Atrial Fibrillation Ablation: Techniques, Benefits, and Patient Considerations
Comprehensive overview of atrial fibrillation ablation, including procedure details, benefits, risks, and patient expectations.
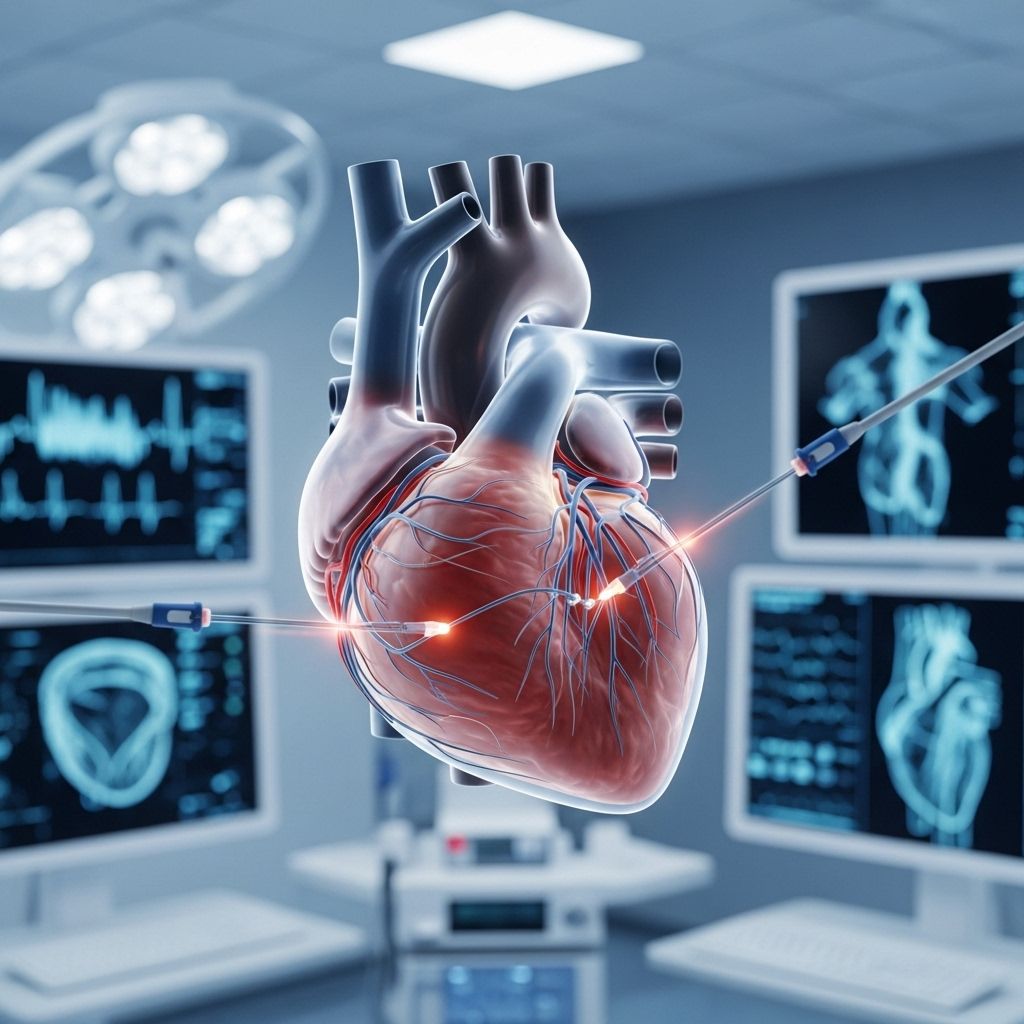
Atrial fibrillation (AFib) ablation is an advanced procedure designed to treat the irregular heart rhythm known as atrial fibrillation. It uses energy to strategically create small scars on heart tissue, disrupting faulty electrical signals and restoring normal rhythm when medications or other treatments have failed or are unsuitable.
What Is Atrial Fibrillation?
Atrial fibrillation is a common cardiac arrhythmia marked by rapid and irregular beating of the heart’s upper chambers (atria). Normally, the sinus node—the heart’s natural pacemaker—sends regular electrical impulses that coordinate heartbeats. In AFib, chaotic signals in the atria override the normal pathway, resulting in poor blood pumping and increased risk of stroke or heart failure.
- Symptoms of AFib: Palpitations, shortness of breath, chest discomfort, fatigue.
- Risks: Blood clots, stroke, heart failure.
- Treatment goals: Control heart rate, restore normal rhythm, reduce complications.
Why Is Atrial Fibrillation Ablation Performed?
AFib ablation is recommended when:
- Medications and other therapies (like lifestyle changes or electrical cardioversion) fail to control symptoms.
- The goal is to restore and preserve normal heart rhythm in suitable candidates.
- There are frequent, symptomatic AFib episodes that impact quality of life.
- There’s evidence of high risk for stroke or heart failure due to sustained abnormal rhythm.
For some patients, ablation may be considered a first-line treatment, especially when other interventions are contraindicated or poorly tolerated. It’s mainly proposed for people with symptomatic, frequent episodes and less structural heart disease or atrial enlargement.
Types of Atrial Fibrillation Ablation Procedures
The two main categories are catheter ablation and surgical ablation:
- Catheter Ablation: Most commonly performed. Flexible tubes are inserted via blood vessels (usually via the groin) and guided to the heart. Delivers targeted energy (radiofrequency heat or cryotherapy/cold) to ablate problematic tissue.
- Surgical Ablation: Performed less frequently, generally during open-heart surgery. Techniques include the Maze Procedure, where a controlled pattern of scars blocks the transmission of abnormal signals.
Special approaches:
- AV Node Ablation: Damages the connection between atria and ventricles; an artificial pacemaker controls rhythm.
- Pulmonary Vein Isolation (PVI): The most common strategy isolates electrical triggers located at the pulmonary veins’ openings.
How Catheter Ablation Works
The central goal is to silence the abnormal electrical signals causing AFib while preserving the heart’s normal conduction system. Below is the procedure overview:
- Preparation
- Performed in a hospital electrophysiology (EP) or cath lab.
- Patient is given anesthesia (general or local) and sedatives.
- Blood-thinning medicine is started before, during, and after to lower stroke risk.
- Catheter Placement and Mapping
- Electrical catheters are inserted (usually via groin veins; sometimes neck vein).
- Imaging technologies (X-ray, ultrasound, 3D mapping) guide catheter position.
- Transesophageal echocardiogram may be used for real-time heart imaging.
- Electrophysiology study maps heart’s electrical activity to pinpoint abnormal areas.
- Ablation
- Energy (heat or cold) is delivered via the catheter tip to ablate targeted tissue.
- Circumferential ablation often performed around each pulmonary vein opening.
- Duration: Ablation itself takes about 30-40 minutes, full procedure averages 3–4 hours.
- If persistent AFib, additional areas may be ablated for broader substrate modification.
- Final Steps and Recovery
- Vascular closure system is used at the insertion site to allow early mobilization.
- Monitoring for complications and arrhythmia recurrence post-procedure.
Technologies Used in Catheter Ablation
| Technology | Description | Main Uses |
|---|---|---|
| Radiofrequency Ablation | Uses heat delivered through the catheter tip to create microscopic scars. | PVI, focal ablation |
| Cryoablation (Cryo-balloon) | Uses cold energy to ablate specific regions, especially pulmonary vein openings. | PVI |
| Electro-anatomical Mapping | 3D mapping system to guide precise localization of abnormal pathways. | Procedure navigation |
| Transesophageal Echocardiography | Ultrasound probe in the esophagus for real-time heart imaging. | Pre- and intra-procedural imaging |
Candidate Selection: Who Benefits Most from AFib Ablation?
- Ideal Candidates:
- Relatively younger patients with frequent, symptomatic episodes.
- No significant structural heart disease.
- No significant enlargement of the left atrium.
- Failed or intolerant to antiarrhythmic drugs.
- Inappropriate Candidates:
- Severe atrial enlargement, extensive structural heart disease.
- Advanced comorbidities increasing procedural risks.
- Contraindications to blood thinners or anesthesia.
Benefits of AFib Ablation
- Improved Quality of Life: Ablation often results in significant symptom reduction, with improved energy and exercise tolerance.
- Restored Normal Rhythm: Restoration and maintenance of normal heart rhythm are often achieved, especially in paroxysmal AFib.
- Reduced Hospitalization and Medication Need: Successful ablation can lower reliance on antiarrhythmic drugs.
- Pulmonary Vein Isolation: Most successful strategy for recurrent AFib due to pulmonary vein triggers.
- Potential Reduction in Stroke and Heart Failure Risk: Observed particularly in selected patient populations.
Risks and Possible Complications
While AFib ablation can be highly beneficial, it is not without risks. Serious complications include:
- Cardiac tamponade: Build-up of fluid around the heart.
- Stroke or transient ischemic attack (TIA): Related to clot formation during/after the procedure.
- Pulmonary vein stenosis: Narrowing of vein openings due to scar formation.
- Atrio-esophageal fistula: Rare, but potentially fatal connection between the heart and esophagus.
- Bleeding, vascular injury at the catheter insertion site.
- Arrhythmia recurrence: Recurrence rates post-ablation vary from 50–80% over the long-term, often due to vein reconnection or persistent atrial remodeling.
- Anesthesia-related risks.
Preventive strategies include close follow-up and sometimes repeat procedures to manage recurrence.
Recovery After Ablation
- Immediate Recovery:
- Hospital stay ranges from a few hours to overnight observation.
- Early mobilization is encouraged using advanced vascular closure methods.
- Post-Procedure Care:
- Continuous blood thinning medication for several weeks or months to lower clot risk.
- Periodic ECG and follow-up appointments to monitor rhythm stability.
- Some patients experience “early recurrence” of arrhythmia within 2–3 months, which may resolve over time.
- Long-Term Outlook:
- Success rates for maintaining normal rhythm improve with repeat procedures.
- Some may require continued or additional antiarrhythmic therapy if recurrence occurs.
- Quality of life improvement is substantial for most suitable candidates.
Frequently Asked Questions (FAQs)
Q: Is atrial fibrillation ablation painful?
A: Most people do not feel pain during the procedure, as sedation or anesthesia is used. You may experience mild discomfort at the catheter site after the procedure, but severe pain is uncommon and should be reported to your medical team.
Q: How long does the ablation procedure take?
A: The actual ablation part can take 30–40 minutes, but the total procedure typically lasts 3–4 hours due to pre-, intra-, and post-procedural steps.
Q: Does ablation cure atrial fibrillation?
A: Ablation can significantly reduce or eliminate AFib episodes for many patients, but arrhythmia recurrence is possible, especially in persistent AFib or those with advanced atrial remodeling.
Q: What are the common risks?
A: Risks include bleeding, infection, stroke, cardiac tamponade, and rare but serious injuries to the heart or surrounding structures. These are generally low in skilled centers but must be discussed with your doctor.
Q: Will I need more than one ablation?
A: Some patients need repeat procedures for lasting rhythm control, especially if early recurrence or pulmonary vein reconnection occurs.
Q: When can I return to normal activity?
A: Most people resume light activities within 1–2 days after discharge and return to routine work or exercise after several days, depending on their doctor’s guidance.
Key Takeaways
- Atrial fibrillation ablation is a safe, effective treatment for restoring normal heart rhythm in selected patients.
- It uses precision energy to eliminate sources of erratic electrical signals in the heart.
- Success rates are highest in younger patients with less structural heart disease and frequent, symptomatic AFib.
- Risks exist and must be balanced against benefits; thorough discussion with an electrophysiologist is critical.
- Follow-up care and sometimes repeat procedures may be necessary for optimal outcomes.
References
- https://www.melbourneheartrhythm.com.au/learn/procedures/13-atrial-fibrillation-ablation?showall=1
- https://www.mayoclinic.org/tests-procedures/atrial-fibrillation-ablation/about/pac-20384969
- https://nyulangone.org/conditions/atrial-fibrillation-atrial-flutter/treatments/catheter-ablation-for-atrial-fibrillation-atrial-flutter
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5565661/
- https://www.heart.org/en/health-topics/arrhythmia/prevention–treatment-of-arrhythmia/ablation-for-arrhythmias
- https://my.clevelandclinic.org/health/treatments/16851-catheter-ablation
- https://www.youtube.com/watch?v=DNHQ5ClaEdM
- https://news.bostonscientific.com/cardiac-ablation-for-afib
- https://www.youtube.com/watch?v=3_aR0jL9BSU
Read full bio of Sneha Tete












