When Does Atherosclerosis Start? Understanding Early Onset and Risks
Uncover how atherosclerosis develops over a lifetime, who is at risk, and what early signs to watch for to protect your heart and arteries.
When Does Atherosclerosis Start? Early Origin and Lifelong Risks
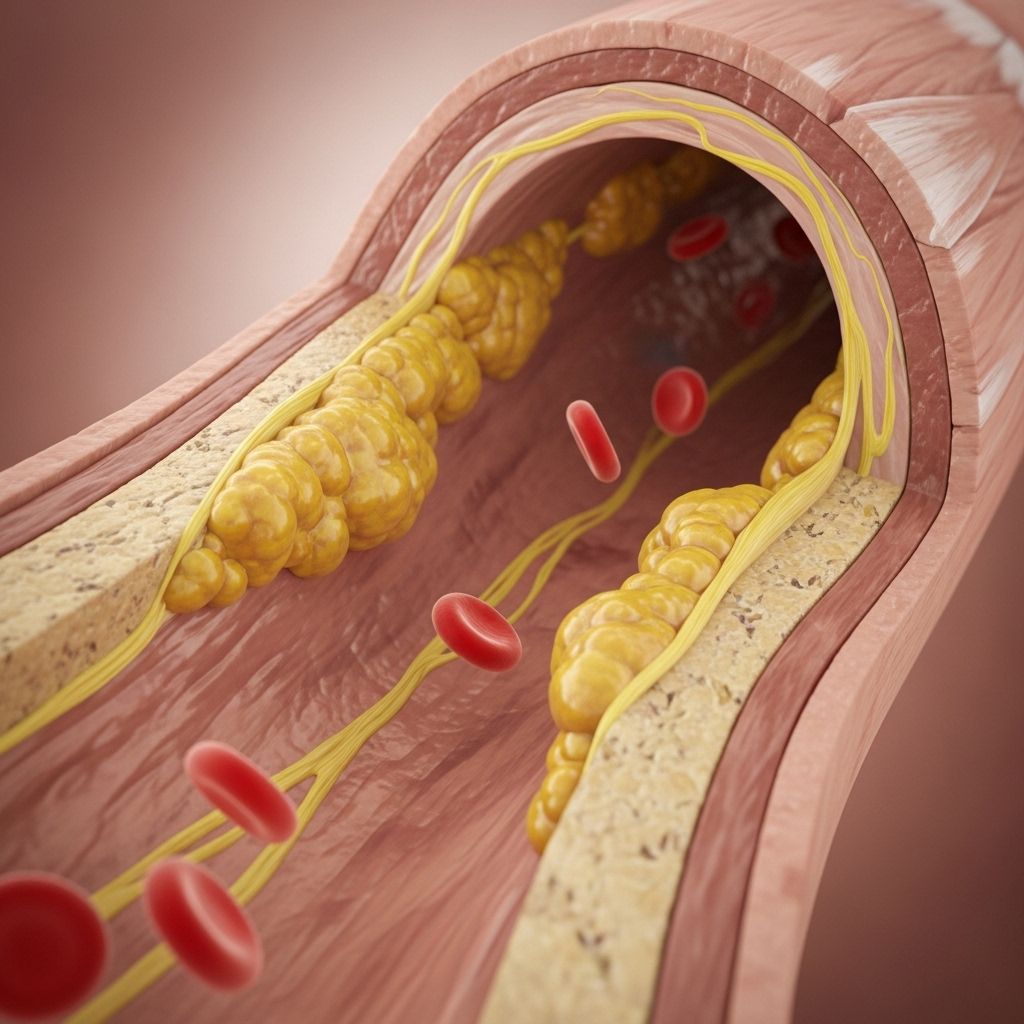
Atherosclerosis is a chronic condition characterized by the buildup of fatty deposits, cholesterol, and other substances (commonly known as plaque) along the walls of your arteries. Most people associate it with heart attacks and strokes later in life, but research shows that the process often begins much earlier than symptoms appear — even in childhood or adolescence. Understanding this early onset and the contributing factors can help you take action before the disease silently progresses.
What Is Atherosclerosis?
Atherosclerosis is the progressive hardening and narrowing of the arteries due to the accumulation of plaque. This plaque is primarily made of lipids, cholesterol, calcium, and cellular waste. Over time, plaque restricts blood flow or triggers sudden, catastrophic events such as heart attacks or strokes. The condition develops slowly, often showing no symptoms until it becomes severe or causes an acute blockage.
How Early Does Atherosclerosis Begin?
- Children and Adolescents: Evidence from autopsies and imaging studies reveal the presence of fatty streaks — the earliest signs of atherosclerosis — in the arteries of children as young as 10 years old.
- Young Adults: In some cases, plaque progression advances through the teens and twenties, particularly among those with genetic predispositions or exposure to risk factors.
- Middle Age and Beyond: While the process often begins young, symptoms typically don’t appear until middle age or later, when blockages become significant or plaque ruptures occur.
The silent nature of early atherosclerosis makes awareness and prevention essential from an early age.
Stages of Atherosclerosis
The development of atherosclerosis follows a series of identifiable stages:
| Stage | Description |
|---|---|
| 1. Endothelial Damage | Initial injury to the lining of the artery (endothelium), often from high blood pressure, smoking, diabetes, high cholesterol, or inflammation. |
| 2. Fatty Streak Formation | Accumulation of cholesterol-rich foam cells (from white blood cells) just beneath the arterial lining, creating a yellowish streak, often seen in youth. |
| 3. Plaque Progression (Fibrous Plaque) | Fibrous tissue forms over the fatty streak, developing into a larger, more stable plaque that begins to narrow the artery. |
| 4. Plaque Complications (Plaque Rupture and Thrombosis) | The fibrous cap covering the plaque can rupture, triggering blood clots that can cause heart attacks or strokes. |
Each stage may last for years, and progression varies greatly based on genetics, lifestyle, and other risk factors.
Causes and Major Risk Factors
Atherosclerosis results from a complex interplay between genetic, environmental, and lifestyle influences. Some risk factors are non-modifiable, while others can be addressed through lifestyle changes or medical management.
- High LDL (“bad”) cholesterol: Excess LDL cholesterol initiates and accelerates fatty streak formation.
- High blood pressure: Damages the artery wall, making it more susceptible to plaque accumulation.
- Type 2 diabetes and insulin resistance: Increases inflammation and cholesterol buildup in the arteries.
- Smoking: Directly injures the endothelium and amplifies other risk factors.
- Obesity: Promotes inflammation and negatively influences cholesterol and glucose metabolism.
- Family history and genetics: Inherited traits can significantly impact your risk and the pace of disease progression.
- Chronic inflammation: Diseases like lupus, rheumatoid arthritis, psoriasis, and certain infections can start or worsen the process.
Symptoms: When Does Atherosclerosis Become Noticeable?
In its early stages, atherosclerosis is generally “silent,” presenting no obvious symptoms. Symptoms usually result from significant blockage or a sudden blockage due to ruptured plaques. The specific symptoms depend on which arteries are affected:
- Heart (Coronary Arteries): Chest pain or discomfort (angina), shortness of breath, heart palpitations, or heart attack.
- Brain (Carotid or Cerebral Arteries): Sudden numbness or weakness (often on one side), facial drooping, speech difficulties, sudden vision problems, or stroke.
- Legs (Peripheral Arteries): Cramping or pain while walking (claudication), numbness, weakness, or even non-healing wounds.
- Kidneys (Renal Arteries): High blood pressure or kidney dysfunction.
- Intestinal arteries: Abdominal pain after eating, unintentional weight loss.
Recognizing and reporting these symptoms early can be lifesaving.
How Is Early Atherosclerosis Detected?
Detecting atherosclerosis in its early stages is challenging but possible with certain tests.
- Physical examination: May detect decreased pulses or blood pressure differences between limbs.
- Blood tests: Monitor cholesterol, blood sugar, and inflammation markers.
- Imaging tests: Carotid ultrasound, coronary artery calcium scoring (via CT scan), and other vascular imaging can reveal plaques before symptoms develop.
- Non-invasive vascular studies: Ankle-brachial index (ABI) for leg artery disease, or advanced imaging for coronary arteries.
Your doctor will assess your risk based on overall health, family history, and these diagnostic findings.
How Fast Does Atherosclerosis Progress?
Progression is highly variable. Some plaques remain stable for decades, causing little to no symptoms, while others grow or rupture unpredictably, triggering acute blockages. Risk factors, genetic predisposition, and lifestyle choices all determine the speed of progression.
- In some people, plaque buildup is steady but slow, not causing symptoms until later adulthood or not at all.
- Other cases see plaques remain small and stable for years, then abruptly rupture.
- Intervention (healthy lifestyle and/or medication) can dramatically slow or even halt progression in many individuals.
Who Is Most at Risk for Early Atherosclerosis?
Risk is cumulative and influenced by inherited and acquired factors.
- Family history of early heart disease or stroke: Strongly raises risk, especially if a parent had heart disease before age 55 (men) or 65 (women).
- Genetic conditions: Familial hypercholesterolemia and other inherited disorders cause high cholesterol from a young age.
- Uncontrolled risk factors: High blood pressure, diabetes, smoking, and high cholesterol — especially when starting in youth.
- Autoimmune or chronic inflammatory conditions: These accelerate vascular damage and plaque formation.
Even children can develop early fatty streaks if exposed to significant risk factors.
Can Atherosclerosis Be Prevented or Delayed?
Many cases of early atherosclerosis are preventable or reversible, especially with intervention before significant artery narrowing occurs.
- Manage blood pressure, cholesterol, and blood sugar: Regular monitoring and medication when necessary.
- Adopt a heart-healthy diet: High in fruits, vegetables, whole grains, lean protein, and healthy fats. Limit saturated fats, trans fats, sodium, and sugar.
- Exercise regularly: At least 150 minutes of moderate activity weekly helps control weight and improve vascular health.
- Quit smoking: Stopping tobacco use quickly reduces risk and improves artery function.
- Maintain a healthy weight: Reduces diabetes and high blood pressure risk.
- Control chronic conditions: Properly manage diabetes, kidney disease, and inflammation.
Long-Term Outlook and Complications
If left unchecked, atherosclerosis can progress to serious, potentially fatal complications:
- Heart attack (myocardial infarction)
- Stroke (ischemic type)
- Peripheral arterial disease (PAD): Leading to limb pain, ulcers, or even amputation
- Aneurysm: Weakened, bulging artery wall at risk for rupture
- Chronic kidney disease
However, positive lifestyle changes, medical management, and early screening significantly improve outcomes and quality of life.
Frequently Asked Questions (FAQs)
Q: What are the earliest signs of atherosclerosis?
A: Most people do not experience symptoms until plaques are large or rupture. Early signs can include decreased exercise tolerance, mild chest discomfort, or leg cramping during physical activity. In many, the first sign is a heart attack or stroke.
Q: How is atherosclerosis in children possible?
A: Risk factors such as obesity, diabetes, and familial hypercholesterolemia, as well as poor diet and exposure to tobacco smoke, can start the disease process early, with fatty streaks observed in adolescence or even younger.
Q: Can atherosclerosis be reversed?
A: Some early changes, particularly fatty streaks, can be stabilized or partially reversed with aggressive risk factor modification. Advanced plaques typically can’t be eliminated completely, but progression can be significantly slowed.
Q: What are the four main stages of atherosclerosis?
A: The four stages are: Endothelial damage, fatty streak formation, fibrous plaque development, and plaque rupture leading to potential clot formation.
Q: How long can you live with atherosclerosis?
A: With early detection and proper management, many people with atherosclerosis can live long, healthy lives. Neglecting care, however, may shorten lifespan, especially after heart attacks, heart failure, or strokes.
Summary: Taking Early Action for Lifelong Artery Health
Atherosclerosis is a lifelong condition that often starts much earlier than most people realize. While symptoms typically surface in middle age or older, the process begins silently in childhood or teenage years. The good news is that, with modern understanding, targeted lifestyle changes, early screening, and medical management, you can minimize your lifetime risk and protect your arteries and heart well into old age.
- Promote healthy habits as early as possible
- Know your family history and discuss screening options with your doctor
- Address risk factors — smoking, high cholesterol, high blood pressure, diabetes — promptly
Awareness and prevention are the best ways to guard against the lifelong threat of atherosclerosis.
References
- https://www.webmd.com/heart-disease/what-is-atherosclerosis
- https://www.nyp.org/heart/atherosclerosis
- https://www.advocatehealth.com/health-services/advocate-heart-institute/conditions/vascular-disease/atherosclerosis
- https://my.clevelandclinic.org/health/diseases/16753-atherosclerosis-arterial-disease
- https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569
- https://www.pennmedicine.org/conditions/atherosclerosis
- https://my.clevelandclinic.org/watch/where-atherosclerosis-symptoms-can-appear
- https://medlineplus.gov/atherosclerosis.html
Read full bio of medha deb












