Arrhythmogenic Right Ventricular Cardiomyopathy: Understanding, Diagnosis, and Treatment
Comprehensive guide to ARVC: Explore causes, symptoms, diagnosis, and modern treatment strategies for this rare but serious heart condition.
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
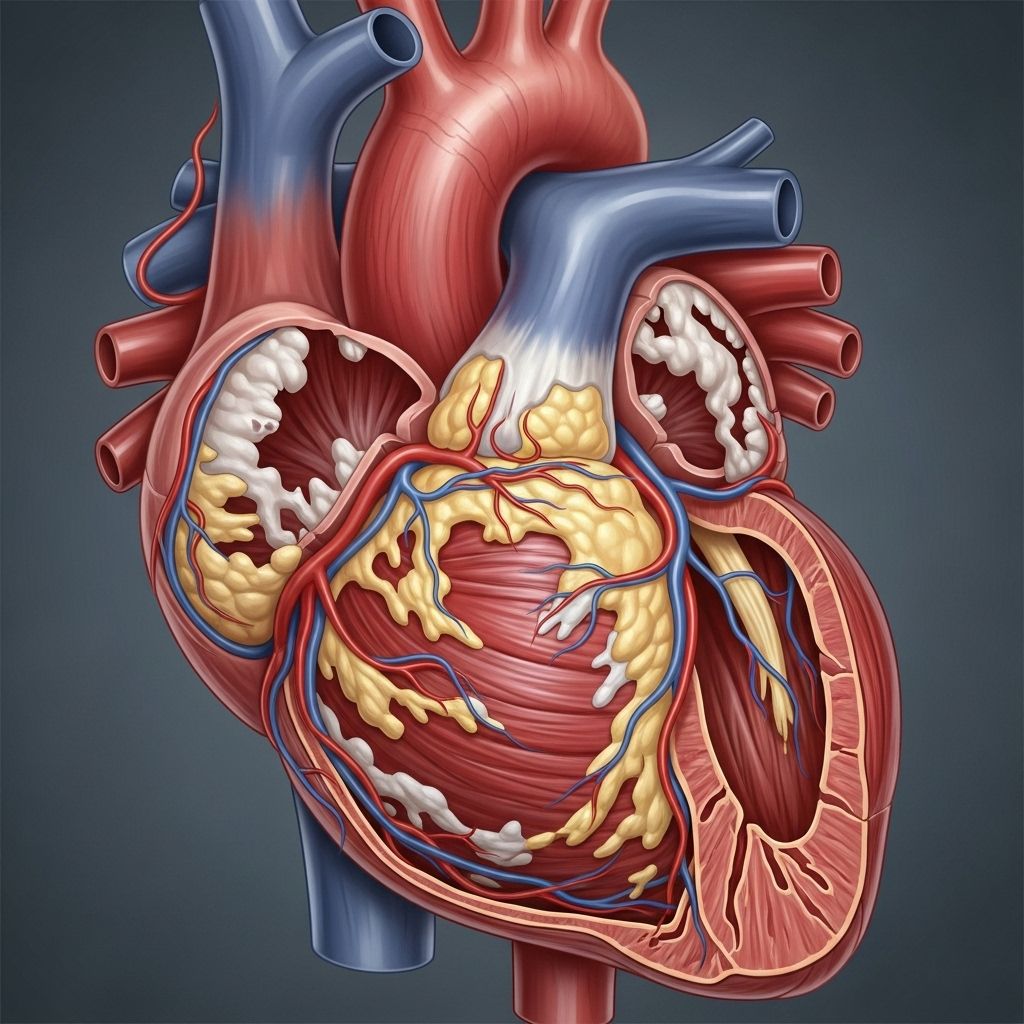
Arrhythmogenic right ventricular cardiomyopathy (ARVC), sometimes called arrhythmogenic right ventricular dysplasia (ARVD), is a rare condition where the muscle tissue in your right ventricle is replaced by scar and fat, potentially disrupting the heart’s rhythm and function. This disease places individuals at an increased risk of arrhythmias, heart failure, and sudden cardiac death, especially in young adults and athletes. Understanding ARVC is vital for early detection and effective management.
What is Arrhythmogenic Right Ventricular Cardiomyopathy?
ARVC is a genetic heart disease that affects the myocardium—the muscular wall of the heart—primarily targeting the right ventricle. Over time, normal heart muscle is gradually replaced by fatty or fibrous tissue, weakening the ventricular muscle and disrupting the normal flow of electrical signals in the heart. This makes affected individuals susceptible to potentially life-threatening arrhythmias and eventually, heart failure.
Alternate names include:
- Arrhythmogenic right ventricular dysplasia (ARVD)
- Arrhythmogenic cardiomyopathy (ACM) (when left ventricle is involved)
Main Characteristics of ARVC
- Progressive replacement of heart muscle with fatty or fibrous tissue.
- Predominantly affects the right ventricle but can involve both ventricles.
- Leads to electrical instability, abnormal heart rhythms, and diminished pumping capacity.
- Symptoms often first appear in people aged 10–50, but it can be undetected for years.
How Common Is ARVC?
ARVC is considered a rare disease, occurring in about 1 in 1,000 to 1 in 1,250 people globally and fewer than 200,000 cases in the United States. However, it is likely underdiagnosed because the symptoms can be subtle or mistaken for other cardiac conditions. ARVC remains a leading cause of sudden cardiac death in young athletes and adults.
Causes of ARVC
The development of ARVC is mainly attributed to genetic mutations affecting proteins responsible for attaching heart muscle cells (called desmosomes). Disruption of these proteins weakens the cell connections, making cells prone to injury, especially during exercise, and leading to their replacement by fat and scar tissue.
- Inherited condition: Most cases are inherited in an autosomal dominant pattern. This means that just one copy of the altered gene from either parent may cause the disorder.
- Multiple genes are implicated, though some remain unidentified, and new mutations may occur spontaneously.
Environmental and Lifestyle Factors
- Intensive physical activity (especially endurance sports) may accelerate disease progression and brings on symptoms earlier, particularly in genetically predisposed individuals.
- Some non-genetic factors, such as certain viral infections or inflammation, might influence disease development, but these are rare.
Symptoms of ARVC
Symptoms of ARVC may be absent in early stages, but with disease progression, the heart’s impaired structure manifests through a range of clinical symptoms. Sometimes, the first noticeable sign is a life-threatening arrhythmia or sudden cardiac arrest, particularly in young people or athletes.
- Palpitations: Feeling like the heart is fluttering, racing, skipping beats, or pounding in the chest.
- Lightheadedness or dizziness
- Shortness of breath
- Fainting spells (syncope): Especially after exercise.
- Chest pain
- Swelling: In the feet, legs, ankles, or abdomen—more often seen at advanced stages due to heart failure.
- Fatigue
Symptoms often emerge during adolescence to early adulthood, and men are more frequently affected than women. Some individuals may never develop symptoms but can still be at risk for life-threatening events.
When to Seek Medical Help
- If you feel sudden, severe chest pain, or if someone collapses or passes out unexpectedly, call emergency services immediately.
- Frequent unexplained palpitations, dizziness, or fainting should prompt a medical evaluation, especially if there’s a family history of unexplained sudden death or ARVC.
Diagnosis of ARVC
Diagnosing ARVC can be challenging because its features can resemble other heart conditions. A combination of tests and evaluation criteria are used, often following international Task Force criteria.
Key Diagnostic Steps
- Medical and Family History: Assessing for family members with ARVC, sudden cardiac death, or unexplained syncope.
- Physical Examination: Checking for abnormal heart rhythms and signs of heart failure.
- Electrocardiogram (ECG or EKG): Detects abnormal rhythms and electrical activity suggestive of ARVC.
- Holter Monitoring: Portable ECG worn for 24–48 hours (or longer) to record ongoing rhythm disturbances.
- Echocardiogram: Ultrasound imaging of the heart reveals changes in size, movement, and function of the right ventricle.
- Cardiac MRI: Provides detailed images showing fat and scar tissue replacing the myocardium.
- Genetic Testing: Identifies mutations associated with ARVC, potentially benefiting family members.
- Endomyocardial Biopsy: Rare, but may be used to obtain tissue for analysis.
Task Force Criteria for Diagnosis
Doctors may use a set of major and minor criteria, including clinical symptoms, family history, ECG findings, and cardiac imaging, to classify ARVC as possible, borderline, or definitive.
| Test/Exam | What it Looks For | Role in Diagnosis |
|---|---|---|
| EKG/Holter Monitor | Abnormal heart rhythms | Detects arrhythmias and monitoring for irregular beats |
| Echocardiogram | Structure and movement of the heart | Assesses right ventricle for abnormalities |
| Cardiac MRI | Fat and scar tissue in heart muscle | Visualizes damaged or inflamed areas |
| Genetic Testing | Specific gene mutations | Confirms hereditary risk in family members |
Risk Factors for ARVC
- Genetic predisposition: Having a first-degree relative with ARVC greatly increases risk.
- Intense and prolonged physical activity: High-level athletes, especially in endurance sports, are more likely to develop symptoms at an earlier age if genetically predisposed.
- Age: Adolescents and young adults are at highest risk for sudden symptoms and cardiac events.
Complications
ARVC is progressive, meaning its effects can worsen over time and lead to serious complications if not managed:
- Ventricular arrhythmias: Abnormal, rapid heart rhythms originating in the ventricles. The most serious, such as ventricular tachycardia or ventricular fibrillation, can cause fainting or sudden death if untreated.
- Sudden cardiac arrest: Can occur without warning, especially during or immediately after intense physical exertion.
- Progressive heart failure: As the muscle is replaced by scar and fat, the pumping ability declines, leading to symptoms such as swelling and weakness.
Treatment Options for ARVC
There is no cure for ARVC, but early identification and treatment can significantly improve quality of life and reduce the risk of sudden cardiac death. Treatment focuses on reducing arrhythmia risk, controlling symptoms, and slowing disease progression.
Core Treatments
- Lifestyle modifications: Limiting or avoiding intense physical activity, especially competitive sports.
- Medications: Such as beta-blockers and antiarrhythmic drugs, to help control heart rate and reduce arrhythmia risk.
- Implantable devices: Most commonly, an implantable cardioverter defibrillator (ICD) is recommended for those at high risk of life-threatening arrhythmias.
- Catheter ablation: A procedure using radiofrequency to destroy small areas of heart tissue responsible for abnormal rhythms. Used in select cases not well controlled by medications.
- Heart transplant: In advanced stages with severe heart failure unresponsive to all other treatments.
Lifestyle Changes
Making healthy choices can help reduce the risk of complications and improve overall well-being:
- Adhering to medication and treatment plans
- Attending regular follow-ups with a cardiologist specialized in inherited heart conditions
- Refraining from high-intensity and competitive sports
- Maintaining a heart-healthy diet
- Managing other cardiovascular risk factors like high blood pressure or cholesterol when present
Prognosis
The outlook for ARVC varies. Some individuals experience only mild symptoms and live normal lifespans, while others are at high risk for severe complications. Earlier diagnosis, adherence to treatment, and lifestyle adjustments can significantly lower the risk of sudden cardiac death and slow progression to heart failure.
- The average age at diagnosis is around 30 years old.
- Cardiac arrest risk is highest in those under 25 years old, particularly if the disease is not diagnosed and managed early.
Living with ARVC
Being diagnosed with ARVC can be life-altering. Emotional support, regular doctor visits, and careful monitoring are important, both for individuals and their families. Genetic counseling is strongly advised for those with ARVC and their first-degree relatives.
- Psychological support or patient communities can help with adjustment.
- Family screening and preventive strategies may reveal others at risk before major symptoms appear.
Frequently Asked Questions (FAQs)
Q: Can ARVC be prevented?
A: ARVC is primarily caused by inherited genetic mutations. While you cannot prevent the gene changes that cause ARVC, early detection and lifestyle modification can help reduce risks and improve outcomes.
Q: Is exercise safe if I have ARVC?
A: Most experts recommend avoiding competitive sports and intense endurance activities, as they can worsen symptoms and increase the risk of sudden death, especially if you have a diagnosis or family history of ARVC.
Q: Should my family members be tested?
A: Yes, genetic testing and cardiac screening for first-degree relatives (parents, siblings, children) of someone with ARVC are highly recommended to identify those at risk and begin monitoring or preventative care.
Q: Can children get ARVC?
A: While ARVC typically presents symptoms between ages 10 and 50, it can occur in children and young adults, especially those with a family history.
Q: Does ARVC only affect the right ventricle?
A: ARVC usually affects the right ventricle but can sometimes involve both right and left ventricles—this is referred to as arrhythmogenic cardiomyopathy (ACM).
Summary
Arrhythmogenic right ventricular cardiomyopathy is a rare but serious inherited heart condition. It is a leading cause of sudden cardiac death in young people and athletes, but with modern medical care, early diagnosis, lifestyle changes, and proper treatment, many can lead fulfilling lives. Family awareness and screening play a major role in reducing tragic outcomes. If you experience symptoms such as unexplained palpitations or fainting, especially with a family history of heart disease or sudden death, consult a healthcare professional promptly.
References
- https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/arrhythmogenic-right-ventricular-dysplasia-cardiomyopathy/symptoms.html
- https://cvrti.utah.edu/recognizing-early-signs-of-arvc-cardiomyopathy/
- https://www.pennmedicine.org/conditions/arrhythmogenic-cardiomyopathy
- https://medlineplus.gov/genetics/condition/arrhythmogenic-right-ventricular-cardiomyopathy/
- https://arvcstudies.com/about-arvc/
- https://pubmed.ncbi.nlm.nih.gov/26498164/
- https://my.clevelandclinic.org/health/diseases/16752-arrhythmogenic-right-ventricular-dysplasia-arvd
- https://www.bhf.org.uk/informationsupport/conditions/arrhythmogenic-cardiomyopathy
Read full bio of Sneha Tete












