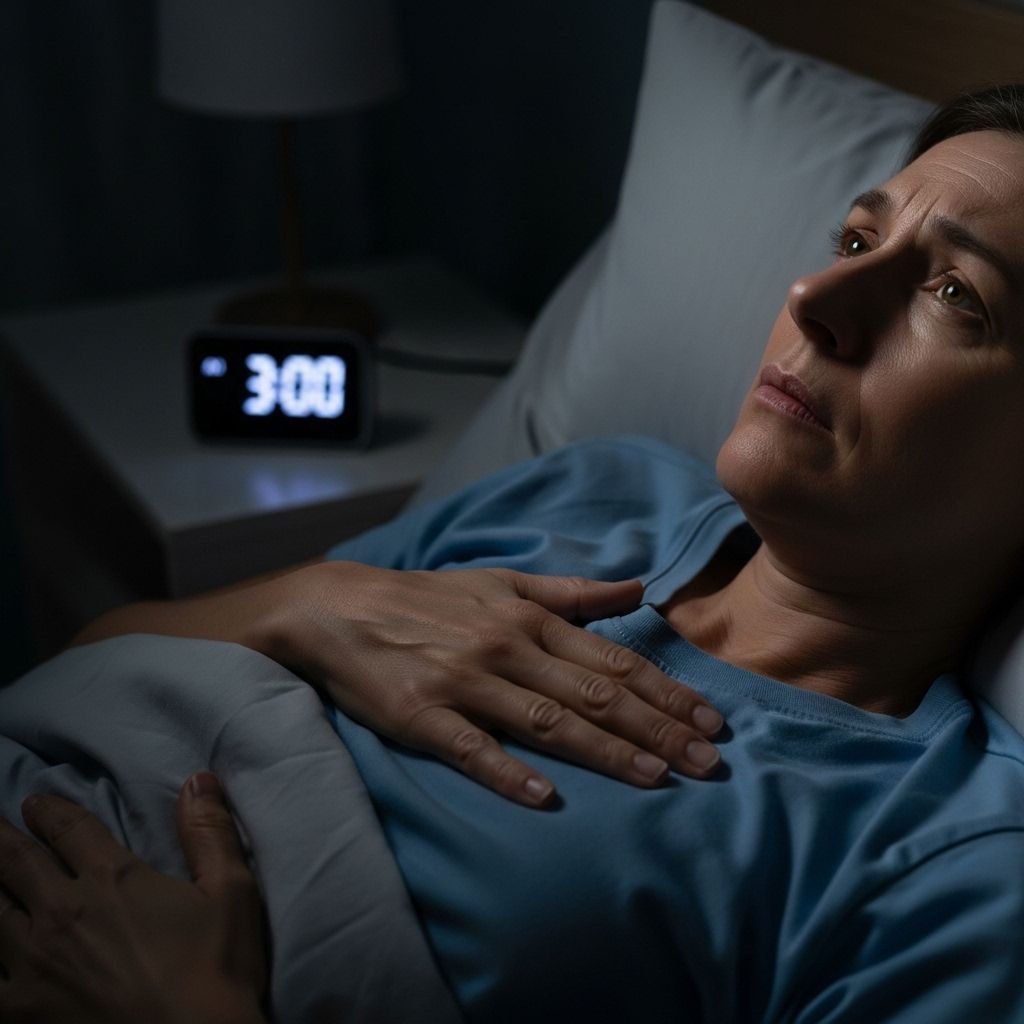
Atrial fibrillation (AFib) is a common form of arrhythmia that can disrupt your daily life—and, for many, its symptoms become most apparent or intense at night. Understanding why AFib can act up when you are lying down is crucial for managing symptoms, preventing complications, and achieving restful sleep.
What Is Atrial Fibrillation?
Atrial fibrillation (AFib) is an irregular and often rapid heart rhythm that originates in the upper chambers (atria) of the heart. During AFib, the heart’s electrical signals become disorganized, causing the atria to quiver instead of contracting effectively. This disruption impairs normal blood flow from the atria to the lower chambers (ventricles), increasing the risk of blood clots and potentially leading to serious complications such as stroke, heart failure, and other cardiovascular conditions.
- AFib is the most common heart rhythm disorder worldwide
- It often affects adults over 65 but can occur at any age
- The risk increases with age, certain chronic health conditions, obesity, and family history
Why Are AFib Symptoms Worse at Night?
Many people notice that their atrial fibrillation symptoms are most bothersome at night or when lying down. Multiple factors contribute to this pattern:
- Increased Vagus Nerve Activity: The vagus nerve slows the heart rate and is more active at rest or during sleep. In some individuals, this triggers abnormal electrical signaling in the atria and increases the likelihood of AFib episodes at night.
- Position Change: Lying down increases blood flow back to the heart (venous return), which may stretch the atria and exacerbate irregular rhythms or palpitations.
- Other Underlying Conditions: Nighttime is when certain conditions, like sleep apnea or gastroesophageal reflux disease (GERD), can flare up and, in turn, provoke or worsen AFib symptoms.
- Reduced Distraction: At night, you’re less distracted by daily activities and more likely to notice palpitations, irregular heartbeat, or chest discomfort.
Together, these factors contribute to the heightened perception and sometimes actual increase in AFib symptoms while resting or trying to sleep.
Common Symptoms of AFib at Night
The symptoms of atrial fibrillation may not always be present or may be subtle, especially in the early stages. However, at night, they can become more pronounced and may interfere with sleep quality. Nighttime AFib symptoms can include:
- Heart palpitations: Sensation of fluttering, pounding, or racing heart
- Chest discomfort or pain: Pressure or aching in the chest
- Shortness of breath or trouble breathing: Especially when lying flat
- Fatigue or weakness: Feeling unusually tired or drained after awakening
- Dizziness or lightheadedness: Sensation of being unsteady when getting up at night
- Difficulty sleeping: Frequent nighttime awakenings due to discomfort
Some individuals experience “silent AFib” with no noticeable symptoms, even overnight. This type can only be detected with a heart rhythm monitor or ECG and is still associated with an increased risk of complications.
What Causes Nighttime Episodes of AFib?
Several triggers or underlying conditions can instigate atrial fibrillation episodes at night:
- Sleep Apnea: Repeated pauses in breathing during sleep can alter oxygen levels and increase pressure in the chest, triggering AFib
- High Vagal Tone: Enhanced parasympathetic (rest and digest) activity during sleep may destabilize heart rhythms
- Fluid Redistribution: Lying down shifts body fluids, increasing blood volume returning to the heart
- Alcohol or Large Evening Meals: Both can stress the heart and digestive system, potentially provoking arrhythmias during the night
- Caffeine or Stimulant Medications: Evening consumption may heighten heart rate and trigger AFib
- Heart Disease: Conditions like heart failure or valve disorders greatly raise risk
- Chronic Illness: Thyroid disease, obesity, diabetes, and chronic lung disease also increase likelihood
Complications of Untreated AFib at Night
Ignoring nighttime AFib can carry significant risks. AFib increases the risk of:
- Stroke: Inefficient heart contractions may allow blood clots to form in the atria, which can then travel to the brain
- Heart Failure: Chronic rapid or irregular rhythms can weaken the heart over time
- Sudden Cardiac Arrest: Although rare, irregular heart rhythms can sometimes escalate to life-threatening arrhythmias
- Cognitive Impairment or Dementia: Poor blood flow caused by AFib has been linked to cognitive decline over time
The risk of complications persists even if nighttime AFib is the only manifestation. Silent, undiagnosed AFib can be particularly dangerous due to lack of treatment.
Who Is Most at Risk for Nighttime AFib?
Several groups are more likely to experience nighttime atrial fibrillation:
- Older adults (especially 65+)
- People with a family history of AFib
- Individuals with sleep apnea or obesity
- People with high blood pressure or heart disease
- Those with thyroid disorders
Women and certain ethnic groups may also have distinctive risk profiles, though AFib remains most common in older men.
How Is Nighttime AFib Diagnosed?
Diagnosis begins with a careful medical history and physical exam, but the gold standard is an electrocardiogram (ECG or EKG), which records the electrical activity of the heart. Sometimes, nighttime or intermittent episodes can be tricky to catch during a standard ECG, so your doctor might recommend:
- Holter monitor: A portable ECG worn for 24-48 hours to catch irregular rhythms as they occur, including overnight
- Event monitor: A device worn for several weeks to track less frequent symptoms
- Implantable loop recorder: A device placed under the skin to monitor heart rhythms long-term, especially for suspected silent AFib
Other tests may target underlying causes, such as overnight sleep studies (if sleep apnea is suspected), blood tests (for thyroid issues), or echocardiograms to look at heart structure.
Managing Nighttime AFib: Effective Strategies
Management focuses on controlling the heart’s rhythm or rate, preventing complications, and addressing factors that trigger nighttime symptoms. Treatment may include:
| Treatment Option | How It Helps |
|---|---|
| Medications to control rate/rhythm | Beta-blockers, calcium channel blockers, or antiarrhythmic drugs keep the heart from beating too fast or irregularly |
| Blood thinners (anticoagulants) | Reduce the risk of stroke by lowering the likelihood of blood clots |
| Lifestyle changes | Weight management, reduced alcohol and caffeine, regular exercise, and improved sleep hygiene support overall cardiovascular health |
| Treating secondary conditions | Addressing sleep apnea, thyroid issues, and high blood pressure can lower the frequency and severity of episodes |
| Ablation procedures | In minimally invasive procedures, targeted heart tissue is “ablated” (destroyed) to prevent abnormal electrical signals |
| Cardioversion | A controlled electric shock restores normal rhythm (for some patients) |
Tips for Better Sleep and Fewer Nighttime AFib Episodes
Simple changes can help reduce the occurrence or severity of nighttime atrial fibrillation:
- Elevate your head: Use extra pillows to decrease venous return and reduce heart strain while lying down
- Maintain a healthy sleep schedule: Go to bed and wake up at the same time each day
- Avoid heavy meals, alcohol, or caffeine in the evening
- Address snoring or sleep apnea: Ask your doctor about a sleep study if you have risk factors like obesity, loud snoring, or excessive daytime sleepiness
- Manage stress: Use relaxation practices (such as meditation or gentle yoga) before bed
- Monitor your symptoms: Keep a diary to track episodes and discuss with your healthcare provider
When to Seek Immediate Medical Help
Not all AFib requires emergency care, but certain symptoms should be taken seriously. Contact emergency services immediately if you develop:
- Severe or persistent chest pain
- Extreme shortness of breath
- Sudden weakness, numbness, or difficulty speaking (possible stroke symptoms)
- Fainting or near-fainting spells
Frequently Asked Questions (FAQs)
Q: Can AFib only occur at night?
No, atrial fibrillation can occur at any time of day, but many notice symptoms or have AFib episodes more frequently at night due to physiological changes during sleep or rest.
Q: Is AFib at night more dangerous than daytime episodes?
Nighttime AFib is not inherently more dangerous, but because symptoms can be subtle or go unnoticed (especially if you’re asleep), there is a risk of undiagnosed AFib and related complications.
Q: Will treating sleep apnea help my AFib?
Yes, for many, managing underlying sleep apnea (using CPAP or other therapies) significantly reduces nighttime AFib symptoms and episodes.
Q: If I have AFib but no symptoms at night, should I still worry?
Yes. Even asymptomatic (silent) AFib increases risk for complications such as stroke and heart failure. Regular monitoring and working with your healthcare provider are essential.
Q: What lifestyle changes are most effective for reducing nighttime AFib?
Losing excess weight, treating sleep apnea, avoiding heavy evening meals/alcohol/caffeine, managing stress, and maintaining regular exercise can all help.
Key Takeaways
- Nighttime is a common time to notice or experience AFib symptoms due to changes in the body’s physiology and less distraction from daily activities.
- Typical symptoms at night include palpitations, chest discomfort, shortness of breath, and insomnia.
- Left untreated, AFib increases the risk for stroke, heart failure, and cognitive decline—even if only present at night or during sleep.
- If you suspect you have AFib, talk to your healthcare provider for proper diagnosis and a personalized treatment plan.
- Lifestyle changes, medical therapy, and managing related health conditions can greatly reduce nighttime symptoms and improve overall heart health.
References
- https://www.healthline.com/health/heart/silent-afib
- https://medlineplus.gov/atrialfibrillation.html
- https://www.medicalnewstoday.com/articles/323621
- https://www.healthline.com/health/video/ways-to-manage-afib-symptoms-daily
- https://www.healthline.com/health/video/afib-insights-understanding-the-causes-of-your-irregular-heartbeat
- https://www.healthline.com/health/video/the-atrial-fibrillation-warning-signs-you-need-to-know
- https://www.healthline.com/health/video/exercise-with-afib-what-you-need-to-know
- https://connect.mayoclinic.org/discussion/premature-atrial-contractions/
Read full bio of medha deb












