Arterial Embolization for Kidney Cancer: Methods, Uses, and Recovery
Arterial embolization is a minimally invasive option to shrink kidney tumors and relieve symptoms when surgery is not possible.
Arterial Embolization: Noninvasive Treatment for Kidney Cancer
Arterial embolization is an advanced, minimally invasive procedure designed to disrupt the blood supply to kidney tumors. By targeting nutrient pathways, this technique helps shrink both benign and malignant tumors, improving quality of life for people who are not eligible for surgical removal of the kidney.
What Is Arterial Embolization?
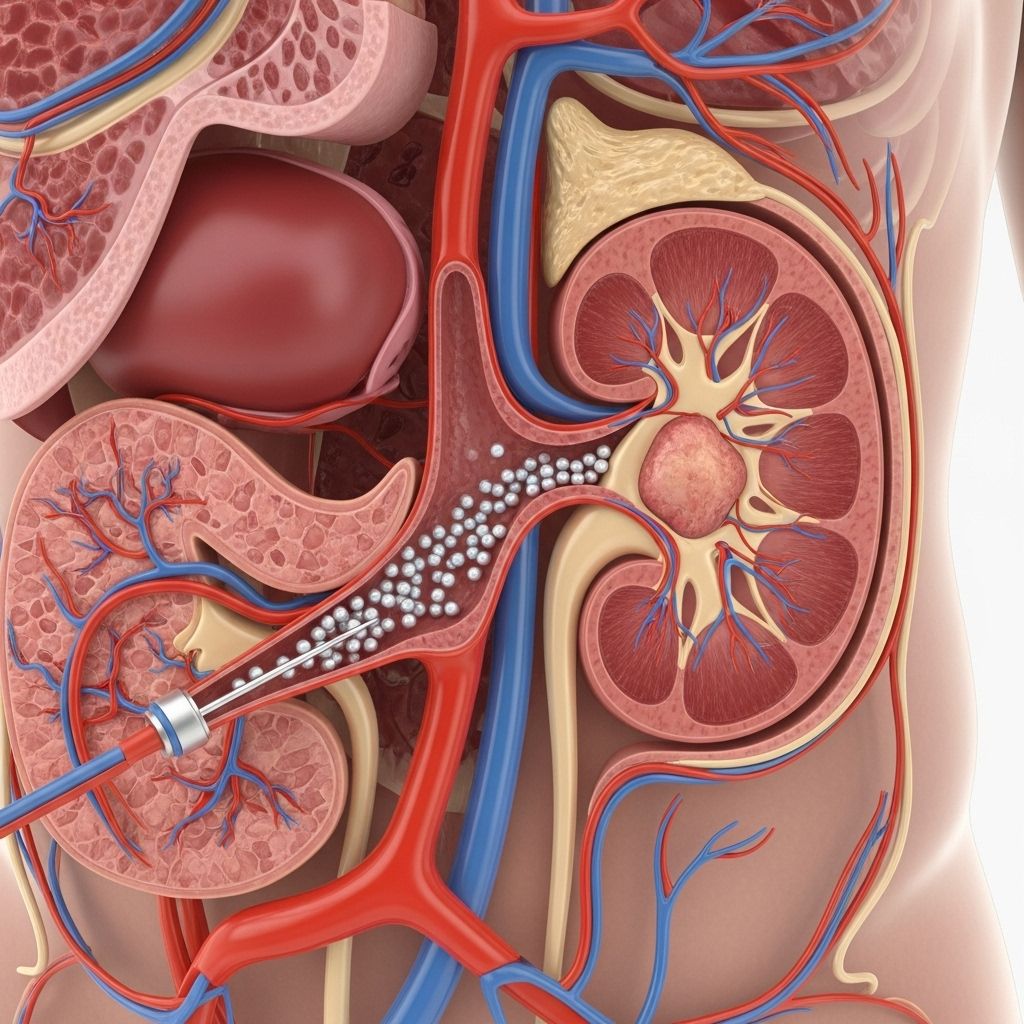
Arterial embolization—sometimes referred to as transarterial embolization—uses medical devices and agents to block specific arteries that supply blood to a kidney tumor. This process deprives the tumor of nutrients and oxygen, causing it to shrink over time rather than being surgically removed. While not a cure when used alone, embolization can be a crucial part of cancer management.
- Minimally invasive approach with fewer risks than major surgery
- Used for both cancerous and benign (noncancerous) tumors
- May precede surgery or act as palliative care in advanced stages
- Often performed under sedation or local anesthesia
How Does Arterial Embolization Work?
Kidney tumors rely on a network of blood vessels to thrive. Interventional radiologists target those vessels, delivering embolic materials that block circulation. Over the weeks following the procedure, tumor cells begin to die or shrink as their supply of oxygen and nutrients is removed.
- Blood flow is interrupted by inserting a catheter into a kidney artery
- Embolic agents (such as ethanol, microspheres, or gelatin sponges) plug the vessel
- Tumor gradually shrinks without direct removal
- Does not destroy healthy kidney tissue surrounding the tumor
- May also relieve pain and bleeding symptoms in kidney cancer patients
Uses of Arterial Embolization in Kidney Tumors
- Benign Tumor Treatment: Frequently applied to shrink noncancerous angiomyolipoma tumors, which contain fat and muscle tissue.
- Malignant Tumor Treatment: For patients with advanced, metastatic, or inoperable kidney cancer.
- Palliative Care: Relieves pain, bleeding, or other symptoms when surgery isn’t appropriate.
- Preoperative Use: Sometimes used before surgery to reduce the risk of heavy bleeding and make surgical tumor removal easier.
- Treatment in Genetic Disorders: Used for tumors associated with rare genetic conditions, like tuberous sclerosis.
Who Benefits from Arterial Embolization?
- Individuals too ill for major kidney surgery
- Patients with large, difficult-to-access tumors
- People experiencing severe symptoms, including pain or bleeding
- Those with benign angiomyolipoma tumors causing or at risk for kidney failure
Kidney Tumors Commonly Treated
| Tumor Type | Treatment Purpose | Notes |
|---|---|---|
| Renal Cell Carcinoma | Shrinking tumor, palliative symptoms, sometimes preoperative | Most common malignant kidney cancer |
| Angiomyolipoma | Reduce bleeding risks, limit growth, prevent rupture | Benign, seen in tuberous sclerosis |
| Metastatic Kidney Tumors | Palliative pain control, symptom management | Advanced cancer spreading beyond the kidney |
Procedure Details: What to Expect
Arterial embolization procedures are typically performed in hospitals under the guidance of experienced interventional radiologists. Preparation and recovery steps are designed for safety and comfort.
Step-by-Step Overview
- Preparation: You may be instructed to fast, stop certain medications, and undergo imaging studies like CT or MRI.
- Sedation: Local anesthesia or conscious sedation is administered to ensure comfort.
- Catheterization: A thin, flexible tube (catheter) is inserted into a blood vessel, typically in the groin, then guided up to the renal artery.
- Delivery of Embolic Material: Gelatin sponges, microspheres, or alcohol solutions block blood flow in arteries that feed the tumor.
- Verification: Imaging confirms that blood flow is halted.
- Recovery: Catheter is removed, and you are observed for several hours (sometimes overnight).
- Average procedure time: 30–90 minutes
- Most patients go home the same or next day
- Follow-up imaging may be scheduled to check tumor response
Risks and Potential Side Effects
Like any medical intervention, arterial embolization has risks and possible side effects. However, it is often better tolerated than open surgery, especially for patients who are not surgical candidates.
- Pain or discomfort at the catheter entry site
- Post-embolization syndrome: Low-grade fever, mild pain, nausea for a few days
- Rare complications include infection, allergic reactions, and unintended damage to healthy tissue
- Blood clot formation or kidney injury (rare)
Managing Risks
- Careful selection of embolic agents and imaging guidance helps protect healthy kidney tissue
- Most side effects are temporary and manageable
- Close observation and prompt care for any unexpected symptoms
Recovery Following Arterial Embolization
Most patients experience only mild discomfort or fatigue after arterial embolization. Recovery steps focus on rest, monitoring, and self-care.
- Bruising or tenderness at the catheter site may occur
- Mild fever and pain typically subside within a few days
- Avoid strenuous activity for several days
- Drinking fluids and adhering to post-procedure instructions helps promote healing
- Follow-up appointments may include repeat imaging or bloodwork
Tips for Recovery
- Rest for the first 24–48 hours post-procedure
- Monitor for symptoms: persistent pain, high fever, swelling, or bleeding warrant prompt medical attention
- Take medications for pain or fever as directed
- Maintain good nutrition and hydration
Long-Term Outlook and Prognosis
Arterial embolization is often used as part of a comprehensive treatment plan. Tumor shrinkage can make subsequent surgery easier, reduce symptoms, and in some cases improve kidney function. However, embolization is not curative on its own and may require follow-up therapy.
- Tumor reduction is typically seen in weeks to months, not immediately
- Some patients require repeat procedures or additional cancer therapy
- Prognosis varies based on tumor type, size, and overall health
- Relief from pain and bleeding can significantly improve quality of life
Frequently Asked Questions (FAQs)
Q: Is arterial embolization painful?
A: Most patients experience minimal pain during the procedure, thanks to sedation and anesthesia. Mild discomfort may occur afterwards at the entry site or in the back.
Q: How soon will I feel relief from my kidney tumor symptoms?
A: Symptom relief—such as less pain or bleeding—often begins within days, but tumor shrinkage may take several weeks.
Q: Does embolization cure kidney cancer?
A: No, arterial embolization is not a cure for kidney cancer when used alone. It is intended for symptom relief, tumor shrinkage, and as a palliative measure, especially for patients unable to undergo curative surgery.
Q: What are angiomyolipomas, and why are they treated with embolization?
A: Angiomyolipomas are benign kidney tumors made of fat and muscle. Large ones can bleed or cause kidney failure. Embolization helps shrink them and reduce such complications.
Q: How is embolization different from surgery?
A: Surgery involves direct removal of a tumor or kidney (nephrectomy), while embolization works by blocking blood supply and shrinking the tumor indirectly.
Q: What should I watch for after the procedure?
A: Look for signs like persistent pain, fever over 101°F (38.3°C), swelling, bleeding, or redness at the catheter site. Contact your healthcare provider promptly if these occur.
Key Takeaways About Arterial Embolization for Kidney Cancer
- Minimally invasive and often well-tolerated, especially for complex or inoperable cases
- Vital for palliative symptom control and management of benign tumors like angiomyolipomas
- Not a stand-alone cure, but a supportive therapy as part of overall cancer care
- Recovery is usually quick, but regular follow-up is needed
- Talk to your doctor about suitability based on health and tumor characteristics
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4272833/
- https://www.healthline.com/health/kidney-cancer/embolization-kidney-cancer
- https://cancer.ca/en/cancer-information/cancer-types/kidney/treatment/arterial-embolization
- https://americanjir.com/combined-transarterial-embolization-and-percutaneous-image-guided-ablation-for-the-treatment-of-t1b-and-central-renal-tumors-in-patients-with-high-surgical-risk/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3930649/
- https://www.cancerresearchuk.org/about-cancer/kidney-cancer/treatment/renal-artery-embolisation
- https://www.cedars-sinai.org/programs/imaging-center/exams/interventional-radiology/kidney-embolization.html
- https://stanfordhealthcare.org/medical-conditions/cancer/kidney-cancer/kidney-cancer-treatments/arterial-embolization.html
- https://www.masseycancercenter.org/cancer-types-and-treatments/cancer-types/kidney-cancer/treatment/
Read full bio of medha deb












