Aortic Stenosis Progression: Stages, Symptoms, and Outlook
Understand how aortic stenosis progresses, what factors speed it up, and what symptoms signal each stage to manage your heart health effectively.
Aortic stenosis is a condition where the aortic valve—which regulates blood flow from the heart into the aorta—becomes narrowed or blocked, causing the heart to work harder to push blood through a smaller opening. The speed and impact of aortic stenosis progression vary between individuals but can significantly affect quality of life, heart function, and overall health. Understanding the stages, symptoms, and risk factors is essential for early identification and effective management.
Does Aortic Stenosis Progress Slowly or Rapidly?
The pace at which aortic stenosis advances is highly individual.
- Variability in progression: Some people experience a slow, gradual increase in valve narrowing, while others develop severe disease much more quickly.
- Underlying cause: The major trigger in adults is usually calcification—the hardening of the aortic valve over time. Age is a primary risk factor.
- No simple prediction: There is no confirmed formula to determine why some cases progress rapidly and others do not. However, rapid progression is linked to more serious disease and higher risk of complications, including death.
Key Point: Monitoring by a healthcare provider, often via echocardiogram, is crucial as aortic stenosis advances, since the severity and rate of progression are unpredictable.
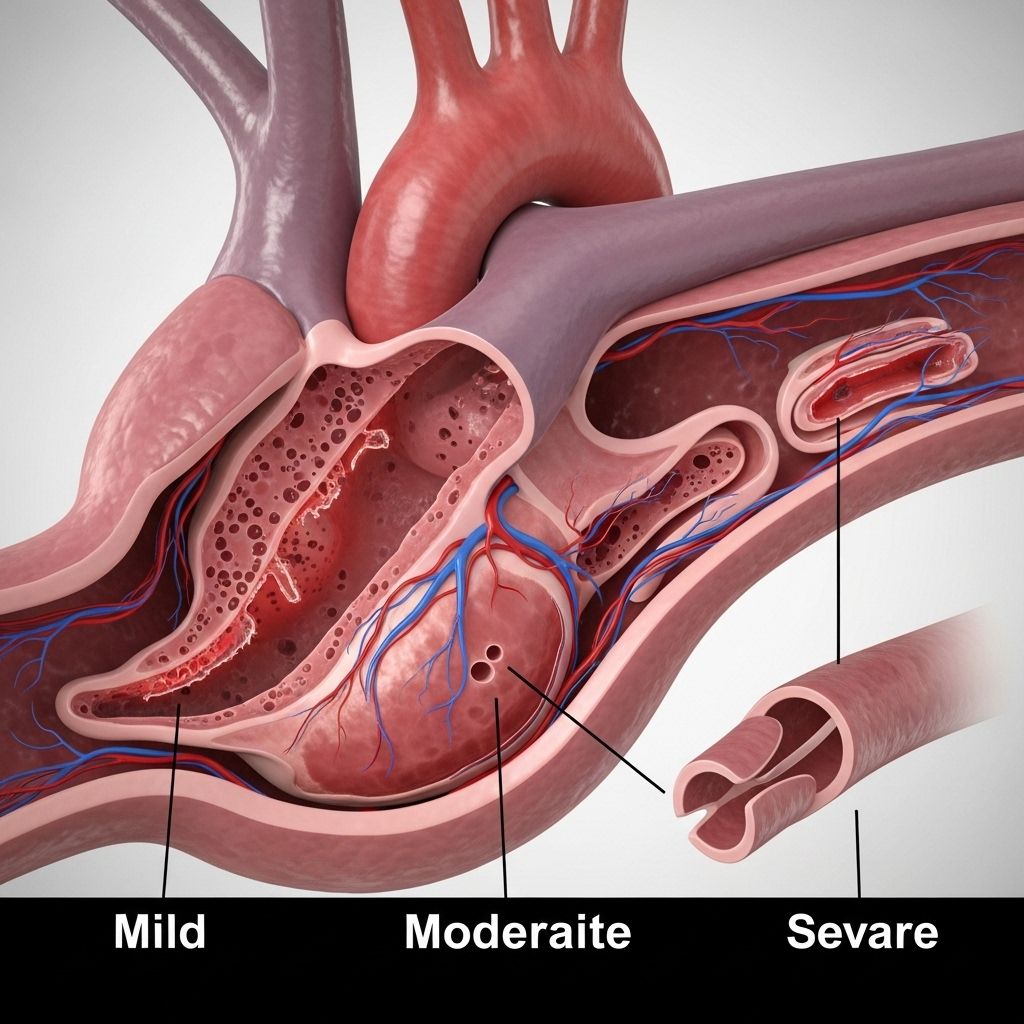
Stages of Aortic Stenosis
Aortic stenosis is staged based on how restricted the aortic valve has become and what additional heart problems, if any, have developed. Different classification systems exist, but most international guidelines describe four to five main stages:
| Stage (US/ACC) | Stage (EU) | Description |
|---|---|---|
| Stage A | Stage 0 | At risk: No valve damage but risk factors present (e.g., age, calcification) |
| Stage B | Stage 1 | Progressive stenosis: Valve narrowing with mild to moderate limitation; left ventricle may begin working harder. |
| Stage C | Stage 2 | Severe stenosis: Severe narrowing, but without symptoms; additional heart structures like the mitral valve may be affected (e.g., leaking/mitral regurgitation, atrial fibrillation). |
| Stage D | Stage 3–4 | Symptomatic severe stenosis: Other valves (tricuspid) and vessels (pulmonary artery) affected; right side of the heart can weaken, potentially leading to right-sided heart failure or pulmonary hypertension. |
Staging helps determine the urgency of treatment and the risk of complications. People with higher-stage disease are typically older and may have additional health conditions.
Common Causes of Aortic Stenosis
- Age-related degeneration: The most common cause is calcium buildup and scarring of the aortic valve, which generally begins after age 60 but typically manifests symptoms after age 70 or 80.
- Bicuspid aortic valve: Some are born with a valve that has two leaflets (cusps) instead of three. This congenital condition is found in 1–2% of people and often leads to earlier-onset stenosis.
- Rheumatic fever: Historic cases of rheumatic fever can cause valve damage and increase aortic stenosis risk, particularly in populations who had childhood illness.
- Congenital defects and other factors: Rarely, some children have abnormal aortic valves that don’t grow properly, predisposing them to stenosis. Other causes in younger individuals are less common.
Factors That Affect How Fast Aortic Stenosis Progresses
While age is the single most significant risk factor, several coexisting health issues can speed up the progression of aortic stenosis and worsen its severity:
- High body mass index (BMI)
- Diabetes mellitus
- Kidney disease
- Previous heart attack or coronary bypass surgery
- Left ventricular hypertrophy (thickened heart muscle)
- Chronic obstructive pulmonary disease (COPD)
- High blood pressure
- High cholesterol
- Male gender and frail health in older age—which frequently coincide with more rapid and severe progression.
Symptoms of Early and Late-Stage Aortic Stenosis
Symptoms usually do not occur until the valve narrowing is significant and the heart is under stress. Aortic stenosis can be “silent” for years, especially in the early phases.
- Common early symptoms:
- Chest pain or pressure (angina)
- Heart palpitations or fluttering
- Shortness of breath, especially during exercise or exertion
- Mild dizziness or lightheadedness, possibly fainting during activity
- Late-stage or worsening symptoms:
- Significant shortness of breath
- Low tolerance for daily activities or reduced exercise capacity
- Swelling in the feet or ankles
- Difficulty sleeping or needing extra pillows to breathe comfortably
- Pronounced fatigue, even with minimal activity
- Irregular heart rhythms (atrial fibrillation)
- Signs of heart failure or pulmonary hypertension—may include problems with the right side of the heart as the disease progresses
- Chronic cases: Without treatment, advanced aortic stenosis can lead to heart failure, which brings extreme tiredness, significant shortness of breath, and more pronounced swelling in extremities.
How is Aortic Stenosis Progression Monitored?
Doctors track aortic stenosis progression using several medical tests and patient-reported symptoms:
- Echocardiogram: Ultrasound examination of the heart is the standard way to assess valve narrowing, blood flow, and heart muscle function.
- Electrocardiogram (ECG): Assesses heart rhythm disturbances and signals of strain on the heart.
- Physical examination: Doctors listen for heart murmurs, irregular rhythms, and look for swelling or signs of breathing difficulty.
- Symptom tracking: Patient input on energy level, breathing, chest pain, and other changes helps guide staging and treatment decisions.
What Increases the Risk of Rapid Aortic Stenosis Progression?
| Risk Factor | Potential Impact |
|---|---|
| Age over 65 | Most common; often coexists with calcification and valve stiffening. |
| Bicuspid aortic valve | Earlier onset; may progress more rapidly than typical calcific stenosis. |
| Chronic kidney disease | Faster calcification and more severe heart valve disease. |
| History of heart attack or heart surgeries | May accelerate deterioration of valve and pump function. |
| Diabetes and high cholesterol | Contribute to vascular disease and can speed up valve damage. |
| Male sex and frail general health | Linked with increased risk and faster disease progression. |
Frequently Asked Questions (FAQs)
Q: What are the earliest warning signs of aortic stenosis?
A: Early warning signs are often subtle and may include mild chest discomfort, slight shortness of breath with activity, or feeling more fatigued than usual. Many people notice symptoms only during physical exertion.
Q: How is aortic stenosis diagnosed?
A: Diagnosis is typically confirmed by an echocardiogram, a painless ultrasound that reveals valve structure and function. Your doctor may also use a stethoscope to detect a heart murmur before ordering imaging tests.
Q: Can lifestyle changes slow aortic stenosis progression?
A: While lifestyle changes can help manage cholesterol, blood pressure, and diabetes—factors that contribute to more rapid progression—they usually do not reverse valve narrowing itself. Monitoring your cardiac risk factors remains crucial.
Q: When is surgery or valve replacement recommended?
A: Valve replacement is considered when stenosis becomes severe and you have symptoms or when there is evidence of significant damage to your heart, even without obvious symptoms. The timing is based on disease progression, heart function, and your overall health.
Q: Is aortic stenosis preventable?
A: Age-related forms are not typically preventable, but managing risk factors (e.g., high blood pressure, cholesterol) and regular monitoring can help delay progression and reduce complications.
When Should I See a Doctor for Aortic Stenosis Symptoms?
Contact a healthcare provider if you notice new or worsening symptoms such as:
- Increasing chest pain or discomfort
- Shortness of breath, especially with activity or when lying down
- Swelling in your feet or ankles
- Unusual fatigue or inability to complete regular activities
- Dizziness, lightheadedness, or fainting episodes
- New irregular heartbeats or palpitations
If you have already been diagnosed with aortic stenosis and develop these symptoms, prompt evaluation is necessary as they may indicate progression to a more severe stage or the onset of heart failure complications.
Key Takeaways
- Aortic stenosis is a progressive condition usually caused by calcification and valve stiffening in older adults, but younger people may be affected by congenital or post-infection causes.
- Progression speed varies but tends to accelerate in the presence of other cardiac or metabolic diseases.
- Symptoms worsen as stenosis becomes more severe, so regular medical follow-up and symptom tracking are essential.
- Treatment options depend on the stage of disease, overall heart function, and presence of symptoms, with valve replacement often considered in severe cases to prevent heart failure and improve quality of life.
References
- https://www.healthline.com/health/heart/aortic-stenosis-progression
- https://www.upmc.com/services/heart-vascular/conditions/aortic-stenosis
- https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-aortic-valve-stenosis
- https://www.mayoclinic.org/diseases-conditions/aortic-stenosis/symptoms-causes/syc-20353139
- https://www.massgeneralbrigham.org/en/patient-care/services-and-specialties/heart/conditions/aortic-valve-stenosis
- https://www.pennmedicine.org/conditions/aortic-valve-stenosis
- https://www.ncbi.nlm.nih.gov/books/NBK557628/
- https://health.clevelandclinic.org/aortic-stenosis-progression
Read full bio of medha deb












