Apical Hypertrophic Cardiomyopathy: Symptoms, Causes, Diagnosis, and Care
A comprehensive overview of apical hypertrophic cardiomyopathy, its symptoms, risks, diagnosis, and modern treatment strategies.
Overview of Apical Hypertrophic Cardiomyopathy
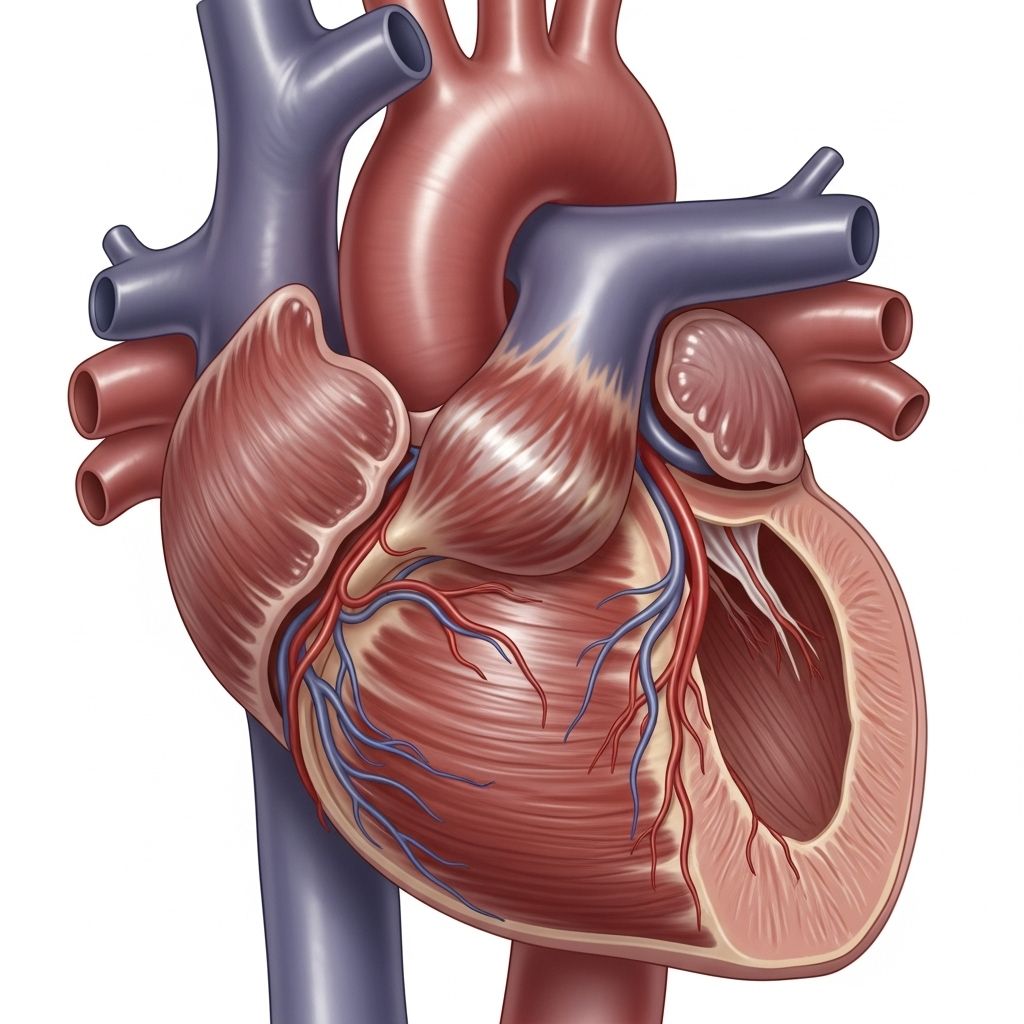
Apical hypertrophic cardiomyopathy (ApHCM) is a rare form of heart muscle disease in which there is abnormal thickening of the heart muscle located near the bottom (apex) of the left ventricle. This unusual variant of hypertrophic cardiomyopathy (HCM) can impact the heart’s ability to pump blood efficiently and may lead to a variety of cardiac symptoms and complications.
The disease shares features with other types of HCM, but it has distinct characteristics, risk factors, and management approaches. Understanding the condition’s mechanisms, potential consequences, and treatment can help affected individuals lead fuller, healthier lives.
Breaking Down the Terminology
- Myopathy: A disorder affecting muscle tissue.
- Cardiomyopathy: Any disease of the heart muscle, potentially impairing function.
- Hypertrophic Cardiomyopathy (HCM): Increase in heart muscle thickness, especially in the left ventricle, making blood pumping less efficient.
- Apical HCM: A subtype mainly involving thickening at the apex of the left ventricle.
Apical Hypertrophic Cardiomyopathy Symptoms
Apical HCM often goes unnoticed in its early stages, as it may not cause any obvious symptoms. When symptoms do appear, they’re frequently nonspecific and may resemble other heart or lung disorders.
- Chest pain (angina)
- Trouble breathing or shortness of breath (especially during exertion)
- Heart palpitations (feeling of skipped or rapid heartbeats)
- Atrial fibrillation (irregular heart rhythm)
- Light-headedness or dizziness
- Exercise intolerance (reduced exercise capacity)
It’s not uncommon for major cardiac events, such as sudden cardiac arrest or stroke, to be an individual’s first warning sign of apical HCM.
Exercise and Apical Hypertrophic Cardiomyopathy
The hallmark of ApHCM—thickening of the heart’s apex—can lead to decreased pumping efficiency. During exercise, the body’s oxygen needs rise, but the heart’s impaired ability to deliver blood can leave tissues starved for oxygen, causing breathlessness and fatigue.
Historically, doctors advised people with HCM to avoid vigorous physical activity out of concern for sudden cardiac death. However, a recent 2023 study found no significant association between vigorous exercise and sudden cardiac death in people with HCM, challenging old guidelines. Nonetheless, exercise plans should always be discussed with a specialist.
What Causes Apical Hypertrophic Cardiomyopathy?
Most cases of HCM, including its apical variant, are inherited, caused by mutations in genes responsible for heart muscle proteins. Over 1,500 different gene mutations are linked to HCM. Yet, fewer people with the apical type report a family history compared to those with classic HCM.
- About 13%–25% of people with ApHCM have identifiable gene mutations.
- The most commonly affected genes are MYBPC3 and MYH7.
Non-Genetic Factors
Some cases aren’t explained by genetics alone. In rare situations, metabolic diseases like Fabry disease can mimic the features of ApHCM.
Risk Factors: Who Gets Apical Hypertrophic Cardiomyopathy?
- Geography: ApHCM is more common in Japan and other East Asian countries than in the United States or Europe.
- Gender: Around two-thirds of people diagnosed are male.
- Age: Most diagnoses occur in the 20s and 30s, but recent research shows increasing cases in the 50s and 60s.
- Family history: Although less frequent than in classic HCM, a positive family history may still increase risk.
Potential Complications of Apical Hypertrophic Cardiomyopathy
While some people with ApHCM live normal lives without symptoms, the condition can lead to serious health problems. Major complications include:
- Atrial fibrillation: Irregular heart rhythm that increases the risk of stroke.
- Chest pain
- Ventricular arrhythmias: Abnormal heart rhythms that may cause sudden cardiac arrest.
- Pulmonary hypertension: High blood pressure in the lung arteries.
- Heart failure or congestive heart failure: The heart can no longer pump efficiently.
- Apical aneurysm: Outpouching of the apex wall, which may promote blood clots and stroke.
In some cases, people may first present with a severe event, such as:
- Sudden cardiac death
- Stroke
- Heart attack
Apical Aneurysms and Thromboembolic Risks
Apical aneurysms—the ballooning out of the thinned apex wall—occur in about 13%–15% of people with ApHCM. These structures can harbor clotted blood, posing a significant risk for stroke. They’re often difficult to see on standard heart ultrasounds and may require advanced imaging.
Diagnosis of Apical Hypertrophic Cardiomyopathy
Proper diagnosis relies on a combination of medical history, physical examination, and cardiac imaging studies.
- Electrocardiogram (ECG): Detects electrical abnormalities suggestive of thickened heart muscle.
- Echocardiography (heart ultrasound): Visualizes the structure and motion of the heart, often revealing apex thickening.
- Cardiac MRI (magnetic resonance imaging): Provides detailed images and can detect apical aneurysms.
- Genetic testing: May find mutations if family history is present or if diagnosis is unclear.
It’s essential to distinguish ApHCM from other causes of left ventricular thickening, such as athletically trained heart, high blood pressure, or disorders like Fabry disease.
Treatment of Apical Hypertrophic Cardiomyopathy
Treatment is individualized and focuses on relieving symptoms, preventing complications, and reducing the risk of sudden cardiac death.
- Medications:
- Beta-blockers: Slow the heart rate and reduce chest pain.
- Calcium channel blockers: Improve heart relaxation and reduce symptoms.
- Antiarrhythmics: Used to control abnormal heart rhythms.
- Anticoagulants: May be necessary if atrial fibrillation or aneurysm increases stroke risk.
- Implantable devices:
- Implantable Cardioverter-Defibrillator (ICD): Considered for those at high risk of life-threatening arrhythmias or sudden cardiac arrest.
- Managing complications: Treatment of heart failure, hypertension, or other coexisting conditions as necessary.
- Lifestyle modifications:
- Tailoring levels of physical activity (ideally under specialist guidance).
- Avoiding dehydration and extreme exercise if directed by a physician.
Surgical options, such as removal of the thickened heart muscle (myectomy), are rarely required for apical HCM but may be considered in severe, unresponsive cases.
Prevention: Can Apical Hypertrophic Cardiomyopathy Be Prevented?
There is currently no known way to prevent inherited forms of ApHCM. Genetic counseling and screening of relatives may help identify high-risk family members early, allowing for monitoring and early intervention.
Secondary prevention involves managing risk factors and complications:
- Regular heart check-ups
- Prompt treatment of high blood pressure or arrhythmias
- Staying informed about one’s genetic and family history
When to Get Medical Help
If you experience unexplained chest pain, shortness of breath, heart palpitations, fainting, or any new cardiovascular symptoms, seek medical attention promptly. Early evaluation can identify ApHCM and reduce the risk of severe complications.
Emergency care is required for any signs of heart attack, loss of consciousness, or sudden weakness and numbness, which may suggest stroke or cardiac arrest.
Outlook for People with Apical Hypertrophic Cardiomyopathy
Many individuals with ApHCM live normal or near-normal lives, especially with appropriate medical care and risk monitoring. Prognosis varies based on symptom severity, presence of complications like atrial fibrillation or aneurysm, and the degree of ventricular thickening.
| Factor | Poor Prognosis Indicator |
|---|---|
| Age at diagnosis | Older age often predicts increased complications |
| Gender | Males may have a higher risk |
| Development of apical aneurysm | Higher risk of stroke and arrhythmia |
| Atrial fibrillation | Higher risk of stroke and heart failure |
| Family history | Increased sudden cardiac death risk |
Frequently Asked Questions (FAQs)
Q: Is apical hypertrophic cardiomyopathy the same as classic HCM?
A: No. While both are forms of hypertrophic cardiomyopathy, the apical variant features thickening at the left ventricle’s apex rather than the more common septal thickening seen in classic HCM.
Q: What is the relationship between apical HCM and sudden cardiac death?
A: Some people with ApHCM are at risk of sudden cardiac death, especially if they have additional risk factors such as a family history or apical aneurysm. Modern research suggests the risk may be less than in classic HCM, but it’s still significant and should be carefully monitored.
Q: Can I exercise if I have apical HCM?
A: Many people with ApHCM can safely exercise, but decisions should be made with a cardiologist. Recent research suggests vigorous activity may not increase sudden death risk, though individual factors matter.
Q: Are genetic tests always positive in apical HCM?
A: No, identifiable gene mutations are found in less than a quarter of cases. Many people with ApHCM do not test positive for known HCM mutations.
Q: What is the most dangerous complication of apical HCM?
A: The most serious risks include sudden cardiac death, stroke (especially with apical aneurysms or atrial fibrillation), and heart failure. Regular monitoring and medical care are crucial.
Summary
Apical hypertrophic cardiomyopathy is an uncommon but potentially serious heart muscle disease. Although it often remains silent for years, it can lead to significant cardiovascular complications, especially if left undiagnosed or untreated. Early detection, genetic counseling, and individualized treatment strategies help reduce risks and optimize quality of life for those affected.
References
- https://www.healthline.com/health/heart-disease/apical-hypertrophic-cardiomyopathy
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6329883/
- https://www.ahajournals.org/doi/10.1161/JAHA.119.015294
- https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/hypertrophic-cardiomyopathy
- https://my.clevelandclinic.org/health/diseases/17116-hypertrophic-cardiomyopathy
- https://www.pennmedicine.org/conditions/hypertrophic-cardiomyopathy
- https://healthcare.utah.edu/healthfeed/2025/05/managing-most-common-inherited-disease-of-heart-muscle-hypertrophic
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3158873/
- https://www.bhf.org.uk/informationsupport/conditions/hypertrophic-cardiomyopathy
Read full bio of Sneha Tete












