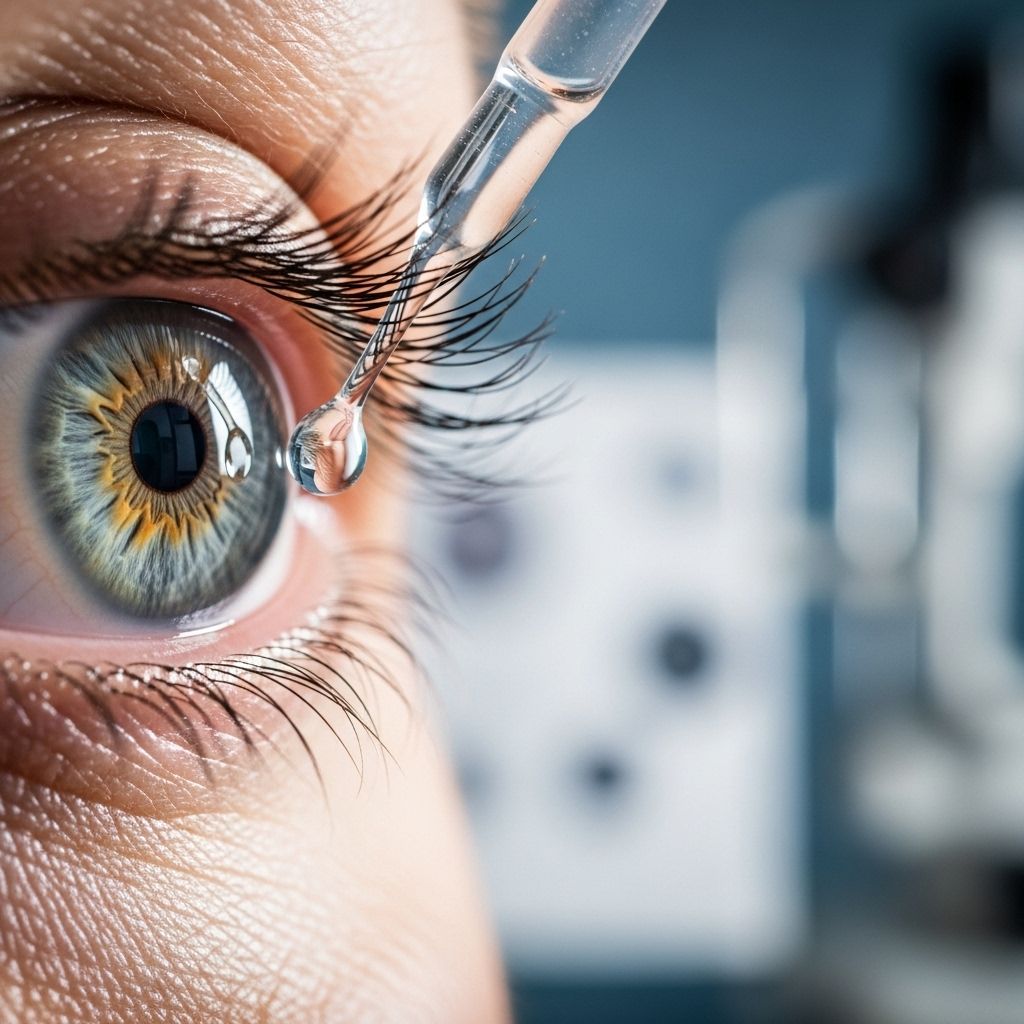
How to Know If Your Glaucoma Eye Drops Are Working
Get expert guidance on recognizing when glaucoma eye drops aren’t working and how to maintain lasting vision health.
How Do You Know If Glaucoma Eye Drops Aren’t Working?
Glaucoma is a chronic eye disease that can cause vision loss due to damage to the optic nerve. One of the most common methods of managing glaucoma is through medicated eye drops designed to lower intraocular pressure (IOP). However, it’s vital to know if these drops are effective and recognize signs that treatment may no longer be working as intended. Close collaboration with your ophthalmologist is essential for preserving your vision in the long term.
About Glaucoma and Eye Drops
Glaucoma is best managed through early intervention and consistent treatment. While damage caused by glaucoma cannot be reversed, using eye drops can help slow down or even halt the progression of the disease.
Eye drops for glaucoma are typically prescribed as a first-line treatment due to their non-invasive nature and ability to control eye pressure effectively. However, using these drops requires lifelong adherence to ensure long-term results, as missed doses can increase the risk of worsening symptoms and irreversible vision loss.
How Glaucoma Eye Drops Work
Glaucoma eye drops are formulated to lower intraocular pressure (IOP), which is the most significant risk factor for glaucoma progression. These medications act in several different ways to maintain healthy eye pressure:
- Decreasing fluid production: Some ingredients in eye drops reduce the production of aqueous humor, the fluid within the eye, which lowers pressure.
- Improving fluid drainage: Other medications focus on increasing the drainage of this fluid, helping the eye get rid of excess liquid and thus reducing pressure.
- Combination medications: A number of eye drops combine both mechanisms—reducing fluid production and enhancing drainage—for enhanced IOP control.
The Need for a Strict Routine
Using glaucoma eye drops is a lifelong commitment. Many people need to use them once or more each day, and missing doses can seriously compromise treatments. Stopping eye drops without consulting a doctor can lead to a dangerous rise in eye pressure and potentially rapid vision loss.
Types of Glaucoma Eye Drops
Several classes of medications are available as eye drops to treat glaucoma, each targeting IOP through different mechanisms. Here’s a summary of the most common types and their unique features:
| Medication Type | How It Works | Common Side Effects |
|---|---|---|
| Prostaglandins | Increases the outflow of aqueous humor, reducing eye pressure. Usually used once daily before bedtime. | Eye redness, eyelash growth, iris color change, pigmentation. |
| Rho kinase inhibitors | Reduces fluid production and improves drainage (e.g. netarsudil). | Eye redness. |
| Nitric oxides | Boosts fluid outflow through the trabecular meshwork (e.g. latanoprostene bunod). | Eye redness, possible risk of depression, allergic contact dermatitis. |
| Miotic/cholinergic agents | Constricts the pupil to open drainage pathways, improving fluid outflow (e.g. pilocarpine). | Eyebrow pain, pupil shrinkage (side effects are stronger with oral form). |
| Beta-blockers | Decreases fluid production (e.g. timolol). Typically used once or twice daily. | Eye pain, eye infections, swollen eyelids; may not be suitable for people with asthma or COPD. |
Recognizing When to Reevaluate Your Eye Drops
Patients may reach a point where their
eye drops do not seem to be working
as effectively. Sometimes, signs of progression are subtle and easy to miss, especially if vision changes occur slowly. Nevertheless, monitoring for certain symptoms and changes is crucial, as early detection of treatment failure can prevent severe vision loss.- Elevated intraocular pressure (IOP): Even with treatment, your eye pressure may rise again, indicating that the medication is no longer controlling IOP effectively.
- Progression of visual field loss: If you notice worsening blind spots, patches in your vision, or trouble seeing at the edges, this could indicate your drops need adjustment.
- Optic nerve damage: Although you can’t see this directly, your ophthalmologist can monitor optic nerve health using specialized testing and imaging.
- New or increased symptoms: If you experience eyestrain, frequent headaches, noticeable changes in vision, more floaters, or patches clouding your sight, you should seek immediate advice from your eye doctor.
Any of these signs can signal the need to reevaluate your treatment. Since many symptoms of glaucoma are gradual, regular visits to an eye care professional are critical for detecting subtle changes and preventing irreversible damage.
What If You’re Not Taking Eye Drops as Prescribed?
One common issue in glaucoma management is medication adherence. Daily use of eye drops can be difficult due to busy schedules, forgetfulness, or even discomfort from the drops themselves. Yet, missing doses can undermine the effectiveness of your treatment. In addition:
- Incorrect technique in administering drops can also reduce effectiveness, leaving a significant portion of patients undertreated even if they believe they’re compliant.
- Ineffective self-instillation has been directly linked to higher risk of progression and even need for surgical intervention.
- People who unintentionally miss getting a drop into their eye (for example, letting it run down their cheek or blink it away) are at greater risk of disease progression or the need for further procedures.
If you struggle with your medication routine, contact your ophthalmologist for advice or ask about techniques and tools (such as eye drop applicators) that can help improve your accuracy and consistency.
Steps to Take If Eye Drops Seem Less Effective
If you have any indication that your current drops aren’t controlling your glaucoma, promptly contact your ophthalmologist for an in-depth evaluation. Testing helps distinguish between medication failure, incorrect usage, or normal changes that require a different treatment approach. Here’s what to expect during an evaluation:
- Measurement of intraocular pressure (IOP) to detect elevations.
- Visual field testing, usually involving looking at blinking lights to determine if there are new or expanding areas of blindness or vision loss.
- Optic nerve imaging and assessment for structural changes that indicate further damage.
Your ophthalmologist may recommend:
- Prescribing new or combination eye drops.
- Adjusting your dosage or administration schedule.
- Switching to other forms of treatment, such as laser procedures or surgery in cases where medication is no longer effective.
Why Consistent Eye Exams Matter
Routine checkups are vital, even if your symptoms seem unchanged. Glaucoma is a gradual condition—vision loss can progress for years before it’s noticed, and only through comprehensive eye exams can your doctor catch the earliest signs of change or medication failure.
- Regular testing tracks treatment effectiveness and helps adapt management plans quickly if your vision or eye pressure begins to worsen.
- For optimal results, always report any changes in vision, discomfort, or trouble administering drops between visits.
Frequently Asked Questions (FAQs)
How can I be sure my glaucoma eye drops are working?
Regular visits to your ophthalmologist, who will measure your intraocular pressure and check the health of your optic nerve and retina, are the best way to know for sure. If your pressure remains controlled and your vision tests are stable, your drops are likely working effectively.
Are there warning signs if my glaucoma gets worse despite using eye drops?
Warning signs can include vision changes such as blind spots, worsening peripheral vision, headaches, eye pain, or increased floaters. However, glaucoma often progresses without noticeable symptoms, making routine eye exams crucial for detection.
What should I do if I have trouble using my eye drops correctly?
Ask your eye doctor for tips or consider using assistive devices. Practicing better techniques and using drop guides can significantly improve success. If you have dexterity issues or severe problems, your doctor may recommend alternative treatments.
Is it dangerous to stop eye drops without a doctor’s advice?
Yes. Discontinuing your prescribed medication can rapidly increase your eye pressure and lead to lost vision that cannot be restored. Any changes in medication use must be directed by your ophthalmologist.
What are my options if my current drops are not controlling my condition?
Your doctor may increase the strength, add another type of drop, recommend a different class of medication, or discuss laser or surgical interventions if eye drops alone aren’t sufficient.
Best Practices for Managing Glaucoma With Eye Drops
- Follow your prescription exactly, including timing and number of drops.
- Ask your pharmacist or doctor if unsure about how to use several types of drops together.
- Use reminders, alarms, or tracking apps to stay consistent with your regimen.
- Keep your hands clean before administering drops to prevent eye infections.
- Report any side effects or challenges to your eye care specialist, as adjustments can be made.
Takeaway
Glaucoma management with eye drops is most effective with strict adherence, regular monitoring, and clear communication with your doctor. Recognizing and responding to any changes in your vision or side effects can help you preserve your sight for years to come. Never hesitate to reach out to your eye care team if you suspect your drops are losing effectiveness or if you have challenges maintaining your routine.
References
- https://www.healthline.com/health/eye-health/are-glaucoma-eye-drops-working
- https://pubmed.ncbi.nlm.nih.gov/34999663/
- https://www.healthline.com/health/eye-health/glaucoma-treatments
- https://www.medicalnewstoday.com/articles/glaucoma-eye-drops
- https://www.healthlinejournal.org/ojs/healthline/article/view/H565
- https://glaucoma.org/articles/glaucoma-eye-drops-prevent-vision-loss-but-only-if-patients-use-them
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8814563/
- https://medicine.washu.edu/news/treatment-not-always-needed-to-prevent-vision-loss-in-patients-with-elevated-eye-pressure/
- https://saberhealth.com/news/blog/glaucoma-symptoms-and-treatment
Read full bio of medha deb












