Understanding the Connection Between Anxiety and Hypoglycemia in Diabetes
Explore how blood sugar fluctuations affect anxiety and what people with diabetes can do to manage both.
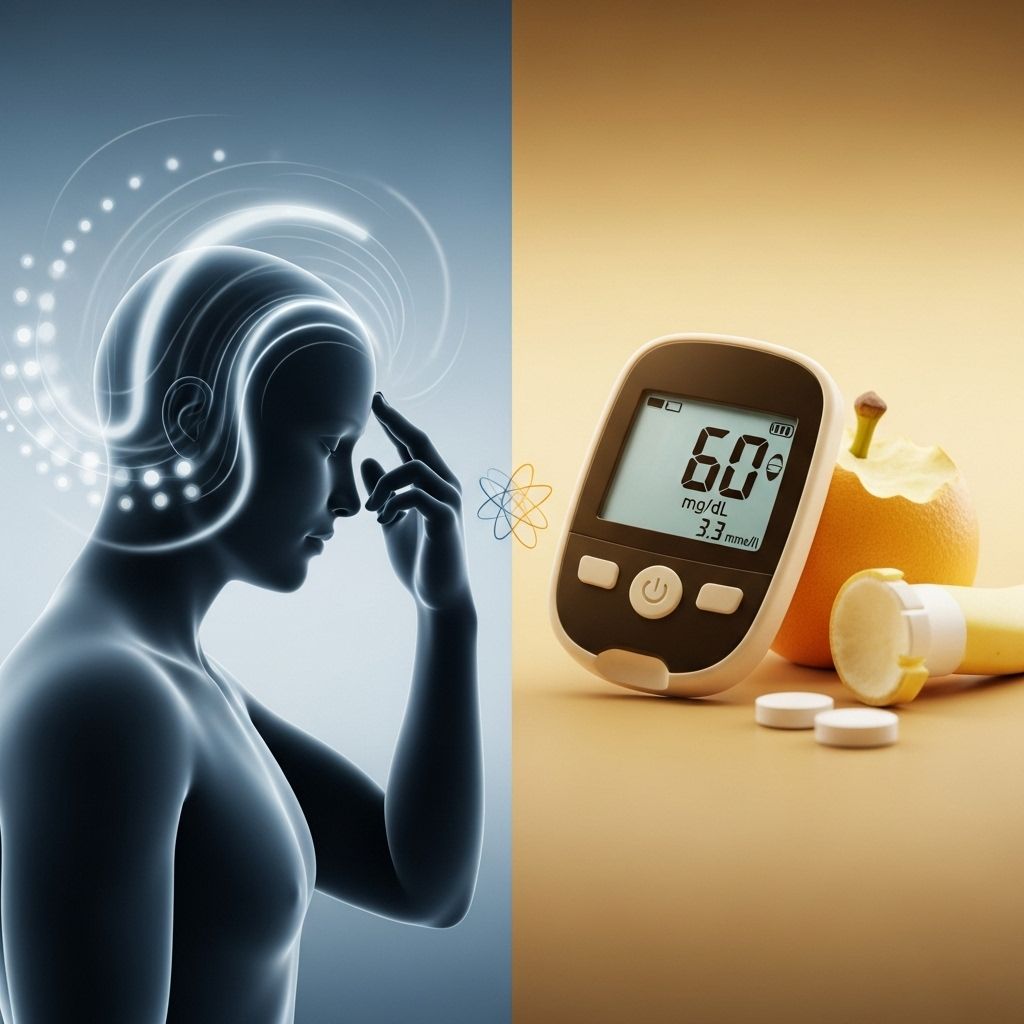
Managing diabetes is a complex balancing act, and it extends beyond monitoring blood sugar levels. Many individuals living with diabetes also struggle with mental health concerns, especially anxiety. One of the most challenging overlaps is between the symptoms of anxiety and hypoglycemia (low blood sugar). This article explores the interplay between the two, how to recognize and differentiate their symptoms, and provides strategies to manage both effectively.
How Are Anxiety and Hypoglycemia Connected?
There’s a strong bidirectional relationship between diabetes and mental health, particularly when it comes to anxiety and hypoglycemia episodes. Simply put, experiencing one can increase the risk or intensity of the other.
- Hypoglycemia can trigger symptoms that mimic, worsen, or even directly cause anxiety.
- Anxiety can lead to behaviors that increase risk for hypoglycemic episodes (such as disrupted eating, increased vigilance, or overcorrecting with insulin).
- The fear of having low blood sugar—sometimes called “hypoglycemia anxiety”—is a significant psychological concern for many people with diabetes.
Blood sugar fluctuations don’t just affect the body physically; they can also create psychological distress. When blood sugar drops too low (below 70 mg/dL for most people with diabetes), the body releases stress hormones—including adrenaline and cortisol—that trigger classic symptoms of anxiety.
Why Does Low Blood Sugar Cause Anxiety?
When blood glucose declines, the body’s stress response kicks in. Here’s the mechanism:
- Adrenaline (epinephrine) is released to stimulate glucose production from the liver, making the heart race and causing shakiness and sweating—symptoms that overlap with anxiety.
- Cortisol, the stress hormone, is also produced and can impact mood, making you feel tense and anxious.
- Physical sensations of hypoglycemia (weakness, dizziness, palpitations) are very similar to those of a panic attack or heightened anxiety state.
The combination of physiological and psychological responses can make it difficult to tell whether you’re experiencing hypoglycemia, anxiety, or both. In fact, studies show that insulin-treated type 1 and type 2 diabetes patients with impaired hypoglycemia awareness report higher levels of general anxiety and depression.
Recognizing Symptoms: Hypoglycemia vs. Anxiety
Because the symptoms of hypoglycemia and anxiety overlap, differentiating them can be tricky. Below is a comparative table of common symptoms:
| Symptom | Hypoglycemia | Anxiety |
|---|---|---|
| Shakiness | ✔️ | ✔️ |
| Palpitations / Rapid Heartbeat | ✔️ | ✔️ |
| Sweating | ✔️ | ✔️ |
| Irritability | ✔️ | ✔️ |
| Lightheadedness | ✔️ | ✔️ |
| Tremors | ✔️ | Sometimes |
| Hunger | ✔️ | Rarely |
| Confusion / Difficulty Concentrating | ✔️ | ✔️ |
| Feelings of Doom / Panic | Sometimes | ✔️ |
| Visual Disturbances | ✔️ | No |
Some symptoms, such as hunger and visual disturbances, point more toward hypoglycemia, while excessive fear or worry and panic are classic anxiety features. Importantly, checking your blood glucose level—using a glucometer or continuous glucose monitor—is the only way to definitively distinguish between the two in the moment.
What Causes Hypoglycemia in Diabetes?
Hypoglycemia occurs in people with diabetes when blood sugar falls too low, usually due to:
- Taking too much insulin or diabetes medication
- Skipping or delaying meals
- Eating less than usual
- More intense or prolonged physical activity
- Alcohol consumption without adequate food
Even people without diabetes can experience hypoglycemia in rare cases, often due to medications, excessive alcohol, underlying illness, or, rarely, after gastric (bariatric) surgery.
Why Is Anxiety Common in Diabetes?
Anxiety is particularly prevalent in people living with diabetes, and hypoglycemia is a key factor:
- Fear of Low Blood Sugar: Prior episodes of severe hypoglycemia can lead to a persistent fear of recurrence, called “fear of hypoglycemia (FoH).”
- Anxious Vigilance: Constant monitoring of blood sugar and anticipating lows can itself be anxiety-provoking.
- Lifestyle Disruption: The daily demands of diabetes management (medication, diet, exercise) can worsen background anxiety and make symptoms harder to tease apart.
In many cases, anxiety and depression are found to be more common in individuals with impaired awareness of hypoglycemia (IAH)—where early warning signs of hypoglycemia are dulled, making the risk of sudden, severe lows and associated anxiety greater.
Can Both Happen at the Same Time?
Yes, low blood sugar and anxiety can co-occur, either compounding each other’s effects or making diagnosis more elusive. Sometimes, one can act as a trigger for the other:
- A hypoglycemic episode may provoke anxiety about immediate safety or long-term management.
- Several physical symptoms of low blood sugar can feed into panic or anxiety loops, particularly in those with generalized anxiety disorder.
- Persistent anxiety can contribute to unhealthy habits such as disordered eating, skipping meals, or overuse of insulin as a form of self-management, all of which raise hypoglycemia risk.
Clinical observation and case reports suggest diet modification, such as increasing dietary protein, fat, and fiber, may reduce symptoms of both anxiety and hypoglycemia, especially in those who consume high amounts of refined carbohydrates.
How to Tell the Difference Between Low Blood Sugar and Anxiety
When you’re not sure whether your symptoms are due to low blood sugar or anxiety, try the following steps:
- Check your blood sugar. Use your glucose meter or CGM. Hypoglycemia is typically defined as <70 mg/dL, although in healthy non-diabetics, the threshold may be slightly lower.
- Consider timing and context. Hypoglycemia often occurs after a long gap between meals, strenuous exercise, use of insulin, or missed meals. Anxiety may occur anytime, often after stress or psychological triggers, though not always predictable.
- Monitor symptom progression. Symptoms of low blood sugar usually improve rapidly (within 10–15 minutes) after consuming carbohydrate sources. Anxiety symptoms often persist even after eating or raising blood sugar.
Always err on the side of caution: if you suspect hypoglycemia, treat it immediately following your healthcare provider’s guidelines.
Strategies to Manage Anxiety and Prevent Hypoglycemia
Effective management involves both medical and psychological strategies. Consider the following:
Blood Sugar Management
- Maintain regular meal times with balanced macronutrients (carbohydrates, proteins, fats, and fiber).
- Avoid high glycemic index foods that lead to rapid blood sugar spikes and subsequent crashes.
- Monitor blood glucose frequently, especially when starting new medication, altering physical activity, or during illness.
- Keep quick-acting glucose sources (like glucose tablets or gel) on hand at all times.
- Work with your healthcare provider to adjust medications to minimize hypoglycemia risk.
Mental Health Support
- Consider therapy or counseling, especially cognitive behavioral therapy (CBT), which has proven benefits for both anxiety and diabetes self-management.
- Practice stress reduction techniques: mindfulness, deep breathing, meditation, or yoga.
- Develop a strong support system: family, friends, or diabetes peer groups.
- Share your anxiety and fears with your diabetes care team.
Lifestyle and Practical Steps
- Avoid skipping meals and always carry a snack, especially during travel or exercise.
- Take note of symptom patterns and keep a diary tracking blood sugar and anxiety symptoms.
- Limit alcohol, which increases risk of hypoglycemia.
- Communicate openly with your employer, school, or colleagues to ensure you have time and access to manage your condition.
Frequently Asked Questions (FAQs)
Can low blood sugar trigger a panic attack?
Yes. Hypoglycemia can cause the body to release stress hormones like adrenaline and cortisol. This can result in symptoms similar to, or even trigger, a panic attack—including rapid heartbeat, sweating, shaking, and a sense of impending doom.
How can I quickly relieve symptoms if I’m unsure whether it’s anxiety or hypoglycemia?
Check your blood sugar immediately. If it’s low (<70 mg/dL), follow the 15-15 rule: consume 15 grams of fast-acting carbs, wait 15 minutes, and recheck. If blood sugar is normal or symptoms persist after treating hypoglycemia, consider using anxiety management techniques, such as deep breathing or grounding exercises.
Is it possible to have both diabetes-related hypoglycemia and an anxiety disorder?
Absolutely. Many people with diabetes experience anxiety, and both conditions can interact in complex ways. Hypoglycemia can cause symptoms of anxiety, but generalized anxiety disorder is a separate medical diagnosis and may require treatment apart from blood sugar management.
What long-term steps can reduce the risk of both anxiety and low blood sugar?
- Consistently check blood sugar and adjust medication if needed.
- Eat balanced meals and avoid long fasting periods.
- Seek professional help for anxiety, such as counseling or therapy.
- Engage in regular physical activity, but monitor your glucose before, during, and after.
When should I seek immediate medical help?
- If you cannot raise your blood sugar with food or drink.
- If you experience seizures, loss of consciousness, or confusion.
- If anxiety or panic attacks are interfering seriously with your daily life.
Takeaway
The relationship between anxiety and hypoglycemia is complex, especially for people with diabetes. Understanding both the physical and psychological triggers, learning to differentiate symptoms, and implementing targeted management strategies can help you regain a sense of safety, comfort, and control over both your blood sugar and emotional wellbeing.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4963565/
- https://diabetesjournals.org/diabetes/article/74/Supplement_1/220-OR/159194/220-OR-Associations-between-Depression-Anxiety
- https://www.webmd.com/diabetes/low-blood-sugar-anxiety-link
- https://www.vcuhealth.org/news/do-you-have-anxiety-or-low-blood-sugar-it-could-be-both/
- https://texasdiabetes.com/is-it-low-blood-sugar-or-anxiety/
- https://sph.umich.edu/pursuit/2019posts/mood-blood-sugar-kujawski.html
Read full bio of Sneha Tete












