Aortic Dissection: Causes, Symptoms, Diagnosis, and Treatment
A detailed guide to aortic dissection: identifying the condition, understanding its risks, and exploring treatment approaches.
Aortic Dissection: An Overview
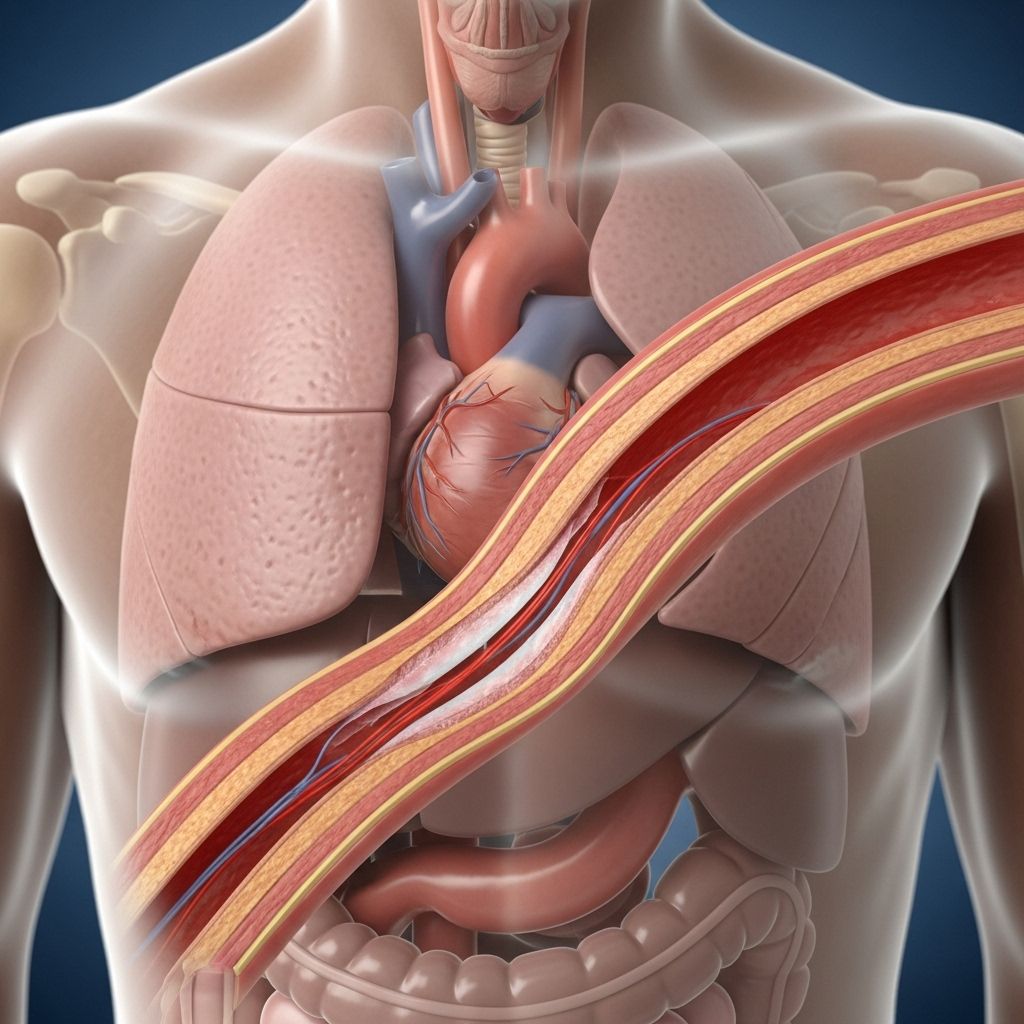
Aortic dissection is a critical medical emergency where the inner layer of the aorta—the major blood vessel carrying blood from the heart to the rest of the body—tears. Blood flows through the tear, separating the inner and middle layers of the artery, a process called a “dissection.” Without prompt treatment, this condition can be fatal as the tear may allow blood to escape the vessel entirely, leading to catastrophic internal bleeding.
This condition is rare but most frequently occurs in men between 60 and 70 years old. The symptoms often mimic those of other serious heart conditions, such as heart attacks, which may result in delayed diagnosis. However, early identification and rapid medical intervention are crucial for survival.
What is Aortic Dissection?
An aortic dissection is defined by a tear in the innermost layer of the aortic wall (the intima). Blood enters through this tear, pushing between the intima and the middle layer (the media), creating a false channel. This false channel may extend along the length of the aorta and interrupt blood flow to critical organs.
Dissections can occur anywhere along the aorta but are most common in the segment that traverses the chest (thoracic aorta).
- Potential complications: Reduced blood flow to vital organs, life-threatening rupture, and stroke-like symptoms.
- Risk: Severe and sudden onset requiring emergency medical care.
Symptoms of Aortic Dissection
The classic symptom is intense and sudden pain, often described as tearing or ripping, which radiates through the chest, back, or neck. Due to the overlap with other cardiac conditions, diagnosis is often challenging.
- Sudden, severe chest or back pain (may shift towards the neck or abdomen).
- Abdominal pain.
- Shortness of breath.
- Loss of consciousness.
- Low pulse.
- Stroke-like symptoms: confusion, slurred speech, vision problems, weakness or paralysis in one side of the body, difficulty walking.
- Pain in one leg.
Types of Aortic Dissection
Aortic dissections are classified primarily according to the location of the tear:
| Type | Description | Risks |
|---|---|---|
| Type A | Tear in the ascending (upper) aorta, may extend to the abdomen. | Most common and dangerous; highest risk for fatal complications. |
| Type B | Tear in the descending (lower) aorta. | Can progress to abdominal involvement; generally lower immediate risk than Type A. |
Medical professionals further classify dissections by timing:
- Acute: Present for less than 2 weeks.
- Chronic: Present for more than 2 weeks.
Causes and Risk Factors
Aortic dissection is typically the result of weakening of the aortic wall. Several factors can contribute:
- Chronic high blood pressure (hypertension): Weakens the integrity of the aortic tissue over years.
- Connective tissue disorders: Such as Marfan Syndrome, Ehlers-Danlos Syndrome.
- Congenital heart defects: Especially bicuspid aortic valve.
- Pre-existing aortic aneurysm: A bulge or weakening in the aortic wall increases the risk of a tear.
- Chest trauma: Injury from accidents or invasive procedures.
- Older age: Most cases occur in those 60 and above.
- Gender: Higher incidence in males.
- Family history of aortic disease.
- Illegal drug use: Cocaine and stimulants can cause surges in blood pressure.
Diagnosis of Aortic Dissection
Diagnosis requires a high index of suspicion and advanced imaging techniques, as symptoms can mimic heart attacks or strokes. Rapid identification improves outcomes.
- Medical History and Examination: Detailed questioning regarding symptom onset, pain quality, and risk factors.
- Imaging Studies:
- Computed Tomography Angiography (CTA): Gold standard for diagnosis; shows the location, type, and extent of dissection.
- Echocardiography: Especially valuable for ascending aorta involvement in initial screening.
- Magnetic Resonance Angiography (MRA): Alternative if CTA is unavailable.
- Digital Subtraction Angiography (DSA): May help in difficult cases.
- Transesophageal Echocardiography (TEE): Enables visualization from within the esophagus.
- Other Tests: Blood pressure measurement in both arms, ECG to rule out heart attack, laboratory tests.
Treatment Options for Aortic Dissection
Treatment depends on the type and severity of the dissection, as well as the overall health of the patient. Management typically includes a combination of emergency intervention, medication, and surgery:
- Medication: Immediate blood pressure reduction and heart rate control to prevent further stress on the aorta. Pain management is crucial.
- Emergency Surgery: Indicated in acute Type A dissections and some complex Type B cases. Surgical options include:
- Aortic replacement
- Endovascular repair (stent grafting)
- Covered stent implantation
- Conservative Management: Used for stable, uncomplicated Type B dissections. Involves close monitoring and medications.
- Long-term Management:
- Regular imaging of the aorta
- Continued blood pressure and heart rate management
- Lifestyle modifications (diet, exercise)
- Psychological and social support
Aortic Dissection in Children
Though aortic dissection is rare in children, it can occur and presents unique challenges:
- Rarity: Most cases occur due to underlying connective tissue disorders, congenital heart disease, or trauma.
- Diagnosis: Often delayed due to vague symptoms and lack of awareness among pediatricians.
- Imaging: CTA remains the diagnostic standard; echocardiography can aid in screening lesions involving the ascending aorta.
- Treatment: Follows adult protocols, with surgical intervention preferred for most cases. Children tend to have better outcomes than adults.
- Follow-up: Lifelong monitoring, imaging, and supportive care are critical to prevent recurrence or complications.
Can an Aneurysm Increase Your Risk of Aortic Dissection?
A pre-existing aortic aneurysm is a significant risk factor for dissection. The weakened and stretched wall of the aneurysm makes the aorta more susceptible to tears that can progress into a full-thickness dissection. Sometimes, a dissection is the first warning sign of an otherwise silent aneurysm.
Complications of Aortic Dissection
Complications arise both from impaired blood supply and potential rupture:
- Organ damage: If blood flow to organs such as the kidneys, intestines, or spinal cord is compromised.
- Stroke: Disruption of blood flow to the brain.
- Rupture: Fatal internal bleeding if the dissection breaks through the outer wall.
- Heart problems: Possible valve or coronary artery involvement.
Living With and Preventing Aortic Dissection
While some risk factors like age and genetic predisposition are unavoidable, certain strategies may decrease the likelihood of developing aortic dissection, particularly for those at risk:
- Regular blood pressure checks and control with lifestyle and medication.
- Treatment of underlying connective tissue disorders.
- Routine medical imaging for those with a family history or previous aneurysm.
- Healthy lifestyle:
- Heart-healthy diet
- Regular exercise
- Avoiding tobacco and stimulant drugs
- Prompt attention to chest, back, or abdominal pain, especially in high-risk individuals.
Frequently Asked Questions (FAQs)
What is the difference between an aortic dissection and an aortic aneurysm?
An aortic aneurysm is a bulge in the aorta caused by weakening of the vessel wall; an aortic dissection is a tear in the inner wall resulting in blood separating the aorta’s layers. Having an aneurysm increases the risk of a dissection.
Who is most at risk for aortic dissection?
Men over age 60, people with chronic high blood pressure, those with connective tissue disorders or congenital heart defects, and individuals with a family history of aortic disease are most at risk.
How is aortic dissection diagnosed?
It is diagnosed with advanced imaging, especially computed tomography angiography (CTA), alongside symptom assessment and clinical exams.
Can aortic dissection be prevented?
Some risk can be reduced by controlling blood pressure, treating underlying conditions, and avoiding stimulant drugs. Those with genetic risks need close monitoring.
Is aortic dissection always fatal?
No, but it has a high mortality without prompt diagnosis and treatment. Survival is greatly improved with early medical and surgical intervention.
Can children get aortic dissections?
Yes, though rare, children—especially those with certain genetic or heart conditions—can experience aortic dissection. Outcomes are better with timely treatment and lifelong follow-up.
Summary Table: Aortic Dissection Facts
| Key Point | Details |
|---|---|
| Incidence | Rare; most frequent in older males (60–70+ years) |
| Main artery involved | Aorta (body’s largest blood vessel) |
| Main symptom | Sudden, severe, tearing chest or back pain |
| Diagnosis | CTA, echocardiography, MRA, DSA |
| Treatment | Emergency surgery and medication |
| Prognosis | Better with rapid medical attention and follow-up |
References
- https://www.healthline.com/health/aortic-dissection-vs-aneurysm
- https://www.mayoclinic.org/diseases-conditions/aortic-dissection/symptoms-causes/syc-20369496
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11921325/
- https://www.medicalnewstoday.com/articles/323435
- https://medlineplus.gov/ency/imagepages/18073.htm
Read full bio of medha deb












