Arteriovenous Malformations (AVMs): Causes, Symptoms, Diagnosis, and Treatment
Understand arteriovenous malformations (AVMs), their causes, risks, symptoms, diagnostic methods, and current treatment options.
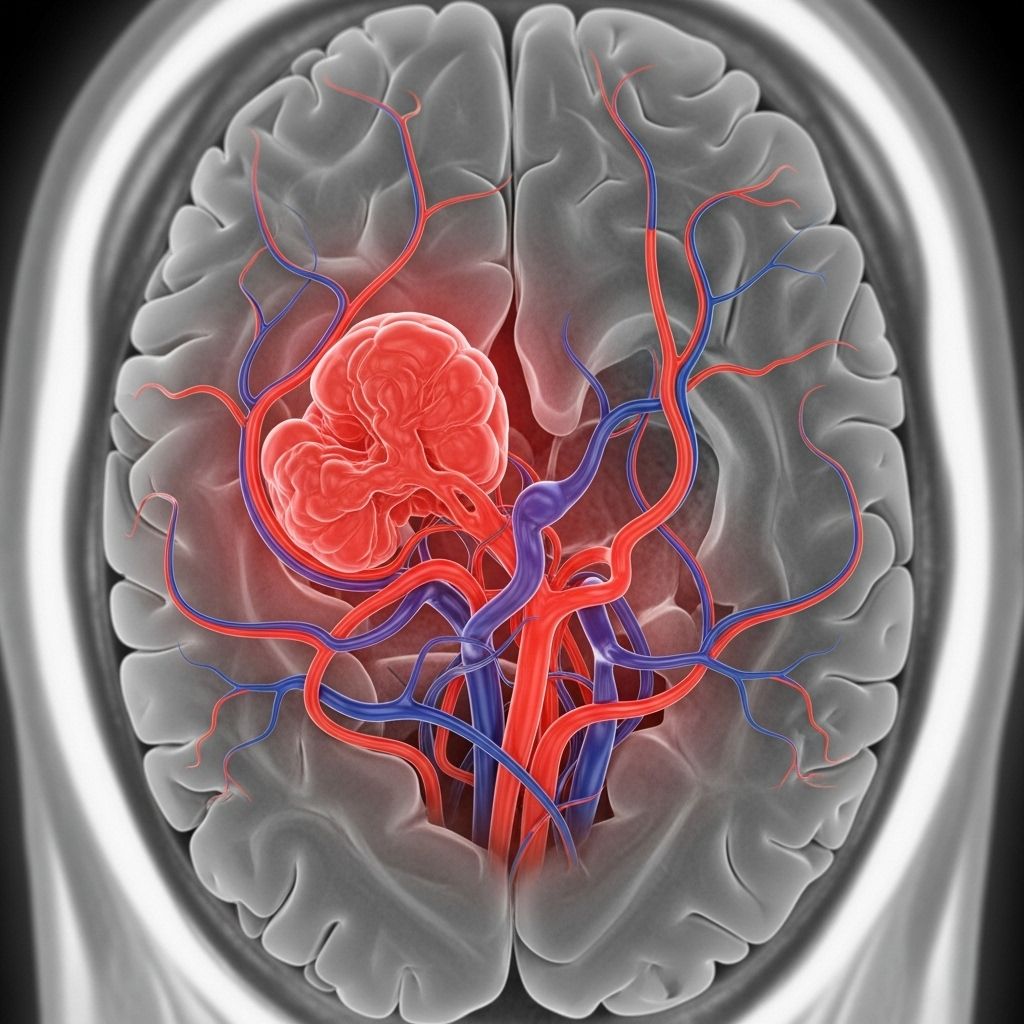
Arteriovenous malformations (AVMs) are uncommon but potentially serious blood vessel disorders characterized by abnormal connections between arteries and veins. Most frequently found in the brain and spinal cord, AVMs can occur elsewhere in the body and pose unique diagnostic and therapeutic challenges. This comprehensive guide explores what AVMs are, discusses their causes and risks, explains symptoms and diagnostic procedures, and covers current treatment approaches.
What is an Arteriovenous Malformation?
An arteriovenous malformation (AVM) is a tangled web of abnormal blood vessels where arteries—vessels carrying blood away from the heart—connect directly to veins—vessels returning blood to the heart—bypassing the capillary system.
This shortcut prevents blood from passing through the tiny capillaries where oxygen and nutrients are normally exchanged with tissues. As a result, some of the heart’s blood flow is wasted, returning to the heart before delivering its full supply to the body’s organs.
- AVMs can occur anywhere, but most commonly develop in the brain or spinal cord.
- AVMs may be present at birth (congenital) or develop later in life.
- They range in size, number, and location, greatly affecting their impact and treatment.
Why Do Arteriovenous Malformations Occur?
The precise cause of AVMs remains unclear in most cases. However, evidence suggests that most AVMs are congenital, forming during fetal development due to errors in the formation and differentiation of blood vessels.
- AVMs are rarely inherited, but syndromes with genetic links such as hereditary hemorrhagic telangiectasia can increase risk.
- There is currently no evidence that AVMs develop from lifestyle factors or accidents.
Though the exact genetic or environmental factors are not well understood, research is ongoing.
Who is at Risk for AVMs?
While AVMs occur in both children and adults, certain factors may increase risk:
- Congenital factors: Most AVMs exist at birth.
- Family history: Some rare, inherited disorders raise the risk, but most cases have no identifiable family link.
- Gender: AVMs are slightly more common in males than females.
Symptoms of Arteriovenous Malformations
The symptoms of an AVM depend on its size, location, and whether it has ruptured. Many people experience no symptoms until complications develop, particularly when AVMs are small or situated in less critical areas. When present, symptoms can include:
- Headaches: May be chronic or sudden and severe if associated with bleeding.
- Seizures: Particularly common with brain AVMs.
- Nausea and vomiting
- Weakness or numbness: Loss of muscle strength or sensation, often on one side of the body.
- Paralysis: Loss of movement in body parts affected by the AVM’s location.
- Loss of coordination: Difficulty with balance and walking.
- Speech or language problems: Trouble speaking or understanding language if the AVM is in the brain.
- Visual changes: Partial loss of vision, double vision, or swelling of the optic nerve.
- Confusion or memory loss: Especially with brain involvement.
- Back pain or stiffness of neck: With spinal cord AVMs.
- Bleeding: Including life-threatening brain hemorrhages.
- Pulsating masses and warmer skin: In AVMs closer to the surface or outside the nervous system.
- Swelling: At or near the site of the AVM.
Symptoms in Children
AVMs in children may present with:
- Birthmarks (pink, red, or purple) over the AVM
- Unusual warmth or a visible pulse over the area
- Pain, swelling, or uncontrollable bleeding
- Learning or behavioral difficulties, in rare cases
Symptoms of the Vein of Galen Malformation
A special type, the vein of Galen malformation, occurs deep inside the brain and usually presents at or soon after birth. Symptoms can include:
- Bulging scalp veins
- Enlarged head due to brain fluid buildup
- Seizures
- Failure to thrive
- Signs of congestive heart failure
Complications and Risks of AVMs
AVMs can be dangerous, with risks tied closely to their location, size, and whether they’ve bled. Key complications include:
- Hemorrhage (bleeding): The highest risk, especially for brain AVMs. Bleeding can rapidly cause stroke-like symptoms or be fatal.
- Reduced oxygen delivery: The abnormal blood flow may deprive brain or spinal cord tissues of oxygen, causing gradual neurological problems.
- Seizures, headaches, and neurological loss: Persistent or progressive symptoms are possible even without bleeding.
- Chronic pain: Especially in AVMs outside the brain.
- Heart failure: Large AVMs can overwork the heart, especially in infants, by creating high blood flow that the heart must accommodate.
- Paralysis: When spinal cord AVMs bleed or compress nerves.
Bleeding from an AVM, especially in the brain, is a medical emergency requiring immediate attention.
Diagnosing Arteriovenous Malformations
AVMs are often suspected following neurological symptoms such as seizures, sudden severe headache, or unexplained neurological deficits. Many AVMs are found incidentally during imaging for unrelated reasons.
Diagnostic Process
- Medical history and physical examination: A neurologist or relevant physician will inquire about symptoms, family history, and perform a focused examination. They may listen for a bruit—a whooshing sound caused by rapid blood flow through an AVM.
- Imaging tests: The mainstays of AVM diagnosis include:
- CT (Computed Tomography) scan: Can reveal bleeding or abnormalities in structure.
- MRI (Magnetic Resonance Imaging): Highly sensitive for detecting AVMs and assessing effects on the brain or spinal cord.
- Ultrasound: More common for AVMs outside the brain and spinal cord.
- Cerebral angiography: Considered the gold standard for diagnosing and mapping AVMs. A dye is injected into the bloodstream to visualize blood flow in the brain or spinal cord on X-ray images.
Treatments for Arteriovenous Malformations
Management of AVMs is highly individualized, depending on the malformation’s:
- Size
- Location
- Patient’s symptoms
- Risk of bleeding
- Patient’s overall health
Observation and Medical Management
- Monitoring: Small, asymptomatic AVMs may be monitored for changes or signs of increased bleeding risk.
- Medications: Used to manage symptoms such as headaches, seizures, or pain. AVMs themselves cannot be removed with medicine alone.
Definitive Interventions
- Microsurgical removal: Surgical resection is considered when the AVM is accessible and the expected benefit outweighs the risk. This offers the possibility of cure, but surgery can be complex, especially for deep or large AVMs.
- Endovascular embolization: A minimally invasive procedure in which a catheter is threaded through blood vessels to the AVM, and a substance is injected to block abnormal blood flow. This is sometimes used before surgery or radiosurgery, or in rare cases as sole treatment.
- Stereotactic radiosurgery: Highly focused radiation beams target the AVM, causing it to shrink over time. This non-surgical option is preferred for deep or small AVMs.
- In many cases, a combination of therapies is required for optimal management.
Note: The choice of treatment should be guided by a multidisciplinary medical team experienced in AVM care, considering both risks and potential benefits.
Living With and Monitoring AVMs
Living with an AVM requires careful monitoring and ongoing care, particularly for individuals whose AVMs are not immediately removed or treated. Key considerations include:
- Regular follow-up imaging to detect growth or changes
- Prompt reporting of new symptoms such as headaches, weakness, vision changes, or seizures
- Management of secondary complications (e.g., anemia from bleeding, neurological losses)
- For children and teens, management of any learning, behavioral, or developmental issues
When to Seek Medical Help
Seek urgent medical attention if any of the following occur:
- Sudden and severe headache—the worst of your life
- Loss of consciousness
- Seizures or sudden neurological changes (weakness, numbness, vision loss)
- Signs of stroke (facial droop, arm weakness, speech difficulties)
Even in the absence of symptoms, individuals diagnosed with an AVM should remain in regular contact with their healthcare provider.
Frequently Asked Questions (FAQs)
What causes arteriovenous malformations?
Most AVMs develop during fetal development for reasons that are not fully understood. Though some can be linked to genetic conditions, most are not inherited or caused by lifestyle factors.
Can AVMs be prevented?
No known measures can prevent AVMs since they are usually present at birth and rarely linked to preventable factors.
How serious is an AVM?
Severity depends on size, location, and risk of bleeding. AVMs in the brain or spinal cord are serious and can cause life-threatening complications if they bleed.
Is surgical treatment always required?
No. Some AVMs may be managed with observation and medical therapy if the risks of intervention outweigh the benefits, especially for small, stable, or symptom-free AVMs.
What is the outlook after AVM treatment?
Many individuals lead healthy lives after AVM treatment or successful monitoring. Prognosis depends on the severity of complications before treatment and the AVM’s response to intervention.
Key Facts Table: Summary of AVM Information
| Characteristic | Details |
|---|---|
| Definition | Abnormal tangle of arteries and veins with direct connections, bypassing capillaries |
| Most Common Locations | Brain, spinal cord, less commonly other organs |
| Major Risks | Bleeding (hemorrhage), stroke, neurological loss |
| Main Symptoms | Seizures, headache, weakness, speech or vision loss, paralysis |
| Diagnosis | CT scan, MRI, ultrasound, cerebral angiography |
| Treatments | Observation, medication, surgery, embolization, radiosurgery |
| Prognosis | Varies: Good if managed before bleeding; more guarded if complications occur |
Latest Medical Recommendations
- If diagnosed with an AVM, consult with a neurologist, neurosurgeon, or interventional radiologist experienced in AVM management.
- Engage in shared decision-making for optimal treatment strategy, considering risks, benefits, and personal preferences.
- Report any new symptoms promptly; rapid intervention for bleeding or neurological changes is critical.
References and Additional Resources
- National Institute of Neurological Disorders and Stroke
- American Stroke Association
- Mayo Clinic
- KidsHealth
- Penn Medicine
References
- https://www.mayoclinic.org/diseases-conditions/arteriovenous-malformation/symptoms-causes/syc-20350544
- https://kidshealth.org/en/parents/arteriovenous-malformations.html
- https://medlineplus.gov/arteriovenousmalformations.html
- https://www.pennmedicine.org/conditions/arteriovenous-malformations-avm
- https://www.mayoclinic.org/diseases-conditions/brain-avm/symptoms-causes/syc-20350260
- https://my.clevelandclinic.org/health/diseases/16755-arteriovenous-malformation-avm
- https://stanfordhealthcare.org/medical-conditions/brain-and-nerves/arteriovenous-malformation/symptoms.html
- https://lluh.org/conditions/arteriovenous-malformations
Read full bio of medha deb












