Atherectomy Heart Procedure: Overview, Risks, Benefits, and Recovery
A comprehensive patient guide to understanding the atherectomy heart procedure, including what to expect, risks, and recovery tips.
Atherectomy is a minimally invasive heart procedure designed to remove plaque build-up from arteries. This comprehensive guide covers everything you need to know, from preparation and who needs the procedure to its risks, benefits, the step-by-step process, and recovery expectations. We also answer common questions to help you make informed decisions about your heart health.
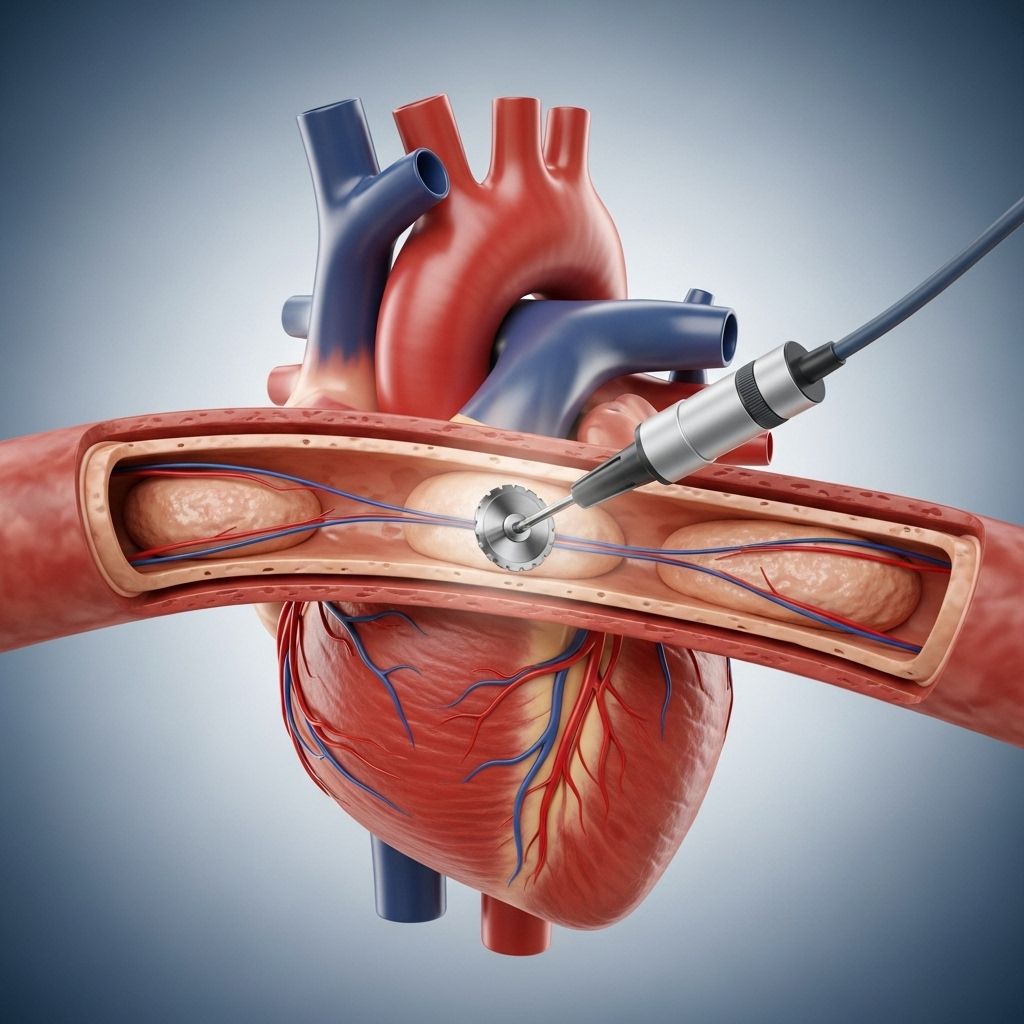
What is Atherectomy?
An atherectomy is a medical procedure that removes plaque—fatty deposits made up of calcium, cholesterol, and other substances—from inside the arteries. Plaque buildup in arteries, known as atherosclerosis, narrows blood vessels and restricts blood flow, potentially leading to significant health complications such as heart attack, stroke, peripheral artery disease (PAD), kidney problems, or loss of limb function.
Key Features of Atherectomy
- Minimally invasive: Involves a small incision and the insertion of a specialized catheter.
- Used to treat atherosclerosis: Primarily for blockages in coronary (heart) or peripheral (leg) arteries.
- Can be performed alone or with other procedures: Frequently combined with angioplasty or stent placement, based on the physician’s evaluation.
Conditions Treated by Atherectomy
Atherectomy is primarily used to treat atherosclerosis, a chronic condition characterized by hardening and narrowing of the arteries. Contributing factors to atherosclerosis include:
- High cholesterol
- High blood pressure
- Obesity
- Diabetes
- Smoking
- Chronic inflammation (e.g., arthritis, lupus)
Untreated atherosclerosis can lead to serious complications, such as:
- Coronary artery disease (leading to heart attacks)
- Stroke
- Peripheral artery disease (PAD)
- Chronic kidney disease
- Blood clots
Who Needs an Atherectomy?
Atherectomy may be recommended if you have symptoms of arterial blockages such as chest pain, shortness of breath, leg pain during walking, or other circulatory issues, and other approaches like medication, lifestyle changes, or less invasive interventions have not been effective. Your doctor will evaluate the severity and location of arterial plaque through a combination of tests and medical history.
Diagnostic Tests Often Used
- Electrocardiogram (ECG): Measures electrical activity and heart rhythm.
- Echocardiogram: An ultrasound to visualize the heart and assess its function.
- Stress Test: Evaluates heart function under physical exertion.
- Angiogram: X-ray imaging to identify blockages in blood vessels.
Types of Atherectomy Devices
The choice of device depends on plaque composition, location, and the specific artery involved. The main types include:
| Device Type | Mechanism | Typical Use |
|---|---|---|
| Rotational | Rotating blade or burr sands or cuts plaque | For calcified (hard) plaque |
| Directional | Rotating blade cuts specific targeted plaque area | For localized plaque removal, often in large vessels |
| Orbital | Spinning diamond-coated crown sands plaque in a circular motion | For arteries with concentric buildup |
| Laser | Emits laser energy to vaporize or burn away plaque | For fibrous or mixed plaques, and small vessels |
How the Atherectomy Heart Procedure Works
Where: Atherectomy is usually performed in a hybrid operating room (cath lab plus surgical suite) or a specialized interventional radiology suite.
Anesthesia: Local anesthesia at the incision site, often combined with mild sedation for comfort.
Step-by-Step Walkthrough
- Preparation: You will change into a hospital gown and lie flat on a procedural table. IV lines are started for fluids and medication. Monitoring devices are attached for heart rate and vital signs.
- Imaging and Planning: A contrast dye is injected into the bloodstream to help the doctor precisely locate blockages with real-time imaging (fluoroscopy or X-ray).
- Incision and Catheterization: A small incision (typically in the groin, wrist, upper thigh, or arm) provides access to the target artery. A catheter is inserted into the artery using a guide wire.
- Device Selection: Based on the size, location, and nature of the blockage, the surgeon selects the most appropriate atherectomy device.
- Plaque Removal: The device at the catheter tip (blade, laser, or sanding tool) is guided to the blockage and activated to mechanically remove, cut, or vaporize the plaque. Multiple passes may be needed.
- Plaque Collection: Most devices have a capture chamber to collect dislodged plaque, minimizing the risk of embolization.
- Device and Catheter Removal: Once enough plaque has been removed and blood flow improves, the catheter is withdrawn, and the incision is closed using manual pressure, a closure device, or a few stitches.
- Post-Procedure Imaging: Additional angiography is performed to confirm successful blood flow restoration.
Throughout the procedure, you are typically awake but sedated—you should not feel pain, just mild pressure or movement sensations where the catheter is manipulated.
Atherectomy vs. Angioplasty and Stenting
Atherectomy is often compared to angioplasty (balloon dilation) and stenting. Here is a basic comparison:
| Procedure | Primary Method | Best For… |
|---|---|---|
| Atherectomy | Physically removes plaque from artery wall | Hard/calcified or complex blockages not well treated with angioplasty alone |
| Angioplasty | Inflates a balloon to widen plaque-narrowed artery | Softer plaque, less severe or long blockages |
| Stenting | Places a metal mesh tube to keep artery open | Maintaining long-term patency following atherectomy or angioplasty |
Often, these techniques are combined—an atherectomy is performed to remove the plaque, followed by balloon angioplasty and/or stenting to provide structural support and prevent re-narrowing.
Potential Risks and Complications
While atherectomy is generally considered safe, it still carries risks, as with any cardiac or vascular procedure. Possible complications include:
- Bleeding or prolonged bruising at the incision site
- Infection at the site
- Damage to the artery (e.g., tearing, perforation)
- Distal embolization: Dislodged plaque may travel further downstream, causing additional blockages
- Heart attack: Occurs in up to 1.3% of procedures
- Slow or blocked blood flow to the heart (no-reflow phenomenon)
- Reblockage or artery closure
Risk factors for complications include advanced age, other chronic diseases (diabetes, kidney disease), poor circulation, or previous interventions in the target area. Your healthcare provider will discuss your individual risk profile and take steps to mitigate these risks.
Benefits of Atherectomy
- Improved Blood Flow: Restores circulation, reducing symptoms like chest pain, leg pain, fatigue, or non-healing wounds.
- Symptom Relief: Many patients experience rapid improvement in mobility and comfort after the procedure.
- Minimally Invasive: Compared to open surgery, atherectomy has less bleeding, fewer infections, and shorter hospital stays.
- Reduced Need for Surgery: Effective plaque removal early may delay or prevent the need for bypass surgery or amputations.
- Quicker Recovery: Most patients return to normal routines within days of the procedure.
Aftercare and Recovery
Recovery starts immediately after atherectomy and generally progresses quickly. Here’s what to expect:
- Initial Recovery: Must lie flat for several hours to prevent bleeding. Hospital observation may last overnight.
- Vital Monitoring: Continuous checks of blood pressure, heart rate, and puncture site for complications.
- Activity: Most people can resume light activities within a few days. Avoid heavy lifting or strenuous exercise until cleared by your doctor.
- Medications: Blood thinners (e.g., aspirin, clopidogrel) are often prescribed to prevent clots. Take all medications exactly as directed.
- Follow-up: Multiple visits with your doctor are essential to monitor progress, wound healing, and ongoing heart health.
Individual recovery is influenced by overall health, the location of the procedure, and your adherence to post-procedure guidelines. Most patients see notable improvements within one to two weeks.
Success Rates and Effectiveness
Atherectomy is effective at restoring blood flow in appropriately selected patients. Success rates vary with factors like the size, location, and nature of the arterial blockage. According to recent studies:
- Atherectomy has a high technical success rate for removing significant blockages without open-heart surgery.
- Complications are rare when performed by an experienced team, especially when combined with lifestyle changes (e.g., diet, exercise, quitting smoking).
- Early intervention with atherectomy can decrease the likelihood of more invasive surgeries later in life.
Long-term outcomes depend on cardiovascular risk management and regular medical follow-up.
Preparing for an Atherectomy
Careful preparation ensures optimal safety and outcomes.
- Consultation and Testing: Your cardiologist will conduct a detailed review of medical history, medications, and results from previous diagnostic tests.
- Fasting: You may be instructed to avoid food and drink for several hours before the procedure.
- Medication Adjustments: Some blood thinners or diabetes medications may be halted or adjusted prior to surgery. Inform your team of all medicines and supplements.
- Consent and Questions: You’ll sign consent forms and have the opportunity to address any remaining concerns or questions with your healthcare providers.
Atherectomy Compared to Other Treatments
In some cases, alternative or adjunctive procedures may be considered, including:
- Angioplasty: A balloon attached to a catheter is inflated to widen narrowed arteries. Less effective for calcified or rigid plaque.
- Stenting: A mesh tube remains in place to keep the artery open, often used after atherectomy or angioplasty.
- Bypass Surgery: A surgical option to re-route blood around severely blocked arteries, reserved for the most complicated cases.
Your care team will recommend a treatment plan tailored to your specific needs and plaque characteristics.
Are There Limitations to Atherectomy?
Not every blockage can be treated with atherectomy. Limitations include:
- Unfavorable Anatomy: Small, tortuous, or highly branched arteries may not be suitable.
- Extensive Disease: Long segments of diffuse disease may be better treated with surgery.
- High Reblockage Risk: Some arterial beds are more likely to re-narrow, requiring ongoing monitoring.
Your doctor will explain if atherectomy is the optimal choice for your condition.
Frequently Asked Questions (FAQs)
Q: Does the atherectomy procedure hurt?
A: Most patients do not feel pain during the procedure due to local anesthesia and sedation. Some pressure or mild discomfort at the access site is possible but temporary.
Q: How long does the atherectomy procedure take?
A: The procedure typically lasts from 1 to 2 hours, depending on the complexity and number of blockages treated.
Q: How soon after atherectomy can I resume normal activities?
A: Light activity is often permitted within a few days. Your doctor will specify when it is safe to return to work, drive, or exercise based on your recovery.
Q: Will I need blood thinners after atherectomy?
A: Yes, many patients are prescribed blood thinners to help prevent blood clots and promote healing. Medication instructions should be followed precisely.
Q: Can the treated artery become blocked again?
A: There is always a risk of re-narrowing (restenosis), especially if risk factors are not managed. Regular check-ups and healthy lifestyle changes are essential for long-term artery health.
Q: Are there alternatives if I’m not a candidate for atherectomy?
A: Yes. Options like balloon angioplasty, stenting, or bypass surgery may be considered based on your specific disease pattern and medical history.
When to Contact Your Healthcare Provider
- If you notice severe bleeding, swelling, or pain at the incision site
- If you experience fever or signs of infection
- If you develop chest pain, difficulty breathing, or sudden weakness
Prompt communication helps address complications early and ensures the best recovery.
Key Takeaways
- Atherectomy is a minimally invasive technique to mechanically remove arterial plaque and restore blood flow.
- It is recommended for select patients with significant arterial disease not managed with medication alone.
- Risks are low but can include bleeding, vessel injury, or clotting; benefits often include rapid symptom relief and improved quality of life.
- Success depends on proper patient selection, post-procedure care, and ongoing lifestyle management.
References
- https://www.tgh.org/institutes-and-services/treatments/atherectomy
- https://www.medicalnewstoday.com/articles/atherectomy
- https://www.healthline.com/health/heart/atherectomy-heart-procedure
- https://uihc.org/services/atherectomy
- https://www.healthline.com/health/minimally-invasive-heart-procedures
- https://my.clevelandclinic.org/health/treatments/17310-pad-atherectomy
- https://stanfordhealthcare.org/medical-treatments/a/atherectomy.html
- https://texaseva.com/peripheral-artery-disease/diagnosis-treatment/atherectomy/
- https://www.ncbi.nlm.nih.gov/books/NBK499916/
Read full bio of medha deb












