Aplastic Anemia Prognosis in Adults: Outlook, Treatment, and Living Strategies
Understanding how factors like age, severity, and treatment impact the long-term outlook for adults facing aplastic anemia.
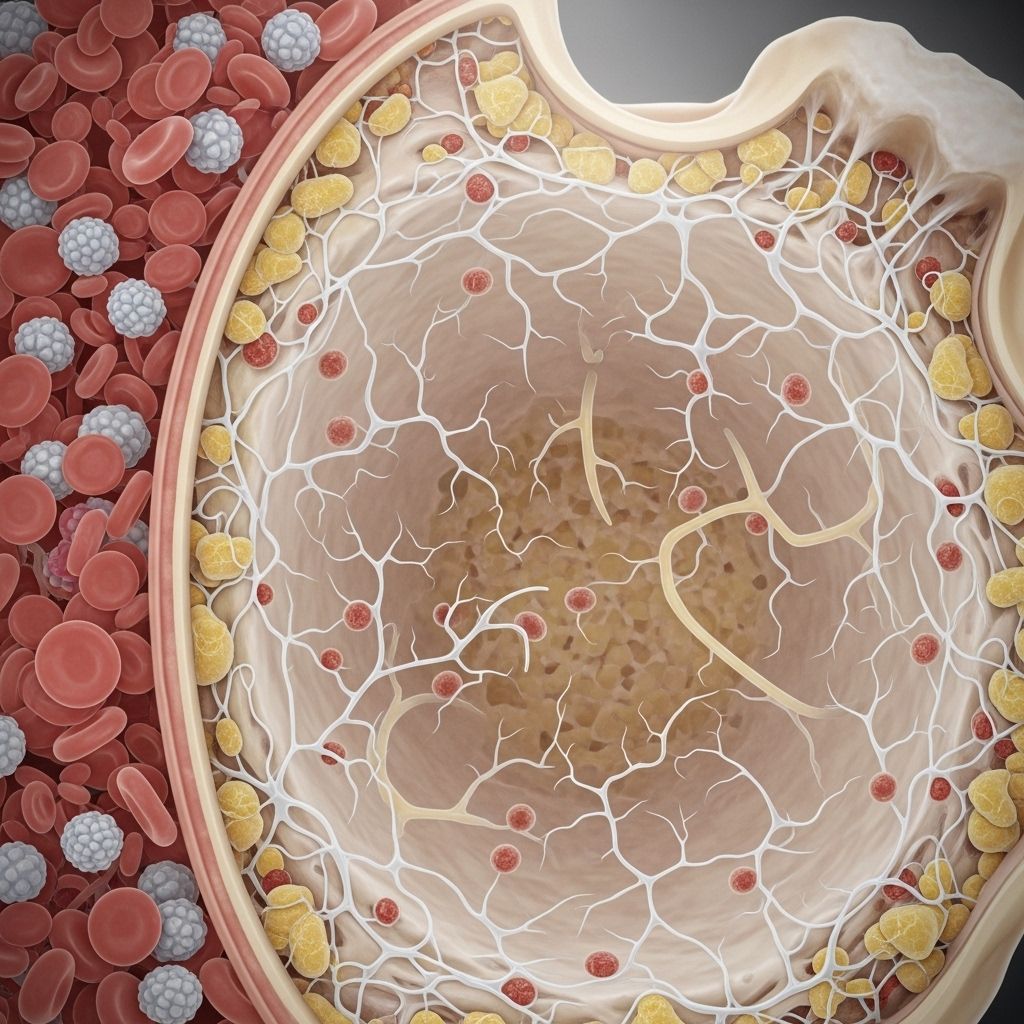
Aplastic anemia (AA) is a complex and potentially life-threatening disorder where the bone marrow fails to produce enough healthy blood cells, leading to deficiencies in red blood cells (RBCs), white blood cells (WBCs), and platelets. This can cause serious medical complications without timely and effective treatment. Prognosis for adults depends on a combination of factors including age, disease severity, overall health, and the response to treatment. Understanding the prognosis of AA is crucial for patients, families, and healthcare professionals in guiding treatment and lifestyle approaches.
What Factors Influence the Prognosis of Aplastic Anemia in Adults?
The outcome for adults diagnosed with aplastic anemia is shaped by multiple key factors, such as:
- Severity of Aplastic Anemia – Classified as moderate, severe, or very severe based on criteria such as blood cell counts and symptoms.
- Age at Diagnosis – Younger adults often have a better outlook compared to older adults.
- Overall Health and Existing Medical Conditions – The presence of additional health problems (comorbidities) can complicate treatment and reduce survival rates.
- Type and Response to Treatment – Advances in therapies, including immunosuppressive drugs and stem cell transplants, have improved outcomes significantly over recent decades.
- Timeliness of Diagnosis and Care – Early intervention is closely linked to better survival.
Historically, AA was almost uniformly fatal, but over the past 30 years, survival rates have increased substantially due to improved care, including immunosuppressive therapy and transplantation techniques.
Research on Prognosis and Survival Rates
Recent studies provide evidence on the prognosis of AA in adults, highlighting how age and treatment influence outcomes:
| Age Group | 5-Year Overall Survival |
|---|---|
| 19–39 years | 90.5% |
| 40–59 years | 70.7% |
| 60+ years | 38.1% |
A 2017 study underlined a clear decline in survival with increasing age. Other research shows that about one-third of older adults (>60 years) with AA achieve a complete treatment response, and roughly 15% reach a partial response after standard immunosuppressive therapies. Factors linked to a poorer prognosis include very severe AA, advanced age, and having multiple other medical conditions. Long-term survival at 30 years is now possible, especially with early diagnosis and current therapies.
Outcomes also depend on the specific treatment path. Patients who undergo a stem cell transplant and those on immunosuppressive therapy have shown similar long-term survival rates, though relapse and specific complications vary depending on the chosen treatment.
How Fast Does Aplastic Anemia Progress?
AA can progress at different rates depending on individual factors. In some, the disease may remain stable for a period, while in others, it can worsen rapidly, especially without treatment. The decline in blood cell production can be gradual or acute. Progression may also result in the development of related blood disorders such as myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML).
Key data points from research suggest:
- Approximately 15% of adults with AA may develop MDS or AML within ten years after diagnosis, particularly those managed with immunosuppressive therapy.
- Some patients experience relapses or resistance to standard treatments.
This highlights the importance of ongoing monitoring and aggressive management to prevent or detect progression promptly.
What Are the Symptoms of Aplastic Anemia in Adults?
AA occurs when bone marrow stem cells are unable to produce adequate amounts of all three blood cell types. Symptoms in adults reflect deficiencies in:
- Red Blood Cells (RBCs): Responsible for oxygen transport — low RBC counts cause anemia, leading to:
- Persistent fatigue
- Weakness
- Dizziness
- Pale skin or pallor
- Shortness of breath
- Headaches
- Rapid or irregular heartbeat
- White Blood Cells (WBCs): Crucial for infection defense — low WBC counts increase infection risk, manifesting as:
- Frequent infections
- Fever
- Difficulty combating common illnesses
- Platelets: Essential for blood clotting — low platelet counts lead to:
- Easy or prolonged bruising
- Frequent or unexplained bleeding (nose, gums)
- Pinpoint red spots on the skin (petechiae)
- Heavy menstrual periods in women
Because these symptoms overlap with other conditions, specialized blood tests and bone marrow examination are typically necessary to confirm the diagnosis in adults.
Aplastic Anemia Treatment Options
Timely treatment is essential since untreated AA often leads to life-threatening complications. The choice of therapy depends on disease severity, patient age, overall health, and the availability of a suitable donor for stem cell transplantation. Treatment options include:
- Immunosuppressive Therapy (IST): Medications that suppress the immune system, such as antithymocyte globulin (ATG) and cyclosporine, are commonly used for adults who are not ideal candidates for transplantation. Recent advances—such as adding eltrombopag, a drug that stimulates platelet production—improve treatment responses and survival rates.
- Stem Cell Transplantation: The only potential cure, involving the replacement of the patient’s bone marrow with healthy donor cells. This is generally recommended for younger adults with a matched sibling donor, though alternative donor techniques are expanding options for older or poorly matched patients.
- Supportive Care: Includes transfusions (blood and platelets), antibiotics for infections, and medications to manage symptoms and reduce risk of complications.
Choosing and timing the appropriate therapy is guided by expert assessment of prognostic factors. Rapid referral and initiation of treatment are crucial for best outcomes.
Common Complications of Aplastic Anemia
Even with improved treatment, AA carries substantial risks for complications, including:
- Severe Bleeding: Due to low platelet counts.
- Infections: As a result of low white blood cell counts.
- Relapse or Treatment Failure: Disease symptoms return after initial response, or the body does not respond to standard therapies.
- Iron Overload: Caused by repeated blood transfusions, can affect organs such as the heart and liver.
- Myelodysplastic Syndromes and Leukemia: Progression to these secondary disorders occurs in a notable percentage of patients over time.
- Graft-Versus-Host Disease (GVHD): Unique to recipients of stem cell transplants—immune cells from the donor attack the patient’s tissues.
- Adverse Drug Reactions or Treatment Side Effects: From immunosuppressive medications or transplants.
Understanding, preventing, and swiftly addressing these complications are key components of comprehensive AA management for adults.
Living with Aplastic Anemia: Daily Strategies for Adults
For those living with AA, ongoing care is important to reduce risks and improve quality of life. Key strategies include:
- Follow All Medical Advice: Attend regular medical checkups and laboratory evaluations to monitor disease status and treatment effects.
- Reduce Exposure to Infection: Maintain strict hygiene, avoid crowds during outbreaks, and promptly report fevers or infection symptoms.
- Prevent Bleeding: Avoid activities with a high risk of injury, use a soft toothbrush, and avoid medications that interfere with clotting unless prescribed.
- Nutrition and Rest: Eat a balanced diet to support recovery and get enough rest. Address fatigue by pacing activities.
- Recognize Signs of Complications: Report unusual bleeding, bruising, infections, or other new symptoms immediately.
- Emotional and Social Support: Consider connecting with support groups or mental health professionals to address the psychological impact of chronic illness.
With appropriate care, many adults can manage symptoms and live fulfilling lives, though continued medical follow-up is necessary.
Frequently Asked Questions (FAQs) About Aplastic Anemia Prognosis in Adults
Q: Is aplastic anemia always fatal?
No. While untreated aplastic anemia often leads to fatal complications, advances in immunosuppressive therapy and bone marrow transplantation have greatly improved survival rates. With prompt and effective treatment, many patients now achieve long-term remission or cure.
Q: How long can adults live with aplastic anemia?
Life expectancy varies based on age, disease severity, and therapy. Survival rates at five years now often exceed 70–90% for younger adults who receive treatment. Most people who receive a successful bone marrow transplant are alive five years after the procedure. Without treatment, survival drops dramatically, with many experiencing serious complications within one year.
Q: What treatments offer the best chance for long-term survival?
Stem cell (bone marrow) transplantation remains the only curative therapy and is preferred for young, otherwise healthy adults with a suitable donor. Immunosuppressive therapy with drugs like ATG, cyclosporine, and eltrombopag is highly effective and offers substantial benefit for many patients, especially when transplants are not an option.
Q: Can aplastic anemia come back after treatment?
Relapse can occur, especially after immunosuppressive therapy. The risk of relapse, as well as of disease progression to conditions such as myelodysplastic syndrome or acute leukemia, underscores the need for ongoing monitoring even after initial remission.
Q: What should I do to lower my risk of complications?
Adhere closely to your treatment plan, attend regular checkups, practice infection prevention, and promptly communicate any new symptoms to your healthcare team. Collaborate with your medical team for individualized advice.
Key Points
- Aplastic anemia prognosis in adults has improved enormously with advances in treatment but depends on age, severity, comorbidities, and treatment response.
- Early intervention increases the chances of remission and long-term survival.
- Both immunosuppressive therapy and stem cell transplantation are effective options, with the best approach determined by patient-specific factors.
- Long-term monitoring is essential to detect relapse or late complications, including progression to other blood disorders.
- With appropriate management, many adults with AA can lead active, fulfilling lives.
References
- https://www.healthline.com/health/iron-deficiency-anemia/aplastic-anemia-prognosis-in-adults
- https://www.ncbi.nlm.nih.gov/books/NBK534212/
- https://www.healthline.com/health/idiopathic-aplastic-anemia
- https://www.aamds.org/aplastic-anemia
- https://my.clevelandclinic.org/health/diseases/16747-aplastic-anemia
- https://www.mayoclinic.org/diseases-conditions/aplastic-anemia/diagnosis-treatment/drc-20355020
- https://ufhealth.org/conditions-and-treatments/aplastic-anemia
Read full bio of Sneha Tete












