Aortic Stenosis Progression: Stages, Symptoms, and Risk Factors
Understand how aortic stenosis develops, its stages, factors influencing progression, and the signs to watch for as the disease advances.
Aortic Stenosis Progression: An In-Depth Guide
Aortic stenosis is a significant heart valve condition involving narrowing of the aortic valve opening, limiting blood flow from the heart to the rest of the body. The disease can progress at various rates and is influenced by age, genetics, and additional health factors. Understanding the progression, risk factors, and symptoms is essential for early recognition and effective treatment.
Table of Contents
- What is Aortic Stenosis?
- How Fast Does Aortic Stenosis Progress?
- Stages of Aortic Stenosis
- Factors Affecting Progression Speed
- Symptoms of Early and Late-Stage Aortic Stenosis
- Diagnosis and Monitoring
- Frequently Asked Questions (FAQs)
What is Aortic Stenosis?
Aortic stenosis (AS) refers to the narrowing of the heart’s aortic valve, limiting blood flow from the left ventricle into the aorta and subsequently to the body. The valve may stiffen and fail to open completely, causing the heart to work harder, leading to cardiac muscle thickening and potential heart failure if left untreated.
Main Causes of Aortic Stenosis
- Age-related calcification: Most common in older adults due to calcium buildup on the valve.
- Bicuspid aortic valve: Congenital condition where the valve forms with two cusps instead of three, leading to early dysfunction.
- Rheumatic fever: Previous infection can cause scarring and narrowing of the valve.
How Fast Does Aortic Stenosis Progress?
The speed at which aortic stenosis progresses varies widely. Some people experience slow, gradual narrowing over years, while others may see rapid progression. The underlying cause—whether degeneration over time or congenital factors—along with individual health, plays a critical role in how quickly symptoms and complications develop.
- Rapid progression is associated with more severe disease and a higher risk of complications or mortality.
- There’s currently no universal formula to predict an individual’s rate of aortic stenosis progression.
- Progression may accelerate in the presence of comorbid health problems or high-risk factors.
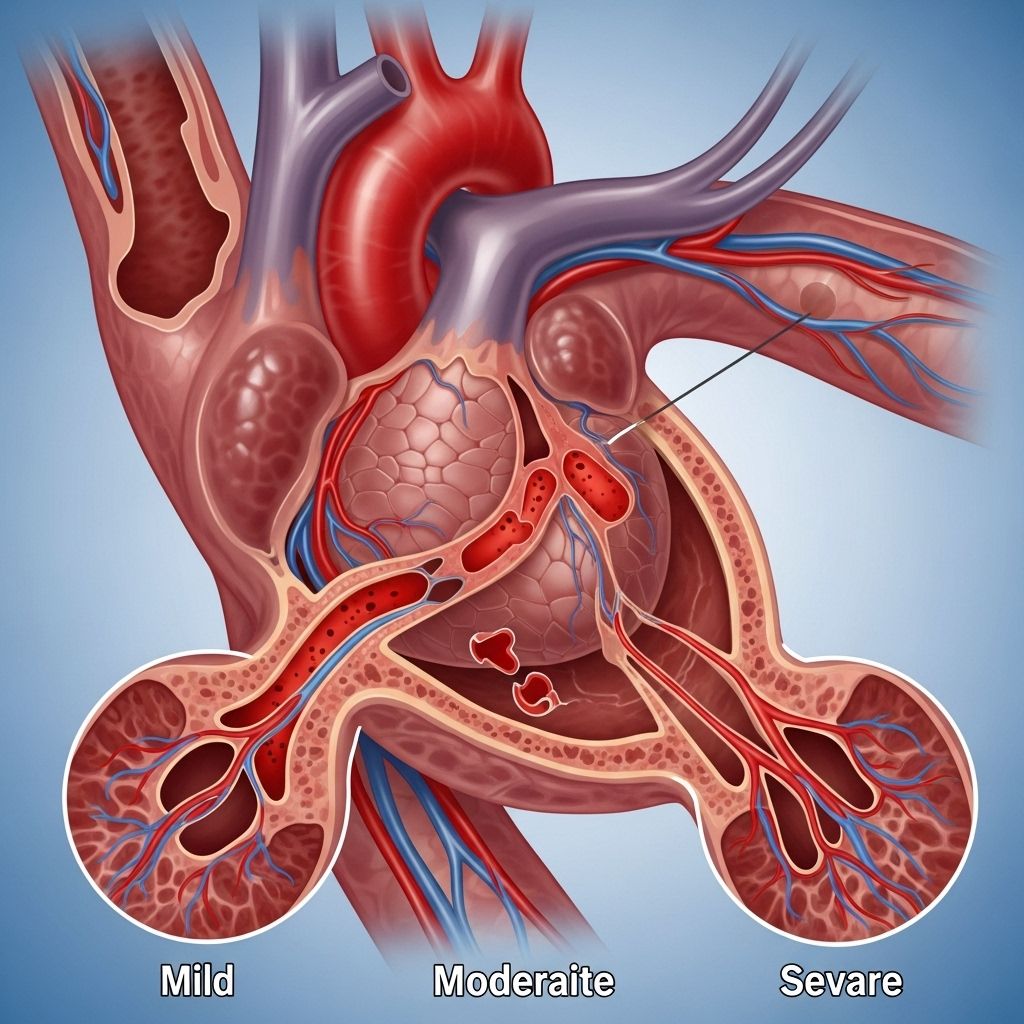
Stages of Aortic Stenosis
Aortic stenosis is categorized by stage according to the severity, associated cardiac damage, and symptoms. Multiple clinical guidelines exist for staging, with two prominent systems: the European Heart Journal model (Stages 0–4) and the American College of Cardiology/American Heart Association model (Stages A–D).
| European Staging (0–4) | American Staging (A–D) | Description |
|---|---|---|
| Stage 0 | Stage A | Risk factors or diagnosis without valve damage or symptoms. |
| Stage 1 | Stage B | Valve and left ventricle affected; obstructed flow, no symptoms. |
| Stage 2 | Stage B/C | Damage extends to the left atrium and mitral valve, often leading to mitral regurgitation and possible atrial fibrillation. |
| Stage 3 | Stage C | Additional valves (e.g., tricuspid) and vessels involved, may lead to pulmonary hypertension. |
| Stage 4 | Stage D | Severe valve obstruction with symptoms; right ventricle damage may be present. |
Summary of Stages
- Stage 0: Aortic stenosis present but heart tissue and function remain unaffected.
- Stage 1: Impacts left ventricle (main pumping chamber); start of reduced efficiency.
- Stage 2: Damage spreads to left atrium and mitral valve; risk of irregular heart rhythms.
- Stage 3: Additional cardiac valves and pulmonary artery involved; may develop pulmonary hypertension (high blood pressure in lungs).
- Stage 4: Right ventricle weakened or damaged; severe functional impairment, often linked with heart failure.
How Staging Is Determined
Staging typically relies on echocardiogram imaging to assess blood flow restriction and structural heart changes. Patients with higher stage disease tend to be older and possess more contributing health problems.
Factors Affecting Progression Speed
Several factors can influence how fast aortic stenosis advances from a mild condition to a critical stage. Understanding these can help with risk assessment and intervention planning.
- Age: Older individuals often experience more rapid progression.
- Existing Cardiac Disease: Prior heart attacks or bypass surgeries can accelerate valve deterioration.
- Body Mass: Higher body mass index is linked to faster worsening of symptoms and cardiac function.
- Diabetes: Raises the risk for rapid progression and complications.
- Chronic Kidney Disease: Renal impairment is a notable risk factor.
- Chronic Obstructive Pulmonary Disease (COPD): Respiratory disease complicates heart function, exacerbating stenosis effects.
- High Blood Pressure & High Cholesterol: Both contribute to further valve and cardiac damage.
- Thickening of the Left Ventricle: Reflects increased workload and advancing disease.
Symptoms of Early and Late-Stage Aortic Stenosis
Most patients with aortic stenosis experience no symptoms until the narrowing is advanced, restricting blood flow and prompting cardiac or systemic issues. As stenosis worsens, signs and symptoms intensify and may hint at the heart’s declining ability to compensate.
Early Signs and Symptoms
- Chest pain or pressure
- Heart palpitations or fluttering
- Shortness of breath (especially with activity)
- Unusual fatigue or low energy for routine tasks
- Dizziness or fainting (syncope)
- Heart murmur (often detected by a physician before symptoms develop)
Late and Severe Symptoms
- Worsening chest pain or tightness
- Severe shortness of breath, even at rest
- Swollen feet or ankles
- Difficulty sleeping flat or needing multiple pillows to breathe comfortably
- Increased fatigue with even minimal exertion
- Development of heart failure signs: weight gain, persistent cough, severe tiredness
- Pulmonary hypertension symptoms: fatigue, chest discomfort, swelling, and shortness of breath
As the disease progresses, symptoms such as fainting or abrupt shortness of breath can become medical emergencies and warrant immediate attention.
Diagnosis and Monitoring
Echocardiography is the primary tool for diagnosing and monitoring aortic stenosis progression. Regular assessments help determine current stage, evaluate cardiac damage, and guide the timing of interventions such as valve replacement.
When to Seek Medical Attention
- New or worsening symptoms
- Exercise intolerance (getting tired or breathless during routine activities)
- Swelling in lower limbs or abdomen
- Episodes of fainting or severe chest pain
Those with diagnoses or risk factors should maintain regular follow-up with a cardiologist, who may recommend lifestyle changes, medications, or procedures to slow progression or alleviate symptoms.
Frequently Asked Questions (FAQs)
Does aortic stenosis always require surgery?
Not all cases immediately require surgery. Early-stage or slowly-progressing aortic stenosis can often be managed with careful monitoring and medication. Advanced or severe symptomatic stenosis, however, often necessitates valve replacement for improved outcomes.
Can aortic stenosis be prevented?
While certain causes such as congenital valve defects can’t be prevented, general heart-healthy measures—controlling blood pressure, cholesterol, diabetes, and maintaining a healthy weight—may help slow disease progression. Preventing rheumatic fever in childhood also reduces later risk.
How often should someone with aortic stenosis see their doctor?
Frequency of follow-up depends on disease stage and symptom status. Some may need annual checkups, while others with rapid progression or severe disease require more frequent visits and imaging.
What lifestyle changes are recommended for people with aortic stenosis?
- Adopt a heart-healthy diet low in sodium and saturated fats.
- Engage in regular, moderate exercise as approved by a physician.
- Avoid smoking and excessive alcohol.
- Maintain strict control of chronic conditions like high blood pressure and diabetes.
Are there any treatments to reverse aortic stenosis?
The narrowing itself generally cannot be reversed with medication; surgical procedures such as valve repair or replacement are needed in severe cases. Medical therapy can manage symptoms and underlying contributing conditions.
Key Takeaways
- Aortic stenosis progression is highly individual, with rates influenced by age, heart health, and coexisting conditions.
- Regular monitoring is essential—even in the absence of symptoms—for timely intervention and better outcomes.
- Early symptom recognition can help prevent complications like heart failure and improve quality of life.
- Healthy lifestyle choices may slow disease progression and reduce cardiovascular risk.
Consult a cardiologist for personalized advice if you or a loved one are at risk for or diagnosed with aortic stenosis.
References
- https://www.healthline.com/health/heart/aortic-stenosis-progression
- https://www.upmc.com/services/heart-vascular/conditions/aortic-stenosis
- https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-aortic-valve-stenosis
- https://www.mayoclinic.org/diseases-conditions/aortic-stenosis/symptoms-causes/syc-20353139
- https://www.massgeneralbrigham.org/en/patient-care/services-and-specialties/heart/conditions/aortic-valve-stenosis
- https://www.pennmedicine.org/conditions/aortic-valve-stenosis
- https://www.ncbi.nlm.nih.gov/books/NBK557628/
- https://health.clevelandclinic.org/aortic-stenosis-progression
Read full bio of medha deb












